The compatibility of simultaneous or alternate use of paracetamol and nimesil is the personal experience of the author, who almost died from such a combination.
I was a fool.
Because I didn’t ask in advance whether nimesil and paracetamol could be used together. Because of this, I almost went to another world.
There were several motives for committing terrible drug-induced violence against oneself.
- Firstly, I was in a hurry to get better; I developed some kind of terrible viral bronchitis, which could very well turn out to be a real coronavirus. I couldn’t get sick – I had a small child in my arms and an elderly man who required constant care.
- Secondly, we sell Nimesil in small bags individually, so the instructions had to be studied separately, and I was too lazy to do this. In addition, I have been using Nimesil for quite a long time - it is a fairly good remedy for headaches, or at the first signs of a cold. My throat started to hurt a little, I took the packet, and in the morning you are fine. At least, that's how it worked for me.
Paracetamol is also a proven remedy since childhood. I never thought that taking Nimesil and Paracetamol together would turn me into a zombie.
The first day
The cold just keeps on coming. Or maybe it's coronavirus? I sneeze loudly and quickly like a Kalashnikov machine gun, simultaneously making predictions that tomorrow the neighbors will shy away from me when they meet. The city has a special quarantine regime.
Temperature 37. Took 2 tablets of paracetamol at intervals of 4 hours. My head and throat hurt badly. Without a second thought, after 3-4 hours I took a packet of Nimesil, and at night another paracetamol tablet.
At night I felt sharply worse and developed a cough. I couldn’t sleep, except that I dozed for about 40 minutes at the table.
How to take Nimesil and Paracetamol?
Taking Nimesil is allowed only in adults. The drug should be taken orally after meals. The average daily dose is 200 mg, taken in two doses of 100 mg. To prepare the suspension, you need to pour the powder from the bag into a glass and add warm boiled water. If necessary, you can increase the dose.
The dosage of the drug can be adjusted depending on the severity of the condition and the susceptibility of the patient, as well as for older people.
Paracetamol tablets are prescribed in a dosage of 0.35-0.5 g 3-4 times a day. The maximum permissible single dose for adults is 1.5 g, the maximum daily dose is 3-4 g, for children from 9 to 12 years old it is 2 g, from 3 to 6 years old – 1-2 g.
Paracetamol, in the amount of 60 mg per 1 kg of child’s weight in 3-4 doses. The drug is taken after meals with a sufficient amount of water.
Paracetamol rectal suppositories for adults and adolescents weighing more than 60 kg are prescribed 3-4 times a day in a dosage of 0.35-0.5 g. The maximum permissible single dose is 1.5 g, the maximum daily dose is 3-4 g. For children from 1 month to 3 years, single dose – 15 mg per 1 kg, daily dose – 60 mg per 1 kg of child’s weight. Suppositories are used 3-4 times a day.
For children from 6 to 12 years old, the maximum permissible daily dose is 2 g 4 times.
For children from 3 to 6 years old, the maximum dose per day is 1-2 g, in the amount of 60 mg per 1 kg of child weight, 3-4 times. Paracetamol in syrup form for adults and children weighing more than 60 kg is taken 20-40 ml of syrup (480-960 mg) 3-4 times a day. Children from 3 to 12 months are prescribed 2.5-5 ml of syrup (60-120 mg), from 1 to 5 years - 5-10 ml of syrup (120-240 mg), from 5 to 12 years - 10-20 ml of syrup (240-480 mg) 3-4 times a day.
Second day
The cough is becoming more intense. I take mucaltin, lozenges for a sore throat, and also irrigate my cold throat with the drug “Inhalipt”. I took a paracetamol tablet in the morning and at lunchtime.
I would like to lie down, but I need to take pills to my sick grandmother. Without contacting anyone, I jump into the car and drive, feeling like I’m in a fog.
The sore throat went away, but in the evening I had a severe headache again. The cough becomes very intense, and heaviness appears in the chest. I drink a packet of Nimesil again, hoping that the syndrome will be relieved. This helps for a while.
I can't sleep at night. I'm coughing. Whistling breathing. Bronchitis. I suffer, I try sounds of nature, try different positions, but I can’t fall asleep. The pulse on the smart watch shows about 100 beats per minute.
Temperature. The second sleepless night and fever are cruel.
I'm squeezed like a lemon.
Latest information and popular answers on COVID-19!
June 30, 2021
Dear friends!
Every day we receive many questions from you about the COVID-19 . Our colleagues, the Association of Family Doctors of Kazakhstan , have prepared answers to the most popular questions that concern everyone so much now. All information was prepared by doctors on June 30, so you can find the most up-to-date information below:
IF YOU ARE SICK
1. I have developed symptoms of coronavirus infection / I suspect that I have coronavirus / I have tested positive for coronavirus / A CT scan has revealed signs of viral pneumonia. What to do?
Your next steps depend on how you feel and your symptoms.
Remember that 80% of people infected with Covid-19 show no symptoms or are only mildly ill.
It is easy to get sick with coronavirus infection - that means:
• your body temperature does not exceed 39°;
• you are not out of breath (you can walk around the apartment/house, you can take a shower, go to the toilet, drink tea, etc.)
• shortness of breath and cough do not interfere with your ability to speak;
• other symptoms: headache, dry cough, sore throat, muscle and bone pain, loss of smell and taste, diarrhea - may or may not be present.
If symptoms appear mildly, the general recommendations below should be followed:
1) Self-isolation so as not to infect other people.
Stay home. If you do not live alone, you must have a separate room, the doors to which must be constantly closed, the room itself must be constantly ventilated, and all surfaces in it must be regularly treated with disinfectant solutions. Your family members should leave everything you need (food, drinks, hygiene products, etc.) at your door. If you leave the room to visit the toilet or bathroom, you need to wear a mask, after yourself you need to treat all surfaces that you touched with a disinfectant solution, also wash your hands thoroughly with soap and treat them with a sanitizer (alcohol solution).
2) Call the clinic and tell your local doctor about your symptoms.
This is necessary so that the doctor can monitor your condition remotely, and if it worsens, help hospitalize you.
3) Drink plenty of warm drinks - up to 2-4 liters per day.
Increased fluid intake helps relieve intoxication, headaches, reduce fever, overcome dehydration (with fever, shortness of breath and diarrhea, your body loses a lot of fluid) and thin the blood.
What drink? First of all, clean water (2-3 liters), any tea with raspberries, currants, sea buckthorn, barberries, honey (if there are no allergies), broths (chicken, beef, lamb, horse meat). It is not advisable to drink a lot of sugary drinks, especially for people with increased weight.
4) Breathing exercises - 2-3 times a day
Breathing exercises will help relieve congestion in the lungs and increase the reserves of the respiratory system. The basic principle is to hold your breath for 7-20 seconds after taking a deep breath. Then exhale strong and long. It is necessary to use the posterior lower sections of the lungs. Try not to lie in bed or sit for a long time.
A video with breathing exercises will be released soon on the ASVK insta account in partnership with the Freediving Federation of Kazakhstan
5) Physical activity
Try to get up, walk, do light exercises to stretch your muscles and joints: turns, bends, etc. Even if you have little strength, do not lie on your back for a long time, always turn on your side or stomach.
6) Get a good night's sleep
7) Balanced diet
Try to eat more raw fruits and vegetables (cabbage, herbs, peppers, cucumbers, etc.).
 Taking vitamin D3
Taking vitamin D3
Vitamin D3 has proven effective against other acute viral infections. Research shows that low levels of vitamin D3 in the blood have been linked to more severe Covid-19. Take 2,000 international units (IU) once daily with meals, especially if you are known to have low blood levels of vitamin D3.
9) Control of respiratory rate per minute
1 cycle of respiratory rate is inhalation + exhalation. Another person must take the measurements when you are at rest, that is, sitting or lying down. The normal level of respiratory rate in an adult is from 12 to 20 cycles per minute; a respiratory rate above 24 per minute is an indicator of shortness of breath.
10) Temperature control - 2-3 times a day
11) Pulse monitoring - 2-3 times a day
12) Symptom Diary
Keep a notebook in which you will write down your symptoms, as well as your respiratory rate, temperature and pulse. Share these indicators with your local doctor. The Ministry of Health has released a convenient checklist. You can download or view it here.
There is currently no specific treatment for COVID-19, so symptomatic treatment is recommended if necessary.
In case of poor tolerance to fever or severe malaise, regardless of temperature (muscle pain, headache, “aches” in the body and joints, general painful condition):
— Paracetamol 500 mg — 1 tablet up to 3 times a day (every 6-8 hours)
or
— Ibuprofen 200 mg — 1 tablet up to 3 times a day (every 6-8 hours)
For sore throat, sore throat, cough:
— Resorption of antiseptic tablets
If there are signs of gastroenteritis (vomiting, diarrhea):
— Regidron — 1 sachet per liter of warm boiled water (up to 2-3 liters per day during the day)
If you have severe nausea:
— Metoclopramide (Cerucal) 10 mg — 1 tablet up to 3-4 times a day 30 minutes before meals
or
Ondansetron 4 mg (lozenges) - 1 tablet 3-4 times a day 30 minutes before meals
+ Basic therapy for concomitant chronic diseases (arterial hypertension, diabetes mellitus, coronary artery disease, asthma, COPD, etc.)
Routine administration of antiviral and antibacterial drugs is not recommended because they do not work against SARS-Cov-2.
It is not recommended to prescribe multivitamin complexes and dietary supplements, as well as so-called immunomodulating / immunostimulating drugs that do not have an evidence base.
In the vast majority of cases, the disease will proceed as a normal viral infection, and the body's immune system will cope with the disease itself. That's why:
• no need to panic;
• you do not need to take any other unproven “medicines”, vitamins or nutritional supplements promoted by dishonest manufacturers for Covid-19;
• no need to breathe alcohol, soda or anything else like that;
• there is no need to call an ambulance unnecessarily or try to call a family doctor at home;
• no need to take antibiotics, antiviral drugs, aspirin, etc.;
• there is no need to strive to get tested for Covid-19.
2. Why is there no need to urgently go for a PCR test and CT scan?
Testing for coronavirus will do nothing if there are no symptoms. You can get a negative result from a nasopharyngeal swab today, but become infected tomorrow.
But even if there are symptoms, there is no need to take any action to make sure that they are associated with coronavirus infection. Unfortunately, these examinations do not provide any specific answers to the questions: what to do next, how to be treated, what to take. The sensitivity of PCR is very low (30-60%). In other words, if you are typically sick, and the “smear is negative,” this does not give grounds to deny the presence of coronavirus infection in your body, that is, with a probability of 40-70% you are still infected with coronavirus.
The analysis will not affect your chance of recovery in any way, but can greatly complicate the situation. For example, you could become infected while being tested. Any visit to a hospital, clinic or laboratory is dangerous for infection, because sick people accumulate there. A negative test creates a false sense of security, while tests for Covid-19 are often falsely negative. A positive test result does not in any way affect further treatment tactics, since there is currently no specific treatment for coronavirus infection, and in any case, the outcome depends only on your immunity.
Computed tomography (CT) of the lungs is an excellent method, but it is not used to diagnose coronavirus as such, but to diagnose viral pneumonia. In many patients, fortunately, the infection occurs without pneumonia or with minimal damage to the lungs. There is no need to do a CT scan “just for fun”.
As with the coronavirus test (PCR), the mere detection of signs of the disease on a CT scan, even bilateral pneumonia, will not in any way affect what needs to be done next. With Covid-19, even in the mildest patients, CT scans sometimes reveal bilateral pneumonia, which subsequently resolves on its own. Additionally, CT scanners are often not properly disinfected, and even if you don't have Covid-19, you can contract it in the CT scanner, in the waiting area, or from interacting with staff.
A CT scan should be done only when the condition is quite severe and the issue of hospitalization is being discussed, when the patient has signs of hypoxia, that is, oxygen starvation of the body.
3. In what cases are hospitalization and examination still necessary?
Hospitalization and examinations for coronavirus (PCR, CT scan of the lungs) are indicated only for seriously ill patients, when there is a question about oxygen support or treatment in an intensive care unit. Only 20% of infected people require hospital care.
The following symptoms are a cause for concern and to seek medical help:
1) Severe shortness of breath* (feeling of lack of air) - respiratory rate more than 24 cycles per minute;
*Shortness of breath is classified according to severity:
Mild—shortness of breath that does not interfere with daily activities (for example, mild shortness of breath when climbing one or two flights of stairs or when walking briskly);
Moderate—shortness of breath that limits daily life (for example, shortness of breath that limits the ability to climb stairs without needing to rest, or interferes with cooking and light housework);
Severe—dyspnea that causes shortness of breath at rest, makes the patient unable to speak in complete sentences, and interferes with simple activities such as washing or dressing.
2) High temperature
39 and above, which does not decrease while taking antipyretics and persists for a long time (more than 7 days);
3) Decreased blood oxygen saturation levels
Blood oxygen saturation is measured using a pulse oximeter, a small device worn on the index or middle finger of the hand. It shows your oxygen saturation percentage and gives your heart rate. A blood oxygen saturation level of 94% or lower is a sign that the lungs are not coping with their function and the patient needs oxygen support.
4) Impaired consciousness
lethargy, disorientation in space and time.
5) Decrease or sharp increase in blood pressure
below 90 mm Hg or 220 mm Hg and above
6) Increased heart rate
above 130 per minute
7) Presence of additional risk factors
age 65+, concomitant cardiovascular diseases, diabetes, obesity, cancer, etc.
 Other severe symptoms
Other severe symptoms
for example, unbearable pain, in particular headaches, uncontrollable vomiting, incessant diarrhea.
* The combination of two or more signs indicates the need for hospitalization. You must report your condition to your local doctor (general practitioner) at the clinic to which you are attached, or call an ambulance.
Seeking medical help in order to prevent a worsening condition or prevent complications, as we always do with other diseases, unfortunately does not work in the case of coronavirus infection. Medical workers cannot help you from this point of view; the course of the disease and its outcome depend only on your immune system. Moreover, unnecessary contacts with medical workers without any serious reasons for this not only will not bring you any benefit, but also poses a risk of catching a real coronavirus infection if you previously had a regular viral or bacterial infection.
4. I have a negative test for COVID, but a CT scan shows double pneumonia. How is this possible?
The sensitivity of COVID tests is highly dependent on the correct nasopharyngeal swab. Not all health care workers can correctly collect a smear from the back of the throat. The result also depends on the quality of PCR diagnostics.
The sensitivity of CT is many times higher. Already in the emergency room, having seen the typical clinical picture and changes on a CT scan of the lungs, doctors are 99.9% confident in the diagnosis. Smear data have statistical (epidemiological) significance, but are absolutely not needed to determine treatment tactics.
5. What if I don’t have coronavirus pneumonia, but regular pneumonia, and they take me to a Covid hospital and I get infected.
Doctors try to minimize these risks at the triage level, but in the current conditions, pneumonia really won’t be taken to a regular hospital. However, the frequency of such an error is less than 1%; ordinary community-acquired pneumonia is now very rare (they can be distinguished by CT).
6. Are the lungs always affected?
Coronavirus infection can occur in different forms and lung damage does not always occur. Often the disease occurs completely without symptoms, that is, even with a positive test result for coronavirus, a person does not feel any symptoms, and when examining such a carrier, no changes in the body are revealed. This condition is called asymptomatic carriage.
If symptoms are present, the following forms of the disease are distinguished:
• coronavirus infection with damage to the upper respiratory tract (rhinitis, pharyngitis)
• coronavirus infection with damage to the lower respiratory tract (pneumonia).
In the latter case, lung damage is observed. But in most patients the disease proceeds without damage to the lungs.
7. I am sick, and I have small children, I cannot isolate myself from them. What to do?
In close contact with children, it is almost impossible to avoid infection. If you are unable to self-isolate, expect your children to also catch the infection because the virus is highly contagious. Even constant protective measures: hand washing with soap, masks, sanitizers, saline solutions will not be able to prevent the transmission of infection when staying in the same area.
But at the same time, you need to know that children mostly experience COVID-19 asymptomatically or in a mild form. Symptoms such as a runny nose, mild fever, sore throat, and loose stools may develop, but in most cases children feel well and do not experience, compared to adults, severe malaise, weakness, or lack of appetite. If symptoms develop, you need to adhere to symptomatic treatment: give the child plenty of fluids, wash the nose with saline solution, and if the body temperature rises above 38.5 C - children's paracetamol.
According to research, newborns and adolescents are at risk. Scientists are still exploring theories and there is no definitive explanation yet.
INPATIENT CARE
8. What is the treatment in the hospital?
There is nothing special to treat in hospitals, since there are no drugs for Covid-19 proven to be effective and safe.
The hospital can help you cope with the complications of Covid-19: first of all, respiratory failure, which is expressed in a decrease in the level of oxygen in the body, which is manifested by severe shortness of breath. Breathing problems occur if the virus enters the lungs and causes pneumonia there. Severe shortness of breath prevents a person from walking, even sitting and talking.
Blood oxygen saturation levels can be determined using a pulse oximeter. Emergency specialists, hospital doctors and some local police officers have these devices. Oxygen saturation for an adult below 94%, as well as a respiratory rate greater than 24, indicates the need for hospitalization and oxygen inhalation through nasal tubes (cannulas).
Droppers help seriously ill patients who cannot drink themselves to reduce dehydration, establish parenteral nutrition and administer certain medications to them. In hospitals, antibiotics are administered intravenously and antiviral tablets are given.
If oxygen inhalation does not help, transfer to artificial ventilation (ALV). Approximately 5% of infected people require intubation. In this case, the prognosis is poor (mortality rate is about 80%). Also, in severe patients, the formation of blood clots increases. This thrombosis is treated with special medications - so-called direct anticoagulants. Also, only severe patients who have developed acute respiratory distress syndrome (ARDS) and “cytokine storm” are given immunosuppressants such as dexamethasone tablets or intravenous bolus. In some countries, monoclonal antibodies are available to treat ARDS.
9. My relative was admitted to the hospital, but he complains that he is not examined or treated in any way!
Hospitalization for coronavirus infection is an issue that is still controversial, that is, the indications for hospitalization of patients are being reviewed and changed. If at the beginning of the spread of the disease in our country everyone who was diagnosed with coronavirus by laboratory methods was hospitalized, now, due to the overload of hospitals, they began to resort to hospitalization for more specific indications.
It is important to note that even if beds are available, hospitalization in most cases (up to 85% of cases) is not indicated. This is due to the fact that there is no specific treatment for covid infection, and hospital stay does not bring any additional benefit to the patient. The situation may also develop in such a way that instead of benefits there will be negative consequences (constant contact with patients, taking severe toxic drugs).
Thus, hospitalization is indicated only in severe cases, when the patient requires oxygen support through stationary equipment for respiratory failure. How does a patient in hospital due to coronavirus infection feel? Patients find themselves in a very unusual and even frightening environment, which is strikingly different from the usual hospital, where they usually receive a lot of examinations, consultations, intimate advisory conversations, etc. The current COVID hospitals have been repurposed specifically for the treatment of COVID-19. Doctors try to take into account the patient’s concomitant diseases, but do not always have the opportunity to fully treat them.
The treatment does not involve many droppers and injections. For patient safety, most drugs are given in tablets. Anticoagulants (blood thinners) are mainly prescribed in injectable form. The main method of treatment in a hospital is oxygen support of varying degrees of intensity.
Therefore, from the patient’s perspective, the treatment process really does not look very exciting: oxygen from the wall, a handful of tablets, 1-2 subcutaneous injections per day and a pulse oximeter on the finger 3 times a day. And the doctor’s talkativeness in a respirator is significantly reduced.
10. My relative is in the hospital, how can I help him?
What NOT to do:
— Don’t try to get a doctor’s personal contact. Most likely, no one will give it to you, and that’s right. In the current conditions, the working day in the zone is extremely busy, and being distracted by conversations is very unproductive.
— There is no need to demand from the doctor a more comfortable accommodation for your relative, because our hospitals, as a rule, are ordinary, of Soviet origin, and in this situation the situation is not so important.
What to do:
— Help provide the patient with all hygiene products and hand over the necessary things. If you have your own pulse oximeter, glucometer, tonometer, thermometer, then this will be useful for the patient, since in our hospitals there are often cases of breakdowns and it is better to have your own devices with you.
— Provide the patient with all necessary medications to treat his underlying chronic diseases.
— Through the patient himself, convey to the doctor information about your readiness to purchase additional medications (as a rule, we are talking about anticoagulants). Not all hospitals have enough of them for 100% of patients. Please note that the doctor himself will almost never ask you to purchase medications.
11. How not to panic when so many people have died?
We say that there is no need to panic, because panic itself can provoke rash and dangerous actions on your part. For example, if you have any symptoms from the respiratory tract, you will rush to go to the hospital and call an ambulance.
In a state of panic, you will not be able to objectively assess your condition. Alarmists not only complicate the work of the healthcare system, doctors, but, above all, their own lives.
By going to the hospital, testing centers, CT scans, you increase the risk of infection if you do not have COVID. If there is a positive PCR test or symptoms of COVID, 80% of people have either asymptomatic or mild illness, and only 20% require hospital care. It is necessary to understand that in addition to the fact that hospitals in Kazakhstan are overcrowded, hospitals are not equipped at the proper level: only 3-5% of beds are provided with oxygen, monitors, and ventilators. Moreover, there are not enough doctors and nurses, as many have become infected and are sick themselves. That is why you should not panic and take rash actions.
RECOVERY, RE-INFECTION, TREATMENT AFTER
12. If a person already has COVID and is recovering, do they need to be isolated from another person with COVID?
If you have been diagnosed with coronavirus, then you must stop contact for 2 weeks with everyone who does not have this virus. You cannot go outside, go to the store, communicate with relatives, loved ones, children and the elderly. If a family member or someone close to you also tested positive for coronavirus at the same time as you, then you can communicate with each other. If this person’s virus was detected later, and you have already recovered and were ill earlier (a week or two or more), then contact with a “fresh” infected person is undesirable.
13. Can people who have been ill get sick again?
In response to infection, the body produces antibodies. Antibodies are proteins that help fight infections and usually provide protection against getting sick again (immunity). Antibodies are specific for the disease. For example, antibodies against measles will protect a person who has been exposed again to someone with measles, but will not work if the person contracts the flu.
COVID-19 is a new infection. Antibodies are also produced in response to this virus. But how persistent they are, whether they can prevent re-infection and for how long is not yet known for sure. Therefore, there is no reliable data yet on whether re-infection is possible. This issue is currently being studied.
14. It seems to me that I have already had coronavirus, because in January-March I had a severe cough. Do I need to take a blood test for antibodies?
If you have these symptoms, it is possible that you have suffered a coronavirus infection, although in January it was not yet widespread in our country (unless you arrived from China). Taking blood tests for antibodies in your case does not have any important meaning. Firstly, the sensitivity and specificity of these tests have not been sufficiently studied, that is, it is unknown how accurately they will confirm that you have encountered a coronavirus infection. Secondly, there is still no answer to the question of how strong immunity is formed in those who have recovered from coronavirus. That is, even if antibodies to coronavirus are detected in your blood, this does not guarantee you complete protection from re-infection, which means you must still take all measures to prevent infection - just like other people in your environment.
15. How to be treated after suffering from Covid?
We ourselves would like to know the answer to this question. The long-term consequences of COVID-19 appear to be manifested in different organs. This includes pulmonary fibrosis, myocarditis, and much more. As for pulmonary rehabilitation, we can talk about standard breathing exercises (these techniques can be found on the Internet). Just don't blow up the balloons!
16. Tell us about blowing up balloons?
Inflating balloons is a training of the respiratory muscles with increased resistance during exhalation. This is useful for asthma and COPD (chronic obstructive pulmonary disease), so that patients learn to exhale for a long time. Because with these diseases the lumen of the bronchi narrows.
With Covid, this is not necessary: in this case, it is more important to practice inhalation, because the bronchi do not suffer, but the alveoli suffer, and the respiratory surface decreases. Gas exchange suffers. With breathing exercises, we seem to expand this surface for oxygen exchange and prevent inflammatory fluid from filling the alveoli.
POPULAR DRUGS, TREATMENT PROTOCOLS, ETC.
17. Nowadays there is a lot of talk about the benefits of anticoagulants for COVID. Should I take them for prevention?
No need. Anticoagulants do not prevent or treat the infection itself. They will help with the development of complications in the form of thrombosis. Increased formation of blood clots due to the fact that the virus has penetrated into the arteries and veins occurs extremely rarely, and only in seriously ill patients who are in the hospital, especially in intensive care. Very “serious” injection medications are used for treatment. Such as heparin and its derivatives. These medications require monitoring the state of the coagulation system using multiple indicators.
18. Are the popular drugs that many people are now actively buying effective in the fight against COVID-19?
The effectiveness of drugs such as nobasit (enisamia iodide), ingavirin (imidazolylethanamide of pentanedioic acid), interferon in the nose (leukocyte interferon human or powder for solution, or in solution), arpeflu (umifenovir hydrochloride) has not been proven. All of these drugs are claimed to be antiviral, but have not undergone randomized clinical trials and are not used in countries where evidence-based medicine is accepted.
We recommend using words such as “immunomodulatory effect,” “strengthening the immune system,” or “protector” of something as a “red rag” in the instructions for medications. These very unscientific and vague concepts are often used by manufacturers of unproven drugs and dietary supplements.
Tamiflu (oseltamivir), Relenza (zanamavir) and inavir (laninamivir) only work against the influenza virus (the season will be in winter), but many are now mistakenly taking these medications for coronavirus.
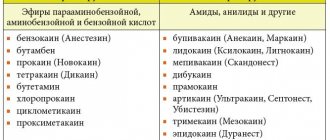
Nimesil is the commercial name of nimesulide, one of dozens of non-steroidal anti-inflammatory drugs, which also include aspirin, ibuprofen, paracetamol, sodium diclofenac, etc. You should not take nimesil if you suspect you have COVID, because it failed the safety test. Today, for very severe pain in muscles, bones, and poor tolerance to very high temperatures, taking only two drugs is justified: paracetamol (acetominophen is its other international nonproprietary name) and ibuprofen.
Sumamed (international nonproprietary name azithromycin), ceftriaxone and any other antibiotics should not be taken by people with coronavirus infection, because you disrupt your microbiome (destroy beneficial microbes in the intestines and nasopharynx), contributing to the development of antibiotic resistance. No antibiotics work on viruses! They are not only useless, but harmful for viral infections. They will be prescribed to you if you are seriously ill with COVID and are in intensive care under intubation, only to prevent a secondary bacterial infection that is carried into the lungs during intubation.
19. A certain protocol for the treatment of coronavirus infection is being actively sent out via WhatsApp, where people are prescribed to immediately take antibiotics and antiviral drugs. Is it correct?
You should not rely on mailings with protocols for the treatment of covid infection or on any other sources of information advising you to take certain antiviral drugs or antibiotics.
Unfortunately, today there is no specific treatment for covid infection. This means that there is not a single drug with proven effectiveness that would prevent the development of the disease or help stop the course of the disease and lead to a faster recovery, so there is no need to take antiviral drugs or antibiotics from the first days of the disease. There will definitely be no benefit from this, but the side effects of these medications are real, and they can worsen your well-being and the course of the disease.
Drugs against the virus and antibiotics in case of secondary bacterial infection are prescribed by the doctor. For this, there are strict indications that he follows when treating seriously ill patients in a hospital. And even in these cases, treatment is often empirical (experimental) in nature, and there is no guarantee that the drugs will work in any particular case.
20. Is it true that ibuprofen can cause complications?
Indeed, early in the pandemic, articles were published that noted that COVID patients who took ibuprofen were more likely to die or have complications. However, subsequent studies completely vindicated ibuprofen.
Moreover, randomized controlled trials have been conducted which have shown that ibuprofen, taken for severe muscle pain, headaches or poor temperature tolerance, is not only safe, but also has an advantage over other similar drugs.
21. Will activated carbon help against the virus?
Some people use activated charcoal for all illnesses. Let's look at what activated carbon is.
Here is what Wikipedia writes: “Activated carbon is a porous substance that is obtained from various carbon-containing materials of organic origin: charcoal (brands of activated carbon BAU-A, OU-A, DAK[1], etc.), coal coke (brands of activated carbon coal AG-3, AG-5, AR, etc.), petroleum coke, coconut shells and other materials. It contains a huge number of pores and therefore has a very large specific surface area per unit mass, as a result of which it has a high adsorption capacity.”
This means that coal, which we sell in black tablets of 0.25 and 0.5 g, is a porous substance, that is, it has the ability to absorb (adsorb) liquids, in particular gastric juice and the poisons it contains. Coal will work as an antidote in the lumen of the stomach and further in the intestines. In medicine, activated carbon is used in large doses (50-100 grams) in the form of a powder, which is mixed with water and given in one gulp, in case of drug overdose, poisoning, in order to reduce the absorption of the drug taken orally and causing anaphylactic shock.
Now think about where the virus is in an infected person? It does not float in the gastric or intestinal juice. It attaches to the walls of the epithelium of the respiratory tract, less often - the epithelium of the gastrointestinal tract. Having attached, the virus penetrates inside the cells in a matter of minutes and causes our cells to produce similar viruses. And the cells die. So coal, as a chemical absorbent-adsorbent, is absolutely useless.
Day three
It was not possible to sleep. I carry out treatment according to the old procedure, again a combination of paracetamol and nimesil, because my head hurts.
I decided that the main cause of lack of sleep was pulmonary obstruction. After all, everyone writes about it. This is logical: the pulse is high, since the heart cannot cope, the cough is strong, a feeling of shortness of breath, in general, there is little oxygen in the blood.
I feel bad. The heart seizes, the pulse does not calm down. I order home delivery of an oximeter. If the saturation is low, I will call an ambulance.
They brought an oximeter, measurements showed a saturation of 95-97 units. Almost normal. But why am I not sleeping? There is a noise in my ears, but my consciousness is surprisingly clear. I try to fall asleep a million times, the cough torments me, but not too much, it’s a hell of a headache.
And again I “repeated” taking paracetamol and Nimesil that day. Can you guess what caused the insomnia?
My heart was already hurting constantly, the pain went away when I took the next “bag”.
Differences
Paracetamol is the only NSAID that selectively affects the synthesis of cyclooxygenase type 3 (COX-3). This biologically active substance is involved in the mechanism of pain and fever, but unlike cyclooxygenases types 1 and 2, COX-3 is not synthesized directly at the site of inflammation.
Suppression of COX-3 synthesis by paracetamol leads to a decrease in elevated temperature during fever and a decrease in pain, but has virtually no effect on the intensity of the inflammatory reaction directly at the site of inflammation. Therefore, it is advisable to use paracetamol as an antipyretic and mild pain reliever.
Nimesulide, the active ingredient of the drug Nimesil, is a predominant inhibitor of cyclooxygenase type 2 (COX-2). Suppression of the synthesis of COX-2, with a weak effect on COX-1, distinguishes nimesulide from other anti-inflammatory drugs by a number of positive qualities: less gastro- and nephrotoxicity, less effect on blood clotting. Another positive quality of the drug is its ability to inhibit the activity of enzymes that damage cartilage cells, which slows the progression of osteoarthritis.
Paracetamol is used in pediatric practice for the symptomatic treatment of pain and fever in children of the first years of life.
In pediatric practice, paracetamol is used for the symptomatic treatment of pain and fever in children of the first years of life. The use of nimesil in children is allowed from 12 years of age.
Day four
During the next night vigil, I began to analyze the intake of all the drugs that I took.
And here a quote from the instructions for Nimesil pops up:
Contraindication is concomitant (simultaneous) use of drugs with potential hepatotoxicity, for example, paracetamol...
Then I read the side effects that paracetamol gives:
Mental disorders (often) – insomnia, anxiety. From the nervous system - headache, dizziness, psychomotor agitation, disorientation.
So Nimesil, together with paracetamol, somehow led to persistent insomnia
. Truly narcotic, endless, irresistible.
In addition, gastrointestinal disorders were observed. Wild thirst, which I, again, attributed to the temperature. Constant runs to the toilet.
I realized that any more and I would have had a heart attack. And it is still unknown how my experiments will turn out in the future. I hope there will be no consequences.
conclusions
A combination of paracetamol and nimesil can cause kidney cancer, liver damage, and gastrointestinal bleeding.
Overall, the very powerful energizing effect that I have discovered the hard way feels equivalent to drinking several cups of strong latte. Perhaps, if a person does not have a cold and is absolutely healthy, he may even experience some positive aspects from the compatibility of these drugs. In any case, consciousness and mental activity remain very clear even after the third night.
What can I say finally? Do not mix different medications. Even paracetamol with aspirin. Remember that this is truly deadly.
Recently, ibuprofen has been increasingly used for viral diseases, coronavirus, and tracheobronchitis. It lowers the temperature and has an anti-inflammatory effect.
As for paracetamol, it should be used only as a single dose, and only by people with a healthy liver.
Is it possible to take Nimesil and Paracetamol at the same time?
The combination of Paracetamol with other non-steroidal anti-inflammatory drugs allows you to obtain a stronger analgesic effect, which can increase the effectiveness of pain relief in the acute phase of diseases accompanied by severe pain (for example, postoperative pain, strangulated intervertebral hernia).
However, simultaneous administration of Paracetamol with nimesulide may increase the risk of hepatotoxicity. Therefore, if it is necessary to use these drugs together, it is necessary to use minimal doses of Paracetamol.