As soon as you say “tooth canal,” people worry about toothache. Why does the mention of root canals scare people so much? Most patients believe that root canal treatment is a very painful procedure. While with the development of modern dental technologies, the treatment process has changed a lot.
There are many myths associated with root canal treatment, and in this article we will present real facts that will help people who are faced with a similar problem to find out the real state of affairs.
Root canal treatment is a very painful procedure.
This is not true. Root canal treatment does not cause pain. In fact, root canal treatment is performed to relieve pain from inflammation of the pulp chamber (where the nerve is located) or a dental abscess. The myth that root canal treatment causes severe pain is becoming a thing of the past. With the use of modern anesthesia methods, this procedure is no more painful than installing a filling.
If there is a serious abscess process, anesthesia may not work, and your doctor will prescribe antibiotics before root canal manipulation. If a root canal is difficult to access, your dentist may refer you to an endodontist, a doctor who specializes in treating dental cavities and root canals.
What is a root canal
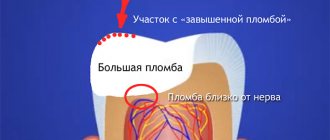
In addition to enamel and dentin, any tooth has a fairly large internal cavity. Its main part is called the pulp chamber. Thin tubules extend from it. They are located along the entire length of the roots. These are root canals. The number of roots varies among different groups of teeth. Accordingly, the number of channels is also different. The front teeth have only 1 canal. Side groups can have from 2 to 4.
Dental tubules are narrow tubes with many branches. They originate at the top of the root. This place is called the apical foramen. From here, neurovascular tissue passes to each root. If it is inflamed or dead, it is removed during endodontic treatment. Next, the resulting cavity is cleaned of its residues, disinfected and sealed.
Root canal treatment is expensive
Right. Although root canal treatment is expensive, it allows you to preserve the tooth, as well as its functionality and chewing functions. If you have a root canal and install a crown on the tooth, the cost of treatment will be less than if you remove the tooth and replace it with a bridge or dental implant.
The cost of treatment will depend on how many root canals the tooth has, whether it is the first time it has been treated, and on the qualifications of the dentist (general dentist or specialist).
Modern methods of endodontic treatment
In the treatment of tooth canals today there are two approaches: therapeutic and surgical. Let's look at them in more detail:
Therapeutic treatment. With this method, it is possible to preserve the entire pulp or at least part. The drug is placed into the cavity. The pulp chamber is isolated using a special gasket, then the tooth is filled. The drug can also reach tissues through dentin. To do this, special bandages with antibiotics are applied to the tooth. This therapy is used only in the initial stages of the inflammatory process.
Surgery. In this case, the pulp is completely removed, the canals are cleaned, disinfected and sealed. There are the following methods for filling cavities:
- Classical. The canals are filled with conventional filling material.
- Vertical filling. A special filling composition is administered as an injection.
- The use of thermophiles. A special heated composition on a carrier is placed into the cavity.
Sometimes, in order to cure the canal, you have to remove the tip of the root. This measure is necessary for cysts, granulomas, perforations, fibroids and other problems.
Toothache disappears immediately after the procedure
Wrong. After completing the treatment procedure, the patient will feel a significant improvement. However, it is normal for the tooth to remain sensitive for a few days after the procedure - in this case, taking painkillers may help. Minor pain may be present, especially when chewing, and may persist for several weeks. After this period, the pain should completely disappear.
Is it possible not to experience any pain after root canal treatment? Yes, this is possible, and it depends on how difficult the treatment process was and whether the tooth was infected before the dental intervention.
Content:
- Features of canal treatment
- Processing sequence
- If pain occurs after therapy
- Complications
For pulpitis, periodontitis, and dental cysts, the canals are cleaned. This is a complex dental procedure that uses specialized equipment. The patient cannot refuse it, since there is no other way to prevent the spread of the inflammatory process.
The effect of treatment is short-lived
Wrong. Although nothing can completely replace a healthy tooth, quality root canal treatment followed by a suitable filling or crown can be very successful. In approximately 85% of cases, the effect of treatment is lifelong.
If a tooth becomes affected again several years after root canal treatment, it often needs to be re-treated. However, in some situations, such as a crack in the tooth, very severe tooth root decay, or severe loss of bone around the tooth, the dentist has no choice but to remove the affected tooth.
Medical Internet conferences
Substances for treating root canals must meet certain requirements: 1. Be bactericidal for microorganisms located in the root canals; 2.Have a quick effect and penetrate deeply into the dentinal tubules; 3.Do not lose its effectiveness in the presence of organic substances; 4.Do not have a smell or specific taste; 5.Be chemically resistant and remain active during long-term storage; 6.Be harmless to periapical tissues and promote their regeneration; 7.Do not have a sensitizing effect and do not cause the emergence of resistant forms of microorganisms. Basic provisions justifying the need for disinfection of root canals: 1. Complex anatomy of root canals, which provides a favorable environment for the growth, reproduction and interaction of microorganisms; 2. In teeth with necrotic pulp and inflammation of the root apex, gram-negative anaerobes predominate; 3. Microorganisms are present in all areas of the root canal, including lateral canals, anastomoses and dentinal tubules at a depth of up to 300 µm; 4. Microorganisms receive nutrition from living or necrotic pulp, salivary proteins and periodontal tissue fluid, and from other bacteria; 5. The waste products of microorganisms negatively affect pulp tissue and are toxic to periodontal tissue. Classification of antiseptics for root canal treatment: 1. Halides 2. Oxidizing agents 3. Nitrofuran preparations 4. Quaternary ammonium compounds 5. Urea or urea 6. Proteolytic enzymes 7. Complexones (chelates). Halides include two types of drugs - chlorine-containing and iodine-containing. Chlorine-containing preparations are presented: 0.05-0.06% chlorhexidine solution, 2-4% chloramine B solution, 1-5% sodium hypochlorite solution, 2% aqueous solution of chloramine T. The mechanism of action of these drugs is based on the release of chlorine gas, which penetrates into the dentinal tubules, disinfecting their contents and destroying organic residues. The most common drug in this group is sodium hypochlorite . The drug was first proposed by G. Deyikn as a wound disinfectant during the First World War, and only a few years later this antiseptic began to be used for root canal irrigation. It has a number of properties that have made it so popular in endodontics: the unique ability to dissolve the organic contents of root canals: necrotic tissue, decay products, scraps of extirpated pulp; pH values range from 11 to 12; pronounced antimicrobial effectiveness, bactericidal effect, consisting in the oxidation and hydrolysis of proteins in microbial cells; is a good lubricant; chemically resistant; has whitening properties; economically beneficial. Sodium hypochlorite, when interacting with tissue proteins, quickly disintegrates, releasing atomic chlorine, which combines with amino groups to form a substance called chloramine and, as a result of the resulting reactions, peptide bonds are broken, proteins dissolve, and do not coagulate, as with the action of other disinfectants. As a result, chloramine disinfects the root canal, which has already been cleared of organic matter, and also dissolves the contents of the lateral tubules or apical delta, which cannot be processed instrumentally. The negative properties of sodium hypochlorite, as well as various other chlorine-containing compounds, are the following: decreased activity in the presence of organic substances, which makes it necessary to re-rinse the root canals; have an irritating effect on periodontal tissue; have a specific, unpleasant odor. It is presented on the market in the form of preparations: Edetal gel (5 ml Omega-Dent, Russia), Parkan (250 ml, Septodont, France), Belodez (30 ml, 100 ml Vladmiva, Russia). Iodine-containing include : 1% aqueous solution of iodinol containing iodine, potassium iodide, polyvinyl alcohol, distilled water. The drug has bactericidal and fungicidal properties due to the action of molecular iodine, it also accelerates regeneration and phagocytosis, has a prolonged effect and is also an indicator of the cleanliness of the root canal (the drug has a blue tint, but upon contact with necrotic tissues, discoloration occurs). A well-known representative of the group of oxidizing agents is hydrogen peroxide, used in the form of a 3% solution. Hydrogen peroxide has a bactericidal effect due to the release of molecular oxygen upon contact with organic tissues, especially against gram-negative microflora. The advantage of this substance is also its hemostatic properties. The disadvantage of a 3% hydrogen peroxide solution is the lack of ability to dissolve necrotic tissue and organic residues, therefore it is recommended to alternately use solutions of hydrogen peroxide and sodium hypochlorite; the interaction reaction between these substances leads to the release of free chlorine and oxygen, which enhances the cleansing and bactericidal properties of these substances. Quaternary ammonium compounds. Includes 1% decamin solution , 15% decamintoxin, biosept. These drugs have bactericidal, bacteriostatic and fungicidal effects, are active in the presence of organic substances, have an anesthetic effect and enhance the effect of other antiseptics. In endodontic practice, drugs based on urea (carbamide) , for example the drug Cly-oxide , the drug is a 10% solution of urea peroxide in glycerin. In addition to the lack of toxicity, the drugs have an antiseptic effect, lyse necrotic tissue, and also potentiate the effect of antibiotics. Drugs of the nitrofuran series include 0.5% solution of furatsilin , 0.1-0.15% solution of furadonin, furagin, furazolidone. The positive properties of these substances include their bactericidal effect on gram-positive and gram-negative microflora, as well as on fungi, stimulate phagocytosis and have an anti-exudative effect. A group of proteolytic enzymes. This group includes preparations of trypsin and chemotrypsin , which are prepared immediately before use - ex temporae, by diluting the crystals in a 0.9% isotonic solution of sodium chloride or 0.5% novocaine solution. This group also includes immobilized enzymes - stomatozyme, immozymase, produced in the form of a gel, ready for use. Proteolytic enzymes are capable of lysing necrotic tissue, have an anti-inflammatory and anti-exudative effect, have an anticoagulant effect, and also deprive microorganisms of a nutrient medium due to which they exhibit an indirect bacteriostatic effect. But despite a number of positive properties, these root canal treatment products often lead to the development of allergic reactions and are also quickly inactivated.
Comparative table of the main properties of representatives of the main groups of antiseptics for root canal treatment:
| Antiseptics | Bactericidal | Toxicity | Having an unpleasant odor or taste | Action in the presence of org. substances | Efficiency |
| Sodium hypochlorite | +++ | +++ | +++ | +++ | +++ |
| Hydrogen peroxide | +++ | ++ | — | — | ++ |
| Chlorhexidine | +++ | — | — | +++ | ++ |
| Urea | +++ | — | + | +++ | ++ |
Unfortunately, today antiseptic solutions of the nitrofuran series have lost their importance in endodontic practice, as some strains of microorganisms have developed resistance to nitrofurans, which has led to a sharp drop in the effectiveness of these drugs. It should be said that an analysis of medical records of dental patients allows us to draw conclusions that the use of sodium hypochlorite in endodontics gives better results than other disinfectants, which is due to the distinctive abilities of its antimicrobial action. It is important to remember that when working with this substance, it is necessary to strictly observe all safety measures: rubber dam, saliva ejector, vacuum cleaner, in order to avoid contact of the antiseptic with the oral mucosa. Complications associated with the use of the drug occur, first of all, due to the release of the drug beyond the top of the canal, which leads to the development of swelling, bleeding, pain, and in some cases, the development of parasthesia and secondary infection is possible.
Based on the material presented, we can conclude that in modern endodontics there is no universal remedy that fully meets all the requirements and is capable of destroying all the diverse microflora found in infected dental tissues; but we can definitely say that medical treatment of root canals using antiseptics is an important stage of endodontic treatment and allows you to avoid possible dangerous complications not only on the tissue of the maxillofacial area, but also on the entire body as a whole.
Mild but prolonged pain after treatment is normal
Wrong. It is not normal to experience constant pain for up to several months after root canal treatment. Causes of pain include hidden canals that were not cleaned during the procedure, or a crack in the tooth.
In these rare cases where pain persists, patients should be referred to an endodontist who specializes in root canal treatment for a diagnosis and appropriate treatment. In cases where the root or tooth is destroyed and no treatment method is suitable, the dentist has no choice but to remove the tooth.
What does the canal consist of and why should you clean it?
The inside of the dental canal is filled with pulp. It is a soft tissue penetrated by nerve fibers. In addition, it contains blood and lymphatic vessels and connective tissue. When an inflammatory process occurs in the pulp, the soft tissues inside the canal are also affected. Sooner or later it comes to such an extremely unpleasant thing as their necrotization.
The cause of inflammation can be caries or pulpitis. Therefore, in order to relieve the patient of acute pain and prevent tooth extraction, it is necessary to clean the dental canals of dead tissue.
The capabilities of modern dentistry in the vast majority of cases make it possible to completely cure and save the affected tooth, while just 10 years ago such inflammation invariably led to surgical removal of teeth.
Important! A disease that has become chronic may well be asymptomatic.
A root canal “kills” the tooth.
Wrong. During root canal treatment, the inside of the tooth is cleaned and disinfected, which helps heal it; it does not kill the tooth. The nerves and blood vessels located in the pulp chamber serve to develop the tooth if it is a child or teenager.
The function of the nerves is to signal pain when something is wrong with the tooth, be it decay, infection, inflammation or injury. Pain, therefore, is a defense mechanism that encourages a person to look for its cause and eliminate it.
Reasons for the development of complications
The very cause of severe pain in the case of each patient must be considered separately. Among the most common sources of such pathology may be the following:
- Incorrectly chosen treatment method, gross mistakes made.
- The channel was not cleaned correctly.
- The doctor left foreign objects inside the canal, did not clean out the tooth fragment, and broke the instrument.
- The patient had a sudden allergic reaction to anesthesia or root canal filling agents, or various medications taken during treatment.
- The filling was placed poorly.
- Severe periodontitis developed and gum damage began.
- The canal walls were perforated during the cleaning process.
- The root of the tooth has received any damage.
Against the background of all of the above, the inflammatory process can actively develop. It becomes the cause of severe pain experienced by the patient.
Need to take painkillers
Right. Relatively, this is true. The pain experienced after root canal treatment is usually caused by inflammation around the tooth and may only last for a limited period of time. This process can be successfully managed with the help of common anti-inflammatory drugs: ibuprofen (Advil, Motrin), acetaminophen (Tylenol).
If severe pain continues for several months after the procedures, you should consult a dentist or endodontist to avoid possible complications.
Processing sequence
Endodontic therapy includes several successive stages:
- Extraction of pulp tissues. All inflamed areas are removed from the cavity of the dental crown.
- Treatment of the tooth canal with sanitizing compounds , cleaning it from bacteria, pathogens, and necrotic accumulations. As a result of this stage, the inflammatory process is stopped.
- Changing the natural shape of the root , giving it an optimal width for further processing. The doctor needs to not only create conditions for optimal patency, but also make sure that the apex of the root reaches the apical part.
- Sealing. This is the final stage of therapy. The cleaned and expanded cavity is filled with filling material. Then a filling is placed and it is polished.
After treatment, the tooth stops hurting and acquires an aesthetic appearance. But we must take into account that now it does not receive the necessary nutrition, that is, it is essentially dead.
This means that its service life will be shorter than that of healthy neighbors. After a few years, small cracks may appear on the surface of the crown or chips may form. Therefore, it is important to take special care of the treated unit and periodically carry out a remineralizing course using special dental gels.
Teeth that have undergone root canal treatment often require a crown.
Right. Often, teeth undergoing root canal treatment have severe caries or large fillings. A tooth with a large filling is at high risk of destruction. For this reason, your dentist may recommend that you get a post and crown after root canal procedures.
Some dentists place a post and filling on the tooth immediately after the root canal has been treated. Although a post adds more strength than a filling alone, a crown is also recommended to improve strength characteristics.
Endodontic instruments during cleaning
To effectively clean the canal, it is necessary to use several types of instruments, usually made of strong wire. Some of them are used in particularly difficult cases when the passage of channels is difficult. The specialist, taking into account the condition of the patient’s dental passages, can select rigid devices with a square cross-section, which are durable, but are less efficient at evacuating dentine filings. Another option is triangular-section reamers, which have increased flexibility but break more easily.
Groups of tools by purpose of use:
- channel expansion. The most commonly used options: Pro File 04, ProTaper, Rasp, K-flexofile, Rotary Instrument;
- increase in the diameter of the canal mouth. : Varieties: Largo and Gates Glidden;
- facilitating passage of the canal. Types: K-reamer, K-reamer farside;
- removal of tool remains. Instrument Removal System, Masseran Extractor Kit.
An auxiliary device is a microscope, which helps to visually zoom in on the channels and ensure high precision of the manipulations performed.
Advice! The safest instruments are considered to be nickel-titanium reamers, which bend easily and “remember” their shape after penetration into the canal.
Root canal treatment is a lengthy process that requires several visits to the doctor.
Wrong. Today, root canal treatment can take one to two hours if there are no complications. The number of visits to the dentist often depends on the condition of the tooth and the number of canals in it.
In cases where the damage is severe, your dentist or endodontist may place medication inside the canal to prepare (disinfect) the inside of the tooth and then finish treatment after a few days. But if there are no lesions or complications, all procedures can be performed in one visit.
Sealing
This moment is very important. Today, two main methods are used to fill dental canals: introducing dense cone-shaped gutta-percha pins into the canal (the so-called lateral condensation) and filling a fragment of the dental canal with a heated mass from the same gutta-percha, followed by the introduction of cone-shaped pins (the so-called vertical condensation). Both of them are very effective and allow you to reliably “seal” all additional branches of the main channel.
All filling materials come in two types. The first is sealers, also known as endosealants, that fill the root canal. The second is the so-called fillers, which fill the lumen of the dental canal. Sealers are divided into pastes based on epoxy resins, calcium hydroxide and zinc oxide, as well as cements.
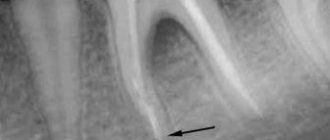
Upon completion of dental treatment while asleep or under anesthesia, the doctor sends the patient for an x-ray - it is important to find out whether the root canals are completely filled with endodontic filling material. If everything went well and the canal is in order, you can proceed to the final part of the process - filling the inlet.
Manual cleaning of canals with removed pulp
After poor-quality cleaning of the canals or removal of the nerve using the formalin-resorcinol method, infection and even pus may form in the canals if the inflammation is localized in the tissue area next to the tooth. The process of sclerotization of the canals becomes a barrier to high-quality cleaning; therefore, in this case, the procedure of widening the passages with the help of reamers is also carried out. After restoring the patency of the canals, chemical antiseptic cleaning is immediately carried out to remove any inflammation. In dental practice, irrigation is often performed using a cannula and irrigation needles.
Features of the traditional antiseptic rinsing method:
- the solution is fed through a syringe into the root canal;
- Pressure is applied to the syringe with the index finger;
- the released liquid is collected with a saliva ejector;
- the solution is held in the channel for 1 minute;
- The antiseptic is washed off with distilled water.
To enhance the impact, feeding can be done together with reciprocating movements, and not just by passive infusion. After the cleansing, treatment begins, which can last up to 2.5-3 months. During this period, the dentist places and periodically changes the disinfectant solution.
Cleaning canals in the presence of pulp
Carrying out a disinfection procedure is impossible without removing the fibrous nerve tissue - the pulp. The reason is that the channels are filled with this mass; an additional reason is the inflammatory process of the connective tissue, which in this case must be eliminated. To open the cavity, different places of influence are used with a drill: on the chewing ones - from the top, on the front - from the side.
Pulp removal algorithm:
- Introduction of anesthesia.
- Tooth preparation.
- Nerve killing.
- Placement of a temporary filling.
The pulp is killed by applying a special arsenic paste, or other options - Devit, Pulpex-S, paraformaldehyde variety. The use of these products allows us to call this part of the cleaning chemical. After a day or two, the tissues die, then the filling is repeated and a pulp extractor is used. By inserting it into the tissue and turning it in a circular motion, the dentist wraps the pulp around the device and removes it from the canals in parts.
After this procedure, reamers are introduced to help expand the mouth and the canals themselves. The thinnest instruments are used first, and then those with larger diameters. Periodically - usually after each manipulation - a disinfectant liquid (chlorhexidine, sodium hypochlorite, EDTA or hydrogen peroxide) is injected, which also helps to wash away detached areas of the pulp. If you do not carry out the procedure for expanding the canals, the quality of the filling will deteriorate significantly (voids may occur). The final part is a permanent filling.
Fact! The tooth being treated is protected with an insulating latex cloth to prevent saliva and bacteria from entering the canals.