Judging by the name, wisdom teeth are supposed to add intelligence to us, but in reality they bring nothing but problems. Why are they even needed? And what to do with these late teeth? Dentist, candidate of medical sciences, head of the expert dentistry center Studio32 Dmitry Vladimirovich Smirnov will dispel the main myths about wisdom teeth and tell you how and when they need to be treated or whether it is better to remove them without regret.
Wisdom teeth received this name because they erupt at the age of 15 - 25 years, when it is believed that a person should already be more or less intelligent. These eighth teeth on the jaw, or third molars, are now considered vestigial because they have lost their original meaning. In the process of human development, our food became more and more soft, as people learned, for example, to heat treat tough meat or grind coarse grains into flour and bake bread from it. Evolutionarily, our jaw has become smaller and smaller and now can no longer accommodate four, essentially, extra teeth. This is where the main difficulties associated with wisdom teeth arise. Most people have them genetically, but there is simply no room for them on the jaw to function normally. There are, of course, lucky people who do not even have the rudiments of wisdom teeth. But 9 out of 10 people still have wisdom teeth, either as unerupted teeth, or erupt in any number from 1 to 4. And in the vast majority of these teeth there are potential problems.
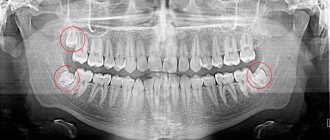
Features of caries on figure eight
The cause of this disease is the accumulation of bacterial plaque and poor hygiene. “Eights” erupt late, on average after 18 - 20 years, and sometimes remain partially unerupted (impacted). At the same time, wisdom teeth are located far in the oral cavity, and it is almost impossible to clean them properly. If part of the crown is located under the gum, a so-called gum hood is formed, where food particles easily fall, and the tooth is destroyed even faster. These factors are the main reasons for the appearance of caries on the figure eight.
Indications for removal
In some circumstances, removing the “eight” becomes the only way out. In particular, the doctor will decide to get rid of the eighth tooth if:
- It is located at an angle and when cutting through it puts pressure on the roots of its neighbors;
- A partially erupted tooth injures the gums;
- When affected by caries, the treatment area is difficult to reach;
- The roots of the "eight" grow in the maxillary sinus;
- The patient suffers from facial neuralgia;
- Complications developed;
- There is a gum cyst in the eruption area.
Symptoms of wisdom tooth caries
The main danger of the disease is that it is asymptomatic for a long time. And if the patient ignores regular preventive examinations at the dentist, he will learn about the problem at a deeper stage. For example, cervical caries of a wisdom tooth is often discovered only when the patient begins to suffer from sudden pain.
At first, a dark spot appears on the enamel, but it is difficult to see, because the tooth is located far away and at an angle. There is no pain because the enamel is devoid of nerve endings.
As the disease progresses, it continues to destroy the enamel and reaches the dentin. Here the first symptoms begin to appear - bad breath, and sometimes short-term pain under the influence of mechanical, temperature and chemical stimuli. You need to remember: if your wisdom tooth hurts, caries is most likely the cause.
Dentin is a porous tissue, so at the middle stage the disease begins to progress very quickly: demineralization of the tooth occurs and necrotic changes begin. Deep caries of a wisdom tooth is characterized by damage to hard tissues, which is why the tooth reacts strongly to hot and cold, sour and sweet. A prolonged aching pain occurs, the coronal part is severely destroyed.
Features of treatment
If the third molars are correctly positioned and the patient visits the clinic in a timely manner, wisdom teeth can be treated – therapeutically or medicinally.
If the doctor decides to remove the nerve, he may prescribe antibiotic treatment to stop the development of the inflammatory process. In case of painful sensations, analgesics will not help to cope with the cause of the disease; they are used only to wait for an appointment with the dentist without pain or to eliminate it after filling the canals. The main thing is not to put off visiting the clinic.
Wisdom tooth caries - treat or remove?
It is important to remember that the carious process cannot be left to chance even at the initial stage: the infection spreads quickly, and even healthy organs of the oral cavity can soon be affected. It's time to answer the question that torments many: if wisdom tooth caries is detected, what to do - therapy or removal?
Removal of a wisdom tooth with caries is indicated
- A wisdom tooth is a rudiment that is practically not used in the chewing process, and there is little benefit from it.
- Eights are located far away, access to them is limited, which makes it very difficult to provide quality treatment. This increases the likelihood of re-infection.
- The therapy is tiring for the patient because he has to sit with his mouth wide open throughout the entire procedure. This is especially true for the treatment of caries of the upper wisdom tooth.
As a rule, removal is indicated in cases where the tooth is dystopic and/or impacted, constantly injures the cheeks and tongue, and causes inflammatory processes due to difficult eruption. Whether to remove a wisdom tooth with caries, if it grows normally and does not cause any problems, should be decided individually together with a specialist.
Structure
Externally, the “eight” is no different from other permanent molars; its uniqueness lies in the following:
- In most cases, teething occurs between the ages of 16 and 25;
- At the moment when the third molar finally appears, the remaining teeth have already taken their places on the jaw, leaving practically no free space. Accordingly, the eighth tooth has to push away its neighbors, which is not always possible;
- Wisdom teeth are extremely difficult to treat because dentists cannot always reach them. And most often, if problems arise with the “eights”, they are simply removed.
Treatment of wisdom tooth caries
Despite the irrationality of preserving the eight tooth, sometimes the doctor recommends abandoning extreme measures and prescribes treatment for the eighth tooth.
Indications for removal of a wisdom tooth with caries
- Caries is at an early stage: the tooth can be saved, and treatment will not be difficult or expensive.
- The figure eight is involved in prosthetics - for example, it is a support for a bridge or clasp prosthesis.
- The tooth erupts normally, without deviations.
- There is an antagonist that will ensure uniform distribution of the chewing load.
- Removing a wisdom tooth with caries is contraindicated due to pregnancy or other reasons, but it is necessary to stop the spread of infection.
Therapy proceeds as follows:
- the affected tissue is removed with a drill;
- the resulting cavity is disinfected with antiseptic agents, an insulating gasket is placed on the bottom;
- the cavity is filled layer by layer with a composite material, which hardens under the influence of a photopolymer lamp;
- The shape of the tooth is adjusted using a drill so that it looks natural and ensures complete closure with the antagonist tooth.
So if you are wondering whether wisdom teeth cure tooth decay, then the answer is yes. However, it is important to consult a specialist in time and not to advance the disease.
Functions
Opinions differ as to why our contemporaries need eighth teeth. Some experts believe that since the “eights” were created by nature and still appear, then they should not be removed unless absolutely necessary. In addition, sometimes the third molar becomes a real lifesaver for fixing a denture. Other doctors are sure that it is better to immediately remove wisdom teeth if they cause concern. After all, these rudimentary organs no longer fulfill their main role - people have long switched to soft foods that have undergone heat treatment.
Deep caries of wisdom tooth
If the development of the carious process is not stopped in time, the infection will gradually penetrate deeper and eventually reach the pulp. Inflammation in the pulp tissue is called pulpitis and is accompanied by aching pain that is difficult to ignore. It is not easy to treat deep caries of wisdom teeth, since it is necessary to fill the root canals, and the roots of figure eights are usually curved. Untreated pulpitis can develop into more serious diseases - wisdom tooth cyst or periodontitis, which are much more difficult to combat.
In addition to location, dentists classify caries according to the depth of the pathology:
- The spot stage is considered the mildest. This type is easy to clean and saves the tooth from further damage.
- The superficial type of caries is characterized by the process of demineralization of tooth enamel with further destruction.
- Deep caries is characterized by irreversible destructive effects on the tooth due to the development of carious microflora. During the examination of the affected tooth, you can see a layer of dentin located between the pulp and the bottom of the carious cavity.
Based on the types of anatomical location, caries of dentin, enamel and cement is distinguished.
Tooth perforation: what to do and should you panic?
Perforation (of the bottom, walls of the tooth or root canal) is a complication that can occur during endodontic treatment when working with burs, hand or machine tools for mechanical treatment of the canal, as well as when installing pins and inlays, and representing a pathological (unnatural) message (hole) with supporting surrounding tissues (bone, gums, periodontal ligament).
Types of perforations
By localization level:
- Crown part of the tooth
- Walls of the tooth crown
- In the area of furcation (furcation is the junction of the roots of the tooth in multi-rooted teeth
Root part of the tooth (canal)
- Wellhead
- Middle part
- Apical part
By time of occurrence:
- Fresh:
which arise during the treatment process and are immediately covered with special materials - Old:
after the occurrence of which no measures were taken to eliminate them, which worsens the prognosis and can lead to additional complications (infection, fracture, crack)
By type of perforation:
- Spot
- Strip perforations (ribbon, longitudinal)
Possible causes of perforation
Let's now see why this complication may occur.
Perforations are most often associated with doctor errors (careless work with burs, ignorance of anatomy and lack of experience, incorrect use of instruments for mechanical processing of canals, etc.). Also important are dental dystopia (improper position in the dentition), complex anatomy of the root canal system, calcification of the dental cavity and obliteration of canals.
Very rarely, the cause may be injury or advanced caries.
Let's look at each type of perforation in more detail.
Perforation of the tooth wall
most often occur when working with burs when creating access to the root canals and deviation from the axis of the tooth.
Perforations in the furcation area
arise as a result of excessive preparation in the process of creating access to the root canals; when installing pins, when they deviate from the course of the channel; when searching for the mouth (entrance to the canal) in case of obliteration (obliteration or calcification - a process in which replacement dentin is deposited, which tightly closes the lumen of the canal).
Perforation of the root canal wall
can occur with a complex anatomical structure of the canals (bends, branching canals), with excessive pressure on the instruments, incorrect direction of insertion of the instrument, with errors in the initial stages of work (creating steps, blocking the canal lumen with sawdust with insufficient irrigation), when preparing the canal for the pin, when trying to remove broken fragments of instruments, as well as during repeated endodontic treatment.
Strip perforations
usually occur when preparing a channel for a pin or when trying to remove broken fragments of instruments. In this case, the canal wall seems to be “worn” and an elongated defect is formed.
How to diagnose perforation?
If perforation occurs during treatment, the patient may feel pain, and the doctor will visually see bleeding from the perforation area.
We can see old perforations on x-rays and when analyzing a computed tomogram. For example, an unfilled or underfilled canal, periapical lesions, excessive release of filling material in the root wall area, deviation of the filling material from the course of the canal when the boundaries of the installed pin cross the boundaries of the canal. All this can help to suspect the presence of perforation.
We can also visualize perforation using an operating microscope during repeated endodontic treatment or diagnostic preparation.
Symptoms of perforation
Fresh perforations are usually not accompanied by symptoms, but pain may occur when they occur.
Old perforations are also usually asymptomatic.
There may be periodic discomfort when biting or minor pain.
Treatment of perforation
Treatment tactics depend on many factors:
- In which area did the perforation occur: the most favorable prognosis are defects of the apical part, because, as a rule, they are not infected. The most unfavorable ones are the furcation and estuarine ones, because the zone of maximum infection is located in this part.
- Fresh or old perforation
- Is there apical periodontitis or not?
- At what stage did the perforation occur: at the initial or final stage? Defects that occur at the beginning of work have a greater risk of infection and therefore require additional medical treatment
- Perforation size
If this perforation is fresh, then after stopping the bleeding it must be immediately closed with MTA-based material. This is a special cement (mineral trioxide aggregate), which has biocompatibility, a chemical bond with dentin, a high degree of sealing and stimulates the formation of cement-like tissue, which is especially important for us when closing such defects.
If this is a small root canal perforation, it can be closed by filling the canal with a bioceramic sealer.
Old perforations, as a rule, always become infected, therefore, before closing them, it is necessary to clean the edges of the perforation: mechanical removal of infected dentin and medicinal treatment (in essence, this is a kind of “wound”, which requires the removal of “contaminated” tissues before applying a medicinal ointment).
Thus, the faster the perforation is closed, the better, because the risk of damage to periodontal tissue (ligament and bone tissue), which leads to lesions that are difficult to treat, is reduced.
But if you leave the problem without treatment, you can get complications, such as:
- Infection and development of apical periodontitis
- Root cracks
- Root fractures
After treatment of a tooth with perforation, it is subject to dynamic observation and radiological control.
Let's summarize: creating a perforation in the vast majority of cases is a doctor's mistake, despite modern technologies and tools. Such mistakes happen quite often, and it is rare that a doctor has never perforated a single tooth in his entire practice. No one is immune from this error, but if you follow a number of certain rules, you can reduce the risk of perforation to a minimum.
Possible complications
Depressions in the enamel themselves signal the presence of problems. If your hole in the tooth begins to hurt, even if not very much, it is recommended to immediately seek the help of a doctor. Otherwise, there will be a huge number of unpleasant consequences.
Among the most common types of complications are pulpitis and periodontitis. In the first case, there is simply acute inflammation of the dental nerve, with severe aching pain. In the second, the dental ligaments that secure the tooth to the bone are damaged.
Important! The main mistake that patients make is using a large number of analgesics. Despite the fact that they relieve pain, the process of decay in the tooth does not stop, and along with this, the death of the nerve occurs, which leads to complete loss of the tooth.
What causes a black hole to form in a tooth?
The main reason for the formation of holes in teeth, as already mentioned, is caries. Being a consequence of the activity of bacteria and microorganisms, it can lead to complete destruction of the tooth. Doctors note that there are many reasons for its appearance.
Important! According to statistics, women suffer from caries more often than men. This is associated with hormonal changes in the body that occur in women during pregnancy and lactation. In addition, people with malocclusions are more likely to develop cavities and holes in their teeth. Too narrow spaces between teeth, thinned enamel - all this contributes to the accumulation of food and the creation of a favorable environment for the development of microorganisms.