For many people, as practice shows, panic is caused by the mere fact that it is necessary to remove a wisdom tooth. This is due to the fact that patients imagine the procedure itself as painful. But the days when a dentist spent more than 2-3 hours chiseling out roots piece by piece with a hammer and chisel are long gone.
Modern clinics use new technologies and techniques, thanks to which the removal of a wisdom tooth in the upper jaw is quick, in a comfortable environment and absolutely painless.
Content:
- Peculiarities
- Indications
- Contraindications
- Operation
- Removal methods
- Difficult removal
- Stages
- Diagnostic value
- Does it hurt to remove
- Possible complications
Wisdom teeth or “eight” teeth, located at the edges of the jaw, erupt much later than their counterparts. Moreover, this often happens in adulthood, causing a person many unpleasant moments. The fact is that the structure of the human jaw does not provide enough free space to comfortably accommodate an additional pair of teeth. Therefore, “eights” often put pressure on “sevens”, they grow at an angle, their roots become curved, and it can be difficult to provide them with proper hygienic care, as a result of which caries develops. The peculiarities of the location do not allow for high-quality treatment of the wisdom tooth, and the optimal solution is its removal, since it bears neither a functional nor an aesthetic load.
In what cases is it necessary to remove upper molars?
Dentists recommend removing the upper “eights” for the following indications:
- an impacted wisdom tooth (molar eruption has not yet occurred) is incorrectly positioned in the upper jaw, causing injury to soft tissues and neighboring teeth. In this case, the latter will develop with pathologies and may become displaced or destroyed;
- the crown is severely destroyed due to advanced caries;
- pericoronitis, periodontitis, pulpitis;
- the ternary nerve was pinched;
- cysts were found at the root of the tooth;
- The patient is planning to have braces installed in the future.
X-ray examination plays a very important role in the early diagnosis of problems with extreme molars. X-ray or visiography allows you to timely identify pathologies, solve detected problems and thereby minimize the risk of complications in the future.
Impacted wisdom teeth
A vertical position of an unerupted extreme molar is normal and there is no reason to remove it. But if it is located at an angle or horizontally and does not provide space for the proper development of neighboring teeth, then this is a serious reason for its removal. If this is not done, problems such as:
- trauma to the mucous membrane, which leads to inflammatory processes in the oral cavity;
- deformation or displacement of adjacent molars;
- destruction of the nearby "seven".
Often, an outwardly healthy wisdom tooth turns out to be affected by caries inside, and this can only be detected through radiography.
Advanced caries
Careful hygiene procedures on extreme molars are difficult due to their inconvenient location. As a result, pathogenic microorganisms multiply in hard and soft tissues, inflammation and caries develop. When the wisdom tooth is inclined, gaps appear between adjacent molars (second and third), which increases the area of caries spread.
If the carious lesion is minor, the dentist can put a filling, but this measure is temporary. Therefore, it is recommended to remove the extreme molars if there are pathologies in them. These teeth are not functional and can cause many problems.
High likelihood of developing pericoronitis
As the outer molars begin to erupt, a hood of mucous membrane often forms over them. Due to insufficient oral hygiene (and it is almost impossible in the area of wisdom teeth), food debris accumulates under this hood and begins to rot. Dental plaque forms—first soft, then hard (tartar), and pathogenic microorganisms develop. As a result, pericoronitis may begin - purulent inflammation of the oral mucosa. The disease is accompanied by pain, swelling, difficulty swallowing and unpleasant odor from the mouth.
To avoid complications, timely excision or complete removal of the hood is required.
Trigeminal neuralgia
If the extreme molars are positioned incorrectly, the trigeminal nerve is often pinched. To make sure that the cause of neuralgia is problems with wisdom teeth, an x-ray is required. If suspicions are confirmed, this is a good reason to remove the “eights”.
Detection of a cyst
Unerupted upper outer molars also pose a danger in the form of cysts, which often form at the roots. When diagnosing a cyst, it is necessary to urgently remove the pathological “eights” along with follicular cysts, otherwise complications such as:
- perineuritis;
- purulent sinusitis;
- chronic inflammatory process;
- osteomyelitis;
- fistulas
Features of the structure of wisdom teeth
The structure of a wisdom tooth is no different from other molars and consists of a neck, a root system (4–5 pieces) and a crown. In some cases, root development is disrupted and a single conglomerate is formed, that is, a tooth grows with one root.
Its only difference from its neighbors is that recent studies recognize the wisdom tooth as a rudiment that has lost its functional purpose during the evolutionary development of man. Scientists do not consider it as a full-fledged organ, since some part of humanity does not grow it at all.
However, the wisdom tooth has several parameters that distinguish it from the same “seven”:
- lack of milk precursors, which ultimately complicates eruption and impedes growth. There is no room left for it on the dental arch, which is why various developmental pathologies arise;
- the number of roots is greater than that of other molars - up to 5 pieces. In this regard, problems often arise when removing a wisdom tooth;
- significantly curved roots of the “eights” make cleaning and treatment of root canals very difficult;
- poor blood supply compared to other teeth leads to rapid aging, accompanied by fragility and susceptibility of tissues to caries, despite minimal load;
- many pathological conditions, for example, pathologies of the masticatory muscles, malocclusion, pericoronitis, are associated with the growth of “eights”.
Thus, the appearance of third molars has many more negative consequences than positive ones. Many patients are forced to see a dentist even before they can be seen in person.
Deformations of the dentition
The pressure exerted by the erupting wisdom tooth on the dentition when there is not enough space causes crowding of the teeth in the dentition and the development of malocclusion. Aesthetics and smiles are affected mainly in the anterior region, and oral hygiene becomes difficult.
Growing and expanding wisdom teeth are often the cause of reoccurrence of malocclusion after long-term orthodontic treatment. Therefore, it is strongly recommended to remove wisdom teeth before starting orthodontic treatment!
Indications for wisdom teeth removal can be formulated as follows: ANY DISEASE, COMPLICATION ASSOCIATED WITH WISDOM TEETH, AS WELL AS THE RISK OF THESE DISEASES OR COMPLICATIONS IS A DIRECT INDICATION FOR WISDOM TEETH REMOVAL.
Indications for wisdom tooth removal
Treating third molars is a challenging task, but a competent dentist will try to keep the unit relatively healthy. However, in practice, even relatively healthy “eights” are extremely rare.
Most often, problems begin at the teething stage, which is associated with pain, fever, swelling and other troubles. The doctor prescribes wisdom tooth removal if:
- an unerupted molar is incorrectly positioned in the jaw, injuring neighboring teeth and soft tissues;
- extensive caries damage with significant destruction of the crown;
- pericoronitis (presence of an inflamed hood);
- installation of a bracket system. Sometimes only the removal of a wisdom tooth can ensure the correct movement of other molars;
- presence of a cyst;
- the trigeminal nerve is pinched;
- pulpitis, periodontitis.
Most experts are inclined to believe that the “eight” should be under the supervision of a doctor from the moment of eruption. An x-ray is sufficient to assess the development of the tooth and assess future prospects. This needs to be done immediately, if only because for young people the rehabilitation period is much easier and the likelihood of complications is minimal.
Symptoms of retention
Sometimes tooth impaction is asymptomatic, without causing pain or discomfort, but most often patients with impacted wisdom teeth notice the following symptoms:
- Unpleasant sensations when chewing food;
- Bad breath;
- Swelling of the gums and redness around the impacted tooth;
- pain or tenderness in the gums or jawbone;
- Frequent headaches or jaw pain;
- Difficulty opening the mouth;
- Temperature increase.
If such symptoms appear during the eruption of figure eights, a visit to the doctor is required. This does not mean that the tooth will have to be removed. First, the doctor will examine the oral cavity, take a photo, and only then will a decision be made on the correct treatment.
Contraindications to wisdom tooth removal
Despite all of the above, there are situations when the mouth cannot do without the “eight” or the operation cannot be performed for other reasons:
- you need to install a bridge supported by the third molar;
- adjacent molars become loose, and a wisdom tooth is used as a base for applying a splint;
- due to the absence of chewing molars, the chewing function falls on it;
- period of pregnancy and breastfeeding;
- cardiovascular pathologies;
- impaired blood circulation;
- allergy to anesthetic;
- hypertensive crisis.
Simple wisdom tooth removal method
For a simple operation, the surgeon uses forceps and an elevator without resorting to incisions or drilling into the bone. This method allows you to extract a molar if:
- the upper wisdom tooth needs to be removed;
- there are no significant developmental deviations;
- there are no complicating circumstances.
Wisdom tooth removal proceeds as follows:
- 1. The dentist collects anamnesis, inquires about the patient’s allergic reactions to medications, and selects the optimal anesthesia;
- 2. an anesthetic drug is administered, its effect begins after about 5 minutes;
- 3. the surgeon prepares instruments, the sets of which differ depending on the location of the tooth, its condition, and the presence of inflammation;
- 4. Using forceps or using an elevator, the tooth is removed from the socket;
- 5. The doctor treats a fresh wound with antiseptic drugs;
- 6. If necessary, an anti-inflammatory agent is placed in the hole.
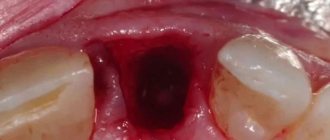
After the removal of wisdom teeth, large sockets remain, so the surgeon sutures the tissue to prevent infection and speed up healing. In the presence of purulent processes and inflammation, suturing the hole is not advisable, since the contents must have an unimpeded outflow. The manipulation usually takes no more than 10 minutes. To monitor the patient’s condition, the doctor schedules an examination a few days after the operation to remove the diseased wisdom tooth.
Experts' opinion
Question: Is local anesthesia sufficient when removing the upper “eight” or is it better to ask for general anesthesia?
Answer : If no serious pathologies are identified in the upper molar during the examination, then the dentist will use a simple method to remove it using local anesthesia. The most commonly used anesthetic drugs are the articaine series, which are highly effective. In order for the effect of anesthesia to be prolonged, norepinephrine or adrenaline is added to it. In this case, the “freezing” will last about an hour, this time is quite enough to remove the upper wisdom tooth and treat the wound. A little pain after the anesthesia wears off is normal. Analgesics prescribed by your doctor will help you cope with it. As for general anesthesia, it is indicated in cases of complications or when the patient’s panic fear of dental procedures prevents the doctor from performing the necessary manipulations.
Question: The upper wisdom tooth still won’t come through. The gums are swollen. Do I need to see a dentist for tooth extraction?
Answer : The extreme molars erupt at a fairly late age and cause a lot of unpleasant sensations: pain, swelling, temperature, etc. If you notice swelling on the gum in the area of a wisdom tooth that has not yet erupted, then you should visit the dentist. He will conduct an examination and order an x-ray examination to determine whether the “figure eight” is positioned correctly and whether it will cause trouble in the future. If necessary, the doctor will make an incision in the gum. If a tooth grows incorrectly, it should be removed as soon as possible.
Complex wisdom tooth removal
During such an operation, the surgeon uses many more instruments and performs more complex manipulations, in particular, cutting soft tissues and suturing the incision without fail.
Complex removal is carried out if:
- we are talking about removing the lower wisdom tooth;
- there is an abnormal root system;
- the coronal part is severely destroyed;
- impacted, dystopic molars.
Preparation for the operation follows approximately the same pattern as for simple wisdom tooth removal, but this is where the similarities end. This is noticeable already at the initial stage: more time is allocated for the effects of anesthesia - about 10 minutes.
Stages of complex wisdom tooth removal
The methodology may differ for each specific case, but in general terms several approximate stages can be outlined:
- 1. local anesthesia;
- 2. incision of soft tissues, peeling them off the bone;
- 3. sawing, drilling out the proper bone tissue;
- 4. extracting the “eight”;
- 5. treatment of a fresh hole left after the removal of a diseased wisdom tooth;
- 6. suturing with non-absorbable suture material;
- 7. The doctor will remove the stitches only after the edges of the wound have completely fused.
The duration of the procedure depends on the situation and can last from 30 minutes to 2 hours. After the operation, the doctor advises the patient regarding wound care, prescribes medications and informs the date of the next appointment.
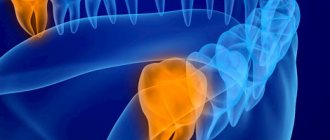
The value of x-ray diagnostics when removing wisdom teeth
No qualified doctor will remove wisdom teeth “blindly”. You cannot rely on external indicators. A clear assessment of the condition of the root system and the development of the tooth is necessary in order to eliminate complications that could arise after the operation. An x-ray must be taken to assess the feasibility of removing a particular wisdom tooth.
X-ray examination provides an informative picture that allows you to see:
- the presence of curved roots;
- number of root shoots;
- structural features.
Based on the results of X-ray diagnostics, the doctor will be able to draw up a surgical plan and eliminate errors in the form of bone fragments remaining in the gum.
Is it painful to remove a wisdom tooth?
Many patients delay wisdom tooth removal due to fear of pain. Such fears in modern dentistry are absolutely groundless, since anesthetics are necessarily used for the procedure. Discomfort occurs when the effect of the drugs wears off and the analgesic effect decreases. But this is a physiological process that fades away on its own after some time. In addition, there is absolutely no need to endure pain; the doctor will prescribe medications to alleviate the postoperative condition.
When removing a wisdom tooth, some patients experience painful symptoms for a number of reasons:
- drug addiction;
- extensive purulent process;
- abuse of painkillers.
Also, the degree of pain depends on the method of removal, the condition of the wisdom tooth, and its location. For example, surgery on the upper jaw is easier. But removing a wisdom tooth from the lower jaw is more problematic due to the structural features of the jaw and large curved roots.
Possible complications
Wisdom tooth removal is one of the most difficult operations in dentistry. Therefore, after it is carried out, various complications cannot be excluded. Thus, during the operation, neighboring “sevens” are sometimes damaged. Such severe consequences are the result of incorrectly chosen treatment tactics, as well as the low qualifications of the dentist, who was unable to understand the peculiarities of the patient’s anatomical structure.
Mature patients in some cases experience damage to the nervous system and, as a result, impaired sensitivity and numbness. Young patients encounter such disorders much less frequently.
A few hours after the removal of a wisdom tooth, bleeding may develop, which is most often provoked by intense rinsing, irritating the wound with the tongue, or eating hot food. This disorder is especially dangerous for patients suffering from hypertension and bleeding disorders.
Dry socket is the most common postoperative complication. Normally, after a wisdom tooth is removed, a blood clot forms in the socket, which promotes rapid healing of the wound. Sometimes a clot does not form, most often in smokers. After a few days, acute pain may appear, for which you should definitely consult a doctor.
Preventive measures
At the end of the operation, the doctor gives the patient a number of recommendations, compliance with which will speed up the healing of the wound after tooth extraction and will avoid serious complications. Dentists at the Optimal Choice clinics give the following advice to their patients:
- You should not eat or drink hot drinks for three hours after the procedure.
- Alcohol and smoking are prohibited.
- Physical activity should be kept to a minimum. It is also not recommended to smile widely or laugh actively, so as not to tear the seams.
- You can quench your thirst with still water at room temperature.
- Hot water procedures are prohibited: bath, shower, sauna, steam bath, as well as hot compresses.
- Cold compresses for five minutes on the cheek from the side of the extracted tooth will help avoid swelling and reduce pain.
- Mouth rinses are prohibited. You can only use oral baths with decoctions of medicinal herbs, chlorhexidine, furacillin, etc.
- If the doctor has prescribed any medications, then take them as prescribed by the doctor.