Dental diseases include not only inflammatory processes occurring directly in the tooth, but also damage to the tissues surrounding the tooth - bone, periosteum or ligamentous apparatus. And basically all damage to surrounding tissues leads to tooth loss.
Inflammation of the periosteum
Periosteum is the lining or connective tissue between the bone tissue and the tooth. Periostitis is an inflammation of the periosteum; this disease is also commonly called “flux”. Periostitis is very easy to detect - a lump appears on the gum, usually filled with pus. Flux is a very serious disease that requires surgical intervention, but in no case self-medication.
The reasons for the appearance of flux can be various injuries that caused hematoma of internal tissues, as well as advanced caries or incomplete dental treatment. For example, the cause of gumboil can be pulpitis, the treatment of which the patient abandoned halfway through. If the doctor did not remove the nerve, but applied, for example, arsenic or a drug, you should definitely visit the dentist again to remove the temporary filling and install a permanent one, otherwise the nerve may begin to become inflamed and even rot, which will invariably lead to inflammation of the periosteum or bone tissue.
Don't suffer toothache! Come visit us today!
Complex treatment of caries - 6500 rub. for all! Flux treatment, full complex - 6500 RUR!
Periostitis: symptoms
- pain in the gum area
- the appearance of a lump on the gum
- increase in body temperature
- cheek tumor
Periostitis: treatment
- mandatory removal of carious cavity
- treatment or removal of an inflamed tooth nerve
- root canal treatment
- removal of a purulent source of inflammation (usually by a surgical method, which involves cutting the gums and releasing pus out)
- filling and prosthetics of damaged teeth
- drug therapy is used simultaneously with dental treatment
In case of flux, you should never treat yourself! The formation of pus indicates a serious inflammatory process. With self-medication, the purulent focus can increase and spread throughout the body. Traditional methods are used only to relieve pain and facilitate the treatment process, but nothing more.
Inflammation of bone tissue
Following the periosteum is bone tissue, in which the tooth root is securely fixed. Inflammation of bone tissue is always a very serious disease that leads to the destruction of hard bone and, accordingly, tooth loss. Periodontitis is an inflammation of the bone tissue surrounding the tooth. With periodontitis, the tooth is not alive, since the bacteria first attack the root and nerve of the tooth, and only then spread to the bone tissue.
The main causes of periodontitis include dental trauma, as well as acute caries or pulpitis, in which the nerve of the tooth dies.
Periodontitis: symptoms
- sharp pain
- the presence of carious cavities on the tooth
- bad breath
- tooth mobility
- fistulas on the gums (in the most severe stages)
What is osteitis of the jaw?
Osteitis of the jaw is an inflammatory process that occurs in the jaw bone tissue and spreads beyond the periodontium of one of the teeth to the spongy substance of the bones. This is a dental disease that develops along the neurovascular bundle, as well as through contact. It is often accompanied by periostitis (inflammation of the periosteum), less often osteomyelitis (inflammation of the bone marrow with the formation of fistulas, abscesses, and phlegmon).
Osteitis can be acute or chronic. Acute is characterized by destruction of dental bone tissue, and chronic develops in the presence of a chronic focus of infection in the periodontium of the tooth, followed by proliferation, when cells cannot perform a protective function, and the infection spreads deeply.
Tooth structure
A tooth is an organ located in the alveoli of the jaws. A tooth consists of a crown part, a root and a neck connecting the crown to the root. According to the morphological composition, the tooth is divided into hard and soft tissues. Enamel covers the coronal, that is, visible, part of the tooth. It is the hardest element in the human body. Under the enamel is the bone tissue of the tooth, or, as it is also called, dentin, which has a soft and porous structure. The root under the gum is covered with a shell of cement, and in the cavity of the tooth there is pulp, soft tissue consisting of blood vessels and nerve fibers. They penetrate the porous structure of dentin, reaching the beginning of the enamel. This explains the high sensitivity during sudden temperature changes in the oral cavity, as well as when interacting with other unfavorable factors.
Main symptoms of jaw inflammation
There are symptoms of osteitis that occur at the beginning of inflammation in bone tissue. This:
- sudden pain that occurs in the affected area of the jaw;
- swelling (hyperemia) of the sore spot;
- difficulty chewing food;
- spread of pain throughout the entire oral cavity.
If the source of infection is a sore tooth, then difficulty occurs when opening the mouth. If the disease develops rapidly, an increase in body temperature is possible.
With further development of osteitis, the inflammatory process is accompanied by suppuration in the affected area. The general condition of the patient depends on the associated secondary damage surrounding the bone tissue (periostitis, abscess, phlegmon).
Osteomyelitis of the jaw - symptoms and treatment
Treatment is carried out only in a hospital under the supervision of a physician and can be medicinal and surgical [9]. Individually, these methods are ineffective and can even harm the patient. Treatment regimens depend on the stage of the disease.
Treatment of acute and subacute osteomyelitis
At the first visit, the neglected damaged tooth is urgently removed. Then the oral cavity is thoroughly washed with antibiotics. This must be done to remove germs and pus from the wound.
In the following days, the wound is treated with disinfectants and injections of antimicrobial drugs are administered. With their help, it is possible to act directly on the source of infection and prevent it from spreading. In addition to the main treatment, nutritional compositions with vitamins C and B are used.
At the subacute stage of the disease, it is important to contain the spread of infection and prevent inflammation from spreading to surrounding tissues.
For this use:
- IVs with antibiotics;
- drugs that reduce or suppress inflammation;
- rubber drainage for exudate drainage.
Vitamin complexes and preparations are also introduced into the bloodstream to cleanse the body of microbes and their waste products. Specific medications and dosages are selected by the attending physician.
Physiotherapy methods can be additional therapy after the main treatment: UHF therapy or treatment with non-constant currents. They are believed to speed up the healing process [7][16].
Treatment of chronic osteomyelitis
If necrotic cavities appear with decay of the bone and surrounding tissue, surgery will be required. To do this, the damaged area is dissected, the affected areas are removed and a splint is applied. Subsequently, using x-ray methods, the doctor monitors how the bone tissue is restored [11].
To help the body fight infection, additional antibiotics are taken in tablets. Metronidazole is most often prescribed and its effect is enhanced by drugs from the group of 3-4th generation cephalosporins.
If the patient's condition does not improve, then fluoroquinolones or Rifampicin are added. The main task of antibiotics is to prevent bacteria from multiplying [7]. Medicines help reduce inflammation and keep the pathological process within the affected area.
Also, the oral cavity is treated daily with bactericidal agents, droppers with vitamins and plasma-substituting fluids are used, which cleanse the body of toxins.
Additionally, it is recommended to rinse your mouth with infusions of chamomile, St. John's wort, mint and comfrey. Herbal remedies reduce inflammation, speed up recovery and have virtually no side effects.
Treatment methods for osteitis of the jaw
Patients who suffer from inflammation of the jaw require complex treatment for osteitis. It includes surgery, as well as taking antibacterial drugs and special immunostimulating agents. If the teeth located in the area of tissue inflammation are severely destroyed and are a constant source of infection and inflammatory processes, then they must be removed.
If there is a general infectious disease that has caused inflammation of the bone tissue (tuberculosis, syphilis), treatment begins with its elimination. In other cases, the doctor drains the inflammation of the jaw through the root canal of the teeth. Physiotherapeutic treatment of the oral cavity is also carried out. Sometimes they resort to laser irradiation on the area affected by osteitis.
If you have the slightest suspicion of inflammation of the bone tissue in the oral cavity, you should immediately contact your dentist. If you start treating osteitis at the initial stage, it will not lead to serious complications and will not cause severe pain. After successful treatment, you should strictly adhere to the doctor’s prescriptions, carefully care for your mouth and teeth in order to prevent relapses of the disease and the transition of osteitis to a chronic form.
Examples of work “Before” and “After”
Metal-ceramic crowns and stump inlays
Case: destruction of the anterior teeth (11 and 21).
Restoration of front teeth with ceramic veneers (May 2012)
Case: I went to the clinic with a complaint about the unsightly shape and position of the central incisors on the upper jaw.
Aesthetic restoration of anterior teeth - lumineers
Case: the patient complained about the unsatisfactory aesthetics of his smile (he was not satisfied with the color and shape of the teeth), since the teeth were not affected by caries, the curvature was small, the patient chose the most non-traumatic restoration option - installing lumineers without grinding and depulping the teeth.
Treatment of tooth root resorption
The doctor chooses a technique in each specific case, taking into account the complexity and characteristics of the patient’s body. The dentist may resort to cleaning the canals and sealing them. When the process is advanced, when irreversible resorption of tooth roots is observed, removal of the unit followed by prosthetics or implantation is indicated.
In the early stages of small lesions, the surgeon removes the infected areas by making an incision in the gum.
If the cause is a tumor or an improperly growing adjacent tooth, then the tumor is removed surgically; the interfering or pathological unit (the choice is made by the doctor depending on the indications) is in most cases removed.
Symptoms and course
Unfortunately, the disease can occur without any symptoms for a long time. The patient does not experience pain, so he consults a doctor only when the infection has penetrated deep into the bone.
Signs of jaw necrosis:
- pain in an infected tooth or in the socket of an extracted one;
- loosening of teeth;
- swelling so severe that it disrupts the symmetry of the face;
- purulent discharge from the gums;
- putrid odor from the mouth;
- pain when swallowing, chewing, talking.
The main symptom of osteonecrosis of the jaw is bone exposure
.
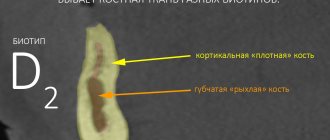
Bone atrophy - what is it?
Bone atrophy is the process of a gradual decrease in the hard tissue of the jaw bone, while the size of the alveolar ridge is significantly reduced, pronounced nasolabial folds appear, the jaw decreases in size, and a “drooping” of the face occurs. Bone resorption (loss) occurs most often after surgical removal of the root, but a person can be born with this pathology.
Clinical case: a person’s tooth and root were removed a long time ago, and an implant and prosthesis were not installed in their place. Over the course of a year, bone tissue atrophies by approximately 25%.
Dentistry for those who love to smile
+7
Make an appointment
Causes of occurrence.
The periosteum is a thin vascular tissue that consists of many nerve endings that completely cover the jaw bone. It securely connects the teeth together with the muscles and ligaments in the oral cavity. If the gum is damaged and an infection gets into it, inflammatory processes begin in the periosteum, the mucous membrane swells, and the person experiences pain. Many patients consider gumboil to be a temporary problem and try to get rid of it using folk remedies. Such an attitude and untimely professional treatment can cause an abscess in the periosteum area. Also, pathology occurs due to difficulty in the eruption of “eights”, i.e. wisdom teeth or as a result of a growing cyst. In addition to these factors, there are several other causes of periostitis:
- Complications of caries.
- Poor oral hygiene.
- Poor quality treatment and improper canal filling.
- Mechanical injuries of the jaw.
- Diseases (sinusitis, sore throat), due to which the infection penetrates the gum tissue through the circulatory system.
- Mistakes during tooth extraction.
Why does bone atrophy occur?
Let us list the main causes of the atrophic process of bone:
- Diseases of teeth and gums. These include periostitis, periodontitis, osteomyelitis, periodontal disease, cysts in the maxillary sinuses, as well as roots, etc. Any inflammatory phenomena in the jaw bone provoke its gradual atrophy;
- No implantation or prosthetics. For example, a patient has had a tooth removed or it has fallen out on its own, and the person is in no hurry to restore the lost dental unit. All this time, the bone tissue atrophies, and other changes also occur: the chewing load is incorrectly distributed due to lack of support and incorrect pressure, the dentition is deformed, etc.
- Advanced age. Unfortunately, in people aged 50+, bone tissue becomes looser, and osteoporosis often occurs. The structure of the bone is disrupted, its density decreases, and its mass decreases. The problem of osteoporosis becomes aggravated if a person is diagnosed with diseases of the heart and blood vessels, central nervous system, thyroid gland, stomach and intestines, etc.
- Congenital abnormalities of the jaw and teeth. It often happens that a person is already prone to bone atrophy from birth. The pathology is accompanied by a reduced jaw size, its underdevelopment and other visible defects that form complexes in people over the years. All these points can be corrected by orthodontic treatment or plastic surgery;
- Congenital abnormalities of the jaw and teeth. It often happens that a person is already prone to bone atrophy from birth. The pathology is accompanied by a reduced jaw size, its underdevelopment and other visible defects that form complexes in people over the years. All these points can be corrected by orthodontic treatment or plastic surgery;
Prevention
To reduce the risk of developing the disease, you should follow simple recommendations:
- Brush your teeth at least 2 times a day. It is advisable not to use hard brushes to avoid injury to the gums.
- After eating, rinse your mouth with warm, clean water or a special mouthwash.
- Use toothpicks less often.
- Visit your dentist regularly.
- Remove tartar twice a year and undergo professional cleaning.
- Get rid of bad habits. Alcohol and smoking greatly impair dental health.
Periodontitis is one of the most common dental diseases. If you take good care of your teeth and maintain oral hygiene, you can significantly reduce the likelihood of its occurrence.
Back
Types of dental periodontitis
Based on localization, the disease is divided into the following types:
- Regional periodontitis. In this case, tissue damage occurs near the edge of the gums. Often occurs due to injury.
- Apical periodontitis. The tissues are affected near the apical part of the root or at the base. In some cases, it is misdiagnosed as pulpitis.
According to stage, the disease is divided into:
- acute form;
- chronic form.
Acute periodontitis
May be purulent or serous. The first type is especially dangerous, as it can lead to the destruction of periodontal tissue. As a result, the teeth become mobile.
Chronic periodontitis
The chronic form is divided into granulomatous, granulating and fibrous periodontitis. The first two types are the most dangerous, as they are accompanied by pronounced bone resorption.
What is dental periodontitis?
Periodontal inflammation is the stage of infection spreading from a carious tooth. It follows pulpitis. The source of infection is located at the apex of the root. This is a small cavity that, in advanced cases, can be filled with pus.
As the disease develops, a cavity appears around the roots. It will open sooner or later. If the disease becomes chronic, it is accompanied by constant suppuration and outflow of pus through a fistula - ducts in which the walls do not fuse.
Treatment of the disease
The therapeutic regimen is always selected on an individual basis. If the disease has recently developed, it is usually possible to manage with conservative methods. The patient is prescribed:
- anti-inflammatory;
- antibiotics;
- antiseptics.
Sanitation of the oral cavity is mandatory. If there are indications for removing destroyed units, they are pulled out and replaced with dental prostheses. Physiotherapy helps speed up the healing process.
In advanced cases, surgical treatment is performed. In this case, the treatment plan looks something like this:
- The doctor examines the condition of the mouth and determines the cause of the disease.
- A local anesthetic is injected into the affected area. As soon as it takes effect, an incision is made in the gum with the abscess.
- The opened lesion is cleaned of purulent exudate and washed. If necessary, install a drainage tube. It is necessary so that necrotic masses do not again begin to accumulate in the existing cavity.
- The doctor treats the tooth, if it is possible to save it. Fills the canals and installs a seal. If the unit cannot be cured because the roots are severely damaged, removal is carried out.
- The patient is prescribed antibiotics, painkillers, and anti-inflammatory drugs.
It is important that after treatment the patient comes for follow-up examinations. They are needed to prevent relapse of pathology and create optimal conditions for rapid regeneration.
Content:
- What is periosteum
- Signs of the disease
- Diagnostic measures
- Classification
- Treatment of the disease
- Prevention
Some dental diseases lead to severe inflammation due to untimely treatment.
As a result, periosteal tissue is included in the pathological process. If qualified dental care is not received at this stage of the disease, osteomyelitis or other dangerous pathologies may develop. Inflammation of the periosteum of the tooth should not be allowed. It is difficult to treat and may require surgery.