Every person changes their milk teeth to molars. At 6-7 years old, the first incisor falls out, and tooth replacement ends after 20, when “eights” appear. New teeth grow according to an individual schedule, so the parent’s task is to teach the child to properly care for the oral cavity and monitor how the children’s molars grow.
When does a child's molars come out?
Growing permanent teeth is a big job for the body, which we rarely notice. Changes begin at 3 years - the rudiments of molars are formed. At age 5, noticeable gaps appear between the baby teeth to make room for new “tenants.”
Which teeth come out first is determined by a lottery - genetics. In half of the cases, growth begins with “sixes”. Molars grow by the age of 7-8 years, at the same time the front incisors change.
Teeth grow slowly but painlessly. At 14, the main bite is already formed. “Late” wisdom teeth - third molars grow in a few years, at 18-21 in most adults.
Anatomy of permanent teeth
The molar tooth includes three zones: the root, which sits deep in the jaw socket and holds the tooth in place, the neck, located in the periodontal area, and the crown, which extends directly into the oral cavity. After the apex of the tooth appears, a protective film forms on the enamel, the strongest layer of the tooth, which is soon replaced by a salivary layer, formed from the saliva itself. The dental tissues themselves are not just a piece of bone, but a certain heterogeneity, which includes, in addition to enamel, dentin (the main substance of the tooth) and the dental cavity, in which nerves and blood vessels branch. Compared to bones, for example, the phalanges of the fingers, dentin is noticeably stronger - it contains an increased amount of minerals, for example, the same calcium-based compounds. The root zone of dentin is connected to the periodontium using a special layer - dental cement, which communicates with the tissues of the periodontium itself and supplies the dentin with nutrients.
Molars in children: symptoms of eruption
In almost all children, molars appear painlessly and unnoticeably. However, there are exceptions when the growth of permanent teeth is accompanied by unpleasant sensations. A common symptom when teething is increased temperature, up to 38 ºС. The child also complains of:
- weakness and drowsiness due to decreased immunity;
- runny nose, excessive salivation;
- inflammation of the gums;
- itching, pain while eating.
Massaging your gums will help relieve discomfort in your mouth. To relieve inflammation, use dental gel. Important: Disinfect your hands or wear sterile gloves before applying.
Consult your dentist before purchasing medications. Severe inflammation is a signal that teeth are not growing properly. Without treatment, the child's bite may become deformed.
Complications during teething
- bite defects. Molars are larger in size than baby teeth; there may not be enough space in a narrow jaw. The bite changes if the baby teeth do not fall out, but new ones begin to grow.
- hyperdentia – teeth grow in a second row. This happens for various reasons, most often - the baby tooth holds tightly and the root one looks for other ways.
- teeth don't grow. If the milk one falls out, but the permanent one is delayed for six months, you need to consult a doctor. Poor dental growth is one of the signs of problems with the immune system in children.
- caries and pulpitis. The first sign of enamel destruction is the child’s complaints of a sore throat, sweet and hot foods “getting” into the tooth. If pulpitis affects the molars, children’s body temperature rises and severe pain appears. Then treatment of pulpitis is urgently needed without delay.
Teething disorders - symptoms and treatment
In case of teething problems, symptomatic treatment is carried out. Its purpose is to eliminate pericoronitis, oral abscess and osteomyelitis.
Treatment of pericoronitis
Treatment of pericoronitis is carried out on an outpatient basis. If the tooth germ is positioned correctly and there is enough space for the dental arch, then surgical treatment is the most preferable option. The mucous membrane in the area of the tooth crown is completely excised. As a result, access to the chewing and lateral surfaces of the crown appears. The operation is performed under anesthesia and can be performed either with scissors or a scalpel, or with more modern methods: cryodestruction, laser and electric knife.
pericoronarotomy can be performed - an operation during which the mucous membrane above the tooth crown is dissected. As a result, tooth surfaces that were previously covered by a hood of mucous membrane are exposed.
After surgical treatment, drug therapy :
- Antibacterial agents are selected individually, taking into account the microflora. It can be:
- Inhibitor-protected penicillins that destroy anaerobic and aerobic microorganisms. Amoxicillin with clavulanic acid is most effective.
- Lincomycin and Clindamycin act against Staphylococcus aureus.
- Metronidazole is not effective against facultative anaerobes and aerobes, but together with other antibiotics it will help cope with mixed microflora.
- Cephalosporins act only together with Metronidazole and Clindamycin, since almost all anaerobic microorganisms are insensitive to them.
- The latest generations of fluoroquinolones are effective against gram-positive bacteria, but each drug has its own level of activity.
- Non-steroidal anti-inflammatory drugs.
- Antihistamines [10].
- Detoxification therapy consists of drinking plenty of warm drinks rich in vitamins, such as compotes and fruit drinks. Sometimes in difficult situations, an isotonic solution is administered intravenously.
To alleviate local symptoms and reduce inflammation, baths with antiseptic solutions are used: a pale pink solution of potassium permanganate, 0.01% Miramistin solution or 0.05% Chlorhexidine.
Treatment of oral abscess
Treatment for an oral abscess includes surgery and medication. Depending on the location of the abscess and the general condition of the patient, it can be performed in a clinic or in a hospital. During the operation, the purulent-inflammatory focus is opened, the postoperative wound is treated with antiseptics and drained.
After surgery, medications must be prescribed. They are similar to those used to treat pericoronitis. To detoxify, it is recommended to drink plenty of alkaline liquids, such as mineral water and cranberry juice.
For several days after the operation, the wound is bandaged daily and treated with antiseptics.
Treatment of osteomyelitis
If osteomyelitis is detected, the patient is immediately hospitalized. The erupting tooth is removed, and all purulent foci are carefully treated. Antibacterial drugs are administered intravenously. For detoxification, saline solutions are used, which are also administered intravenously.
Recommendations for caring for a child's molars
Children's molars require careful care. Young enamel is sensitive to the external environment and bacteria that cause caries. Therefore, it is important to use hygiene products.
The best prevention is to teach your child to maintain good oral hygiene before a permanent bite has formed. To keep your teeth healthy, you need to follow a few simple steps:
- brush your teeth every day ☑️. Brush at least twice a day, use dental floss and mouthwash.
- correct diet ☑️. Sweet plaque on teeth is the best food for bacteria. After meals with a lot of carbohydrates, brush your teeth or rinse your mouth. Avoid snacking when you can't take care of your teeth.
- regular preventive examinations ☑️. You need to visit the dentist once every six months. Treat teeth immediately when problems are detected.
- strengthen teeth ☑️. Eat a balanced diet, take vitamin and mineral complexes rich in calcium.
- Visit the dentist regularly ☑️ and have your teeth professionally cleaned.
Taking care of your teeth doesn't take much time, but taking simple steps now will help you maintain beautiful, healthy teeth for life.
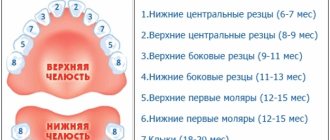
After a year, teeth appear with the following frequency:
- by 12-15 months – two pairs of first molars erupt;
- by 18-20 months – a pair of upper and a pair of lower canines are already clearly visible;
- 20-30 months is the period of appearance of two pairs of second molars.
How many teeth should a child have at 1 year 3 months? Ideally 12, but the number can change in one direction or the other, and this is not considered a deviation. The frequency of teething is influenced by many factors, including previous infections, heredity, climate, and health status.
The question of how many teeth a child should have at 1 year 8 months, or 20 months, also cannot be answered unambiguously. The answer will be approximate - about 16. Up to a year, parents should focus on the approximate formula: the number of months minus 4, with a reservation for the baby’s characteristics.
Where do teeth come from?
Teeth are formed in the fetus’s body during the mother’s pregnancy. When a mother abused something and undermined her own health, the subsequently born child was guaranteed to have diseased teeth that were no longer permanent. At the 15th week of pregnancy, the mother has hardened dental tissues in the fetus - starting from the crown area and ending with the root zone. The embryos of molar teeth are formed by the 5th month of fetal life. The body of a developing fetus and child is designed in such a way that in the upper jaw the anlage of the permanent teeth is located above the anlage of the milk teeth, and in the lower jaw - vice versa. The formation and development of teeth begins as early as the sixth week of fetal development. The source for them is a special epithelial dental plate. Already by 14 weeks of pregnancy, the unborn baby is actively forming hard dental tissues, initially in the area of the coronal part, and then in the area of the roots of the tooth. When a child is born, primary teeth are the first to grow - by the end of the child's first year of life, they will erupt. However, the dentition contains a group of large molars - they, in turn, do not have milk predecessors and subsequently, when they fall out, grow “on a permanent basis”. Nature has arranged it in such a way that while the child’s jaws are still too small, large molars are not needed there.
What to do when teeth grow in two rows
With “shark” jaws, the most reasonable solution seems to be the removal of excess milk units. And they did this for a long time. The result of hasty decisions showed that hasty removal of primary incisors and fangs leads to the opposite result and the formation of a malocclusion. After this, pediatric dental surgeons began to see children only as prescribed by the orthodontist - after professional consultation with a specialist.
An orthodontist is the first doctor you should go to when teeth grow in two rows. The doctor will assess the prospects for the formation of the dentition, send you for an x-ray to accurately determine the rudiments of permanent teeth and make the right decision. And this will not always be immediate removal of a baby tooth!
Based on the results of the diagnosis and examination, the orthodontist can advise:
- increase the amount of solid food in the child’s menu - provide the missing pressure on the baby tooth, causing it to loosen and fall out;
- wait for the natural change of teeth so that the permanent unit moves into its intended place under the influence of other teeth and under the pressure of the tongue muscles;
- remove primary incisors and canines to forcefully free up space.
The latter purpose is typical for parallel growing teeth and firmly standing primary units, since this is the only case when there are no natural prerequisites for root resorption and normal bite changes.
Differences between baby teeth and permanent teeth
The structure of primary and permanent teeth is generally the same, but there are several noticeable differences. Which are better not to neglect:
Baby teeth have whiter enamel, while permanent teeth have a slight yellowish tint. Milk teeth are not as strong as permanent teeth due to the lower percentage of mineral substances. The pulp of baby teeth is wider and thicker, while dentin and enamel are, on the contrary, thinner. This explains the facilitated, spontaneous removal of a shelf tooth - there are often situations when schoolchildren in class independently loosen and remove milk teeth that have served their purpose. In permanent teeth, the length is significantly greater, dominating over their width and cross-sectional area. The root of a baby tooth is thinner and shorter - a person is able to pull out a baby tooth without the help of specialists. Meanwhile, the permanent “embryo” of a real tooth under the shelf one is already ready to grow quickly and be born. The latter is achieved due to the dental gap, which has expanded by the time the non-permanent tooth falls out.