In this material we will try to discuss how to prepare for wisdom tooth removal, basic recommendations, what is and is not possible before wisdom tooth removal, the postoperative period and possible consequences.
All this will help you prepare mentally and make it easier to endure the operation itself.
- When is it better to delete
- What you can do before tooth extraction
- What not to do before tooth extraction
- Recommendation before tooth extraction
- Recommendations after tooth extraction
- Postoperative period and possible consequences
Remember, you are the one who makes the decision to preserve or remove a tooth; if you don’t understand something, ask questions and don’t be shy with the doctors, because you are also responsible for the decision.
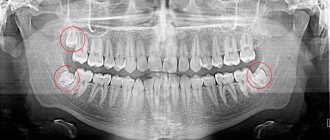
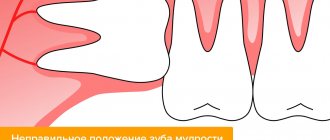
When is the best time to remove a wisdom tooth?
It is better to remove a wisdom tooth when it does not hurt!
Are you faced with the fact that the doctor recommended that you remove a wisdom tooth on the upper or lower jaw? Most likely there are certain indications for this.
Any surgical intervention during a period of acute inflammatory process occurs and is tolerated more difficult than during a period of relative rest. The healing period in such cases is more painful and longer.
Therefore, do not wait until the tooth hurts (IT WILL DEFINITELY HURT).
If you doubt or don’t trust a doctor, consult another one; if you have doubts, consult a third one.
Features of papillomas
Papillomas can be of the following types: ordinary or vulgar warts, filiform (the most common type), flat, genital warts, plantar warts, juvenile warts. A dermatologist diagnoses and treats papillomas.
Most often, papillomas are localized in the armpits and inguinal folds, hands, on the surface of the foot, neck, under the mammary glands in women, as well as on the genitals. Papillomas located on the mucous membranes of internal organs are very dangerous; they can cause ulceration or bleeding. As a rule, papillomas that have a pronounced cosmetic defect are removed with a laser, i.e. which are located in open areas of the body, as well as those with a high risk of cancer.
Recommendations before wisdom tooth removal
It is better to remove wisdom teeth in the morning
The body is full of vital energy in the morning and easily experiences stress. Believe me, even just a visit to the dentist is stressful for some people. After the removal of the eighth teeth (wisdom teeth), pain may appear, which will go away after a few hours. If the operation takes place in the morning, then by the evening the pain will completely disappear and you will go to bed peacefully. In the morning, not only are you full of strength and energy, but so is your doctor. The doctor is not tired yet and is ready to devote maximum concentration of attention and time to the procedure. In case of any complications, you can easily go to the clinic, rather than looking for a 24-hour clinic with sleepy doctors at night or going to an ambulance.
Eat before wisdom tooth removal
(if you are not planning on sedation or general anesthesia) A well-fed person can tolerate stressful situations much easier. After eating, the body releases hormones that help you relax. Concentration decreases a little and you don’t really think about the procedures performed by the dental surgeon. More busy digesting food. A well-fed person's blood clots better than a hungry person's. This can greatly help to avoid unpleasant complications in the postoperative period.
It is strictly forbidden to drink alcohol before and after wisdom teeth removal
Alcohol can greatly change the rheological properties of the blood, which in turn can lead to significant swelling or prolonged bleeding with a risk to life. A person in a state of alcoholic intoxication is not attentive and cannot soberly assess the situation and make decisions. Plus, I’m not able to accurately remember the doctor’s recommendations; all this will lead to unpleasant complications.
What to take before wisdom tooth removal
Before the operation, the doctor will definitely inform you about all the medications that need to be taken before the operation. If you are very worried, you can use mild sedatives - valerian tincture, motherwort tincture, etc. Or the same drugs only in tablet form, for example Tenoten. If a long-term surgical intervention is planned, for example, removal of a retained or dystopic wisdom tooth, or tooth-preserving operations, or tooth implantation, it is reasonable to use non-steroidal anti-inflammatory drugs with a pronounced anti-inflammatory or analgesic effect, antibiotics, and antihistamines. It is better to entrust the choice to your treating dental surgeon about which drug to take.
A good mood is the key to successful treatment
Remember that a good positive attitude will shorten the recovery period and help you overcome surgical procedures more easily.
Anesthesia or pain relief
Local anesthesia is almost universally used in dentistry. All modern anesthetic drugs are non-toxic and hypoallergenic, provided they are selected correctly. Anesthetics used in private dental clinics are absolutely safe. Modern anesthetics can provide complete absence of sensation in the oral cavity for a long time, up to 5 hours. Thereby making the patient’s stay in dentistry comfortable. As an example, many patients fall asleep during dental appointments thanks to good anesthesia. “Anesthesia doesn’t take me away” - every dentist has heard this. The anesthetic affects all people the same. If the anesthesia has no effect (does not take effect) on you, then the doctor does not have the proper skills in administering anesthesia. It is not possible to become infected with infectious diseases during the administration of anesthesia. In private dental clinics, a special carpule syringe system is used, which completely eliminates contact of the solution and needle with the environment and even with the syringe itself. Anesthetics, if chosen correctly, do not affect the fetus during pregnancy and do not affect the composition of breast milk in nursing mothers. The quality of anesthesia can be affected by long-term use of non-steroidal anti-inflammatory drugs with a pronounced analgesic effect (painkillers), narcotics. Anesthetics are not addictive.
How to behave during the removal process
There are a lot of removal techniques and the choice of technique directly depends on the tooth and the situation in the oral cavity. In addition to the tooth extraction itself, the doctor must also ensure a comfortable stay during the process. Do not hesitate to talk about your unusual sensations, this may help the surgeon during the operation. Do not endure the pain, in modern dentistry there is a sufficient amount of anesthetics and, if necessary, the doctor will add anesthesia. During the removal process, you may feel pressure or crunching. The doctor will warn you about this in advance. The removal time depends on the qualifications of the surgeon and the initial situation, on average 15-30 minutes. The hole in the tooth was sewn up. Yes, this happens too. Based on our practice, almost any tooth extraction requires subsequent suturing of the hole, especially when it comes to further implantation in this area. Healing time is reduced and the postoperative period is easier to bear. If you or the doctor have any doubts about whether there is a piece of tooth left there, do not hesitate to ask the doctor a question or take a control X-ray. A gauze swab is not always placed as prescribed by a doctor.
Diagnosis of cataracts
Modern equipment makes it possible to detect disturbances in the structure of the lens even at the initial stages of cataract development. Also, the patient himself should notice characteristic signs - narrowing of the visual field, loss of light sensitivity, visual clouding of the intraocular media, interfering with good vision. Cataracts most often develop in older people, along with other pathologies of the visual tract, especially presbyopia, a natural age-related farsightedness.
The main method for diagnosing cataracts is biomicroscopy, which involves examining the ocular media at multiple magnification under a special slit lamp. Such an examination allows you to determine the size and degree of cataracts, make predictions regarding the speed of spread of the process and the urgency of the operation.
It is also important to determine the degree of visual acuity, the preservation of the peripheral vision field, and to examine the fundus of the eye for changes in the neurovascular structures of the eye. An appointment with an ophthalmologist after 40 years of age must be accompanied by tonometry - measuring intraocular pressure to diagnose glaucoma.
Optical coherence tomography is a method for accurately determining the state of preservation of intraocular structures. Next, modeling and selection of a suitable intraocular lens are used.
Recommendations after wisdom tooth removal
- Behind the wheel. You should drive with caution if you have had a complex removal of a wisdom tooth, for example. Stress can lead to loss of alertness. It is not uncommon for patients to fall asleep while driving after a visit to the dentist.
- In case of a complex operation, if necessary, arrange for support in advance.
- Ask your dental surgeon for your mobile phone number and clinic number for emergency contact with your doctor. It is always faster to receive first-hand information if something bothers you after the operation or you simply have a question.
- Avoid smoking and drinking alcohol for the first days after tooth extraction. Both have a negative effect on healing. Smoking causes burns to the mucous membrane and disintegration of the blood clot
- Do not drink for about 2 hours after removal, until the blood clot fills the socket and attaches there.
- Do not eat until the anesthesia wears off. Otherwise, during the chewing process, you can damage healthy tissues that, under anesthesia, are not sensitive to injury.
- Eliminate coarse, spicy, salty, hot foods from the diet. This food negatively affects healing and can also cause discomfort at the site of tooth extraction and even pain.
- Avoid sports and heating the body (bath, sauna, solarium, hot shower) for 3 days. Sports and heat can cause bleeding from the socket of an extracted tooth and serious swelling of the head and neck.
- Gentle treatment of the surgical site. That is, exclude chewing on the side of the operation, do not climb into the hole of the extracted tooth with your tongue. In other words, create peace at the site of tooth extraction.
- It is forbidden to pick or clean the socket of an extracted tooth. Even if you see something unusual, contact your doctor. Self-indulgence can lead to complications that are very long and difficult to treat!
- It is strictly forbidden to rinse your mouth with anything after tooth extraction for 2-3 days.
- Self-medication, warming compresses, and so on are strictly prohibited.
- You can brush your teeth in the first days after tooth extraction; the only rule is to avoid the surgical area. Avoid strong rinsing movements in the mouth for 2-3 days.
- In case of any concerns, deterioration of health, or simply doubts arise. Do not hesitate and contact your doctor or clinic!!!
Remember! In 90% of all complications after tooth extraction, the cause is non-compliance with the doctor’s recommendations.
Full list of tests
1. Clinical blood test (formula) - valid for 1 month. 2. Blood sugar - valid for 1 month. 3. Blood test for clotting or bleeding time - valid for 1 month. 4. The result of the Wasserman reaction, HIV, NVB antigen, ASU antigen - valid for 1 month. 5. Urinalysis (general) - valid for 1 month. 6. Electrocardiogram tape with interpretation - valid for 1 month. 7. Therapist’s conclusion about the absence of contraindications to eye surgery - valid for 1 month. 8. Dentist’s conclusion on oral sanitation - valid for 3 months. 9. An otolaryngologist’s conclusion about the absence of contraindications to eye surgery - valid for 3 months. 10. X-ray of the paranasal sinuses (description) - valid for 3 months. 11. X-ray of the chest organs (description) - valid for 12 months.
For patients with diabetes mellitus additionally:
12. Glycated hemoglobin - valid for 3 months. 13. Determination of urea nitrogen and creatinine in the blood - valid for 1 month. 14. Endocrinologist’s report – valid for 1 month.
Alcohol before surgery - possible consequences
Some patients try to drown out toothache and stress by drinking alcohol. But it is prohibited to drink alcohol before dental procedures.
Reasons for the ban:
1. Ethanol reduces the effectiveness of anesthetics. The doctor will be forced to increase the dose, which can lead to an overdose.
2. Painkillers have a large number of side effects. This is nausea, vomiting, vertigo. Alcoholic drinks increase unpleasant symptoms.
3. Ethanol reduces blood clotting. This is fraught with the development of bleeding during and after surgery.
Alcohol consumption increases the risk of complications. And the dentist may refuse to remove a tooth from an intoxicated patient until he has completely sobered up.
Possible complications if you ignore the ban
The more alcohol the patient took, the higher the risk of complications. Frequent ones are:
- ineffectiveness or increased side effects of anesthetics;
- development of bleeding;
- increased risk of allergies to medications used by the doctor;
- increased blood pressure, hypertensive crisis;
- heart attack;
- increased load on the kidneys, liver and, as a result, inflammatory processes in the biliary and urinary systems;
- long-term healing of the wound surface.
Briefly about the main thing:
I think that scraping or puncture before removing a mole is not necessary, because... The accuracy of diagnosis is only 95%, in contrast to histology (close to 100%).
Instead of scraping or puncture, in my practice I always remove all moles with an indentation of 1 MM and always send them for histological examination (excisional biopsy). If histology shows melanoma, the biopsy site is excised again with an indentation of 1 to 3 CM, which fully complies with safety standards in oncology.
Why examine a mole if it has already been removed? Will it be too late?
A logical question arises - what to do if the histology shows melanoma? Will we do any harm by removing it? Will this lead to tumor progression?
No.
A large number of clinical studies have found that performing an excisional biopsy
does not worsen the course of melanoma.
In other words, the chances of recovery in patients who first underwent such a biopsy, and then wide excision, are the same as those whose melanoma was immediately excised widely.