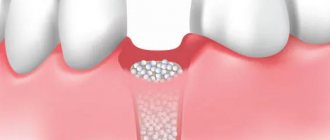
Osteoplasty in dentistry is the augmentation of bone tissue necessary for successful implantation. After a person has a tooth removed, the hard tissue tends to dissolve, and the new artificial tooth must be held securely in the jaw. Bone augmentation for dental implantation successfully solves this problem, but requires additional costs and more time (than, for example, with one-stage implantation, when the tissue volume is sufficient).
Osteoplasty – what is it and why is it needed?
When introducing a titanium root, it is very important that it is surrounded on all sides by bone. If there is a deficiency of tissue, the titanium pin will be rejected. Moreover, if the root is installed in the upper jaw, there is a risk of touching the maxillary sinuses, which can lead to serious ENT diseases. Also, if there is insufficient bone, the implant will become loose and sink below the gum, which will affect the aesthetics of the prosthesis and the overall picture.
Osteoplasty is recommended in the following cases:
- if it is necessary to install a root in an area where a tooth was removed several years (or months) ago;
- if the patient has anatomically large maxillary sinuses;
- when physiologically a person has a minimum volume of hard tissue.
The operation is not performed if:
- the patient has chronic ENT diseases (sinusitis, sinusitis, rhinitis);
- lack of calcium in the body;
- there are pathologies in the structure of the respiratory system;
- oncology;
- polyps and other formations in the nose;
- diabetes.
Also, osteoplasty is not performed on pregnant and lactating women. Otherwise, the operation is done relatively quickly and with a guarantee.
In many cases, patients are recommended to take a course of hormonal medications and antibiotics before surgery in order to neutralize edema and possible inflammation.
How does the violation occur?
Again, I wrote about this. I recommend reading it>>.
The body perceives any surgical operation, including tooth extraction, as an injury and reacts to it with an appropriate reaction, inflammation.
Inflammation is a complex pathophysiological process consisting of several smoothly flowing stages:
During inflammation, a number of biologically active substances (BAS) are released, triggering phagocytosis, in which osteoclasts and other macrophages participate. They destroy everything that they consider damaged (and everything damaged is marked in advance with special compounds, antibodies).
Thus, the process of osteolysis - osteoclasts eat bone tissue, it decreases in volume. And everything would be very sad if osteoclasts did not die from their gluttony - when they die, they secrete a whole series of mediators, the so-called. Bone Morphogenetic Proteins (BMP) or, in foreign languages, BMP (Bone Morphogenetic Proteins), which activate the reproduction and differentiation of fibroblasts and osteoblasts. In other words, they trigger osteogenesis, the growth of new bone:
And here we need to make a couple of important notes:
– the main biologically active substances that trigger phagocytosis (cytokine proteins, etc.) are released during the alterative stage of inflammation, which is known for its violent symptoms. Yes, friends, swelling, pain, increased temperature of the injured area - all this happens in the alteration phase.
– yes, we are all afraid of pronounced post-operative (read, “inflammatory”) symptoms and do a lot to ensure that they are as mild as possible. But an interesting fact is that a weakly expressed alteration stage will not provide the required amount of biologically active substances to trigger osteoclasts, and they, in turn, to regenerate bone tissue. Thus, there is a direct positive relationship between the symptoms of the postoperative inflammatory process and subsequent regeneration: the more pronounced the alterative stage of inflammation, the more factors that control osteogenesis are released.
In fact, the post-traumatic inflammatory process throws our osteolysis-osteogenesis equation out of balance - due to the increased activity of bone-eating cells, osteolysis outweighs:
Fortunately, this process does not last long. Gradually, all processes are balanced again, the rate and degree of osteolysis is almost equal to the degree and rate of osteogenesis.
And the process of atrophy slows down. If we tie it to time and draw a graph, we get the following:
Simply put, the greatest amount of bone loss occurs in the first 4-8 weeks after tooth extraction. Then, the process slows down - and, taking a period of time from 18 to 24 months after removal, we are surprised to note that the linear dimensions of the bone practically do not change:
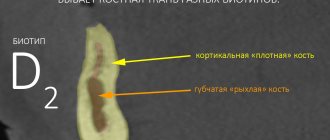
But let’s return to bone tissue biotypes.
If there is a relationship between the biotype of the alveolar bone and its regenerative capabilities (osteogenesis), then, obviously, there is a relationship between the biotype and the rate of bone atrophy. And you have observed this many times - let’s say, if we see a very strongly atrophied alveolar ridge, then, as a rule, it is of the D1-D2 biotype, and if the shape and volume of the jaw bone after the loss of teeth practically does not decrease over a long period of time, then by 146% D3-D4.
And this is easy to explain, knowing that the bone tissue of the D3-D4 biotype is better supplied with blood, there are more osteoblasts in it, and metabolic processes in it are more intense. Significant atrophy of such an alveolar ridge that requires osteoplasty occurs rarely and, as a rule, only in cases of very, very, very traumatic tooth extraction, or against the background of a chronic inflammatory process, when osteoclasts and other macrophages are active for a very, very, very long period of time .
Types of bone tissue in dentistry
- allograft is synthetic bone tissue in dentistry, which is created in the laboratory. This is an artificial material that does not always take root successfully;
- intraoral autograft – the patient’s own bone tissue, which was taken from other areas of the oral cavity. For example, from the farthest part of the dentition. This augmentation procedure is called autotransplantation;
- allogeneic bone material in surgical dentistry is human bone, the donor of which is another patient. High survival rates, but the patient may be confused that this material was taken from a cadaveric bone, although it was stored in sterile packaging;
- Xenograft is a bone tissue substitute in modern dentistry, a material of animal origin. Borrowed from cattle bones. One of the most popular materials for transplantation when a large volume of hard tissue is required;
- Hydroxyapatite granules are an artificial bone graft in dentistry.
An experienced dentist-implantologist will help you determine the specific type of bone material in dentistry, who will study the patient’s condition, the characteristics of the tissue and evaluate the future scope of work on restoring the dentition.
Bone is a complex matter; it is a complex anisotropic, uneven living material with elastic and viscous properties, as well as a good adaptive function. All the excellent properties of bones are inextricably unified with their functions.
The function of bones mainly has two sides: one is the formation of the skeletal system, which is used to support the human body and maintain its normal shape, as well as to protect its internal organs. The skeleton is the part of the body to which muscles are attached and which provides the conditions for their contraction and body movement. The skeleton itself performs an adaptive function by consistently changing its shape and structure. The second side of the function of bones is to maintain the balance of minerals in the human body, that is, the function of hematopoiesis, as well as the preservation and exchange of calcium and phosphorus, by regulating the concentration of Ca2+, H+, HPO4+ in the blood electrolyte.
The shape and structure of bones vary depending on the functions they perform. Due to their functional differences, different parts of the same bone have different shapes and structures, for example, the diaphysis of the femur and the head of the femur. Therefore, a complete description of the properties, structure and functions of bone material is an important and challenging task.
Bone structure
“Tissue” is a combined formation consisting of special homogeneous cells that perform a specific function. Bone tissue contains three components: cells, fibers and bone matrix. Below are the characteristics of each of them:
Cells: There are three types of cells in bone tissue: osteocytes, osteoblast and osteoclast. These three types of cells interchange and combine with each other, absorbing old bones and generating new bones.
Bone cells are found within the bone matrix, these are the main cells of bones in normal condition, they have the shape of a flattened ellipsoid. In bone tissue, they provide metabolism to maintain the normal state of bones, and under special conditions they can turn into two other types of cells.
Osteoblast is cube or dwarf column shaped, they are small cellular projections arranged in a fairly regular pattern and have a large and round cell nucleus. They are located at one end of the cell body, the protoplasm has alkaline properties, they can form intercellular substance from fibers and mucopolysaccharide proteins, as well as from alkaline cytoplasm. This results in the precipitation of calcium salts into needle-shaped crystals located among the intercellular substance, which is then surrounded by osteoblast cells and gradually turns into osteoblast.
Osteoclasts are multinucleated giant cells, their diameter can reach 30–100 µm, they are most often located on the surface of absorbed bone tissue. Their cytoplasm is acidic in nature; inside it contains acid phosphatase, which is capable of dissolving bone inorganic salts and organic substances, transferring or throwing them to other places, thereby weakening or removing bone tissue in a given place.
The bone matrix is also called the intercellular substance and contains inorganic salts and organic substances. Inorganic salts are also called inorganic bone constituents, their main component being hydroxyl apatite crystals about 20-40 nm long and about 3-6 nm wide. They mainly consist of calcium, phosphate radicals and hydroxyl groups forming [Ca10 (PO4) (OH)2], on the surface of which there are ions Na+, K+, Mg2+, etc. Inorganic salts make up approximately 65% of the total bone matrix. Organic substances are mainly represented by mucopolysaccharide proteins that form collagen fiber in bone. Crystals of hydroxyl apatite are arranged in rows along the axis of collagen fibers. Collagen fibers are arranged unequally, depending on the heterogeneous nature of the bone. In the interlacing reticular fibers of bones, the collagen fibers are bundled together, but in other types of bones they are usually arranged in orderly rows. Hydroxyl apatite binds together with collagen fibers, which gives the bone high compressive strength.
Bone fibers are mainly composed of collagen fiber, so it is called bone collagen fiber, the bundles of which are arranged in layers in regular rows. This fiber is closely connected to the inorganic constituents of the bone to form a board-like structure, hence it is called lamella or lamellar bone. In the same bone plate, most of the fibers are located parallel to each other, and the layers of fibers in two adjacent plates intertwine in the same direction, and the bone cells are sandwiched between the plates. Due to the fact that the bone plates are located in different directions, the bone substance has quite high strength and plasticity, it is able to rationally perceive compression from all directions.
In adults, almost all bone tissue is presented in the form of lamellar bone, and depending on the shape of the location of the bone plates and their spatial structure, this tissue is divided into dense bone and spongy bone. Dense bone is located on the superficial layer of abnormal flat bone and on the diaphysis of a long bone. Its bone substance is dense and strong, and the bony plates are arranged in a fairly regular order and closely connected to each other, leaving only a small space in some places for blood vessels and nerve canals. Spongy bone is located in its deep part, where many trabeculae intersect, forming a mesh in the form of a honeycomb with different sizes of holes. The holes of the honeycomb are filled with bone marrow, blood vessels and nerves, and the location of the trabeculae coincides with the direction of the lines of force, so although the bone is loose, it is able to withstand a fairly large load. In addition, cancellous bone has a huge surface area, which is why it is also called bone, which is shaped like a sea sponge. An example is the human pelvis, the average volume of which is 40 cm3, and the surface area of dense bone is on average 80 cm2, while the surface area of trabecular bone reaches 1600 cm2.
Bone morphology
In terms of morphology, bones vary in size and can be classified into long bones, short bones, flat bones and irregular bones. Long bones are tube-shaped, the middle part of which is the diaphysis, and both ends are the epiphysis. The epiphysis is relatively thick, has an articular surface formed together with neighboring bones. Long bones are mainly located on the limbs. Short bones have an almost cubic shape, most often found in parts of the body that experience quite significant pressure, and at the same time they must be mobile, for example, these are the bones of the wrists and the tarsal bones of the legs. Flat bones have the shape of plates; they form the walls of bone cavities and play a protective role for the organs located inside these cavities, for example, like the bones of the skull.
Bone consists of bone substance, marrow and periosteum, and also has an extensive network of blood vessels and nerves, as shown in the figure. The long femur consists of a diaphysis and two convex epiphyseal ends. The surface of each epiphyseal end is covered with cartilage and forms a smooth articular surface. The coefficient of friction in the space between the cartilages at the joint junction is very small, it can be below 0.0026. This is the lowest known frictional force between solid bodies, allowing cartilage and adjacent bone tissue to create a highly efficient joint. The epiphyseal plate is formed from calcified cartilage connected to cartilage. The diaphysis is a hollow bone, the walls of which are formed from dense bone, which is quite thick along its entire length and gradually thins towards the edges.
Bone marrow fills the medullary cavity and cancellous bone. In fetuses and children, the medullary cavity contains red bone marrow; it is an important hematopoietic organ in the human body. In adulthood, the marrow in the bone marrow cavity is gradually replaced by fats and yellow bone marrow is formed, which loses its ability to form blood, but the bone marrow still contains red bone marrow that performs this function.
The periosteum is a compacted connective tissue closely adjacent to the surface of the bone. It contains blood vessels and nerves that perform a nutritional function. Inside the periosteum there is a large amount of highly active osteoblast, which during the period of human growth and development is able to create bone and gradually make it thicker. When bone is damaged, the dormant osteoblast within the periosteum becomes active and becomes bone cells, which are essential for bone regeneration and repair.
Bone microstructure
The bone substance in the diaphysis is mostly dense bone, and only near the medullary cavity there is a small amount of cancellous bone. Depending on the arrangement of the bony lamellae, dense bone is divided into three zones, as shown in the figure: annular lamellae, Haversian (Haversion) lamellae and interosseous lamellae.
Annular plates are plates arranged circumferentially on the inner and outer sides of the diaphysis, and they are divided into outer and inner annular plates. The outer ring-shaped plates have from several to more than a dozen layers, they are located in orderly rows on the outer side of the diaphysis, their surface is covered with periosteum. Small blood vessels in the periosteum penetrate the outer ring-shaped plates and penetrate deep into the bone substance. The channels for blood vessels passing through the outer annular plates are called Volkmann's Canal. The internal ring-shaped plates are located on the surface of the medullary cavity of the diaphysis; they have a small number of layers. The inner ring-shaped plates are covered by the internal periosteum, and Volkmann's canals also pass through these plates, connecting small blood vessels with the vessels of the bone marrow. The bony plates concentrically located between the inner and outer ring-shaped plates are called Haversian plates. They have from several to more than a dozen layers located parallel to the axis of the bone. The Haversian plates have one longitudinal small canal, called the Haversian canal, which contains blood vessels, as well as nerves and a small amount of loose connective tissue. Haversian plates and Haversian canals form the Haversian system. Due to the fact that there are a large number of Haversian systems in the diaphysis, these systems are called osteons. Osteons are cylindrical in shape, their surface is covered with a layer of cementin, which contains a large amount of inorganic components of bone, bone collagen fiber and an extremely small amount of bone matrix.
Interosseous plates are irregularly shaped plates located between osteons, they do not have Haversian canals and blood vessels, they consist of residual Haversian plates.
Intraosseous circulation
Bone has a circulatory system, for example, the figure shows a model of blood circulation in a dense long bone. The diaphysis contains the main feeding artery and veins. In the periosteum of the lower part of the bone there is a small hole through which a feeding artery passes into the bone. In the bone marrow, this artery divides into upper and lower branches, each of which further diverges into many branches that form capillaries at the final section that nourish brain tissue and supply dense bone with nutrients.
The blood vessels in the terminal part of the epiphysis connect to the feeding artery entering the medullary cavity of the epiphysis. The blood in the vessels of the periosteum flows out from it, the middle part of the epiphysis is mainly supplied with blood from the feeding artery and only a small amount of blood enters the epiphysis from the vessels of the periosteum. If the feeding artery is damaged or cut during surgery, it is possible that the blood supply to the pineal gland will be replaced by nutrition from the periosteum, since these blood vessels communicate with each other during fetal development.
Blood vessels in the epiphysis pass into it from the lateral parts of the epiphyseal plate, developing, turning into epiphyseal arteries that supply blood to the brain of the epiphysis. There are also a large number of branches that supply blood to the cartilage around the epiphysis and its lateral parts.
The upper part of the bone is articular cartilage, under which is the epiphyseal artery, and even lower is the growth cartilage, after which there are three types of bone: intracartilaginous bone, bony plates and periosteum. The direction of blood flow in these three types of bone is not the same: in the intracartilaginous bone the blood moves upward and outward, in the middle part of the diaphysis the vessels have a transverse direction, and in the lower part of the diaphysis the vessels are directed downward and outward. Therefore, the blood vessels throughout the dense bone are arranged in the shape of an umbrella and diverge in a radial manner.
Because the blood vessels in bone are very thin and cannot be observed directly, studying the dynamics of blood flow in them is quite difficult. Nowadays, with the help of radioisotopes introduced into the blood vessels of the bone, judging by the amount of their residues and the amount of heat they generate in comparison with the proportion of blood flow, it is possible to measure the temperature distribution in the bone to determine the state of circulation.
In the process of treating degenerative-dystrophic diseases of the joints using a non-surgical method, an internal electrochemical environment is created in the head of the femur, which helps restore impaired microcirculation and actively remove metabolic products from tissues destroyed by the disease, stimulates the division and differentiation of bone cells, which gradually replace the bone defect.
Pros and cons of bone grafting during implantation
Competitive advantages of bone grafting:
- restoration of functions, even if the patient has lost a large amount of hard tissue;
- the appearance of the gum tissue and the oral cavity as a whole is normalized;
- restoration of chewing functions - all types of bone tissue in dentistry are adapted to heavy loads;
- the ability to restore teeth, even in the most advanced situations.
Disadvantages of bone grafting:
- rehabilitation takes several months;
- high risk of block rejection;
- pain during tissue engraftment;
- considerable cost of the operation.
Instead of a prologue. What are biomaterials?
From the point of view of the explanatory dictionary, biomaterials mean any foreign substances and objects introduced into the body and complemented by it structurally and/or functionally, and used for medical purposes . That is, biomaterials can be called artificial heart valves, endoprostheses, implants, including dental ones, metal structures used in osteosynthesis, hemostatic agents, dentures, crowns, inlays, fillings, etc. And vice versa, earrings for piercing, Tattoo inks and all sorts of scary things for body modding do not belong to biomaterials, in their correct understanding.
What we use for “bone tissue augmentation” would be more accurately called “biomaterials for regenerative surgery,” which specifies and explains their purpose. In general terms, the modern dental market offers us three categories of such materials - osteografts, barrier membranes and mucografts:
A little later, we will look at each of these categories in detail.
It is quite difficult to talk about indications and contraindications for the use of biomaterials from the patient’s point of view, so their use during certain osteoplastic operations is an issue that relates more to a specific technique than to the material itself. Therefore, we will consider it in articles devoted to certain osteoplasty techniques. That is, soon.
But, in general, dear friends, you need to know the following:
– the use of biomaterials is always a compromise, a necessary measure.
Yes, theoretically and practically, we could do without them. And there are many examples of this:
Let me clarify that the two right pictures show a temporary crown on an installed implant. Biomaterials for osteoplasty were not used in this clinical case.
But in such cases we are faced with a problem - if we need to compensate for the atrophic loss of bone or mucous membrane, then it must be taken somewhere. And often the process of obtaining an autograft (i.e., one’s own fragment of tissue for transplantation) increases the trauma, complexity and duration of surgical intervention. And sometimes it is even a separate surgical operation with all the consequences: the risks of complications increase and the safety of surgical treatment decreases. The desire to avoid all this by replacing the autograft with something “artificial” seems completely logical.
– none of the existing biomaterials improves the quality of regenerating tissues.
This is a microscopic photograph of what happens after osteoplasty using biomaterials.
If we are talking, for example, about “building up bone tissue,” then none of the osteografts used in modern surgical practice makes the bone stronger, stronger, more beautiful, etc. Moreover, what we get as a result of using “artificial bone substitutes” can hardly be called bone in the biological sense - rather, it is a bone callus with the inclusion of particles of biomaterial (as in the microscopic picture above), its properties and structure are very different from normal healthy bone tissue. If we're talking very seriously, the use of grafts “degrades” the quality of the tissue. But we are forced to make this compromise in order to fill their volume and, accordingly, create conditions for normal implantological rehabilitation.
– there are no biomaterials that accelerate tissue regeneration.
I would even say more - little depends on the brand, manufacturer or country of origin of the biomaterial. All grafts and barrier membranes existing in the world work the same way, according to the same biological laws. It is absolutely wrong to say that “this material works better than this one” or “this one is good, but this one is complete crap!” Of course, biomaterials differ from each other in a number of properties, and today we will definitely talk about these properties.
– each category of biomaterials has its own purpose and clearly defined function.
Just like in this picture:
To use biomaterials for other purposes is, at a minimum, to seriously risk the result. For example, we may try using a hemostatic sponge to fill the subantral space during a sinus lift. And perhaps we will even get a good result. But the word “possible” really confuses me personally. In surgery, the use of this word should be kept to a minimum.
– the use of biomaterials must be justified and understandable, first of all, to you.
“We’ll stick it here, we’ll pin it here”... in other words, the use of grafts and barrier membranes is always a great way to inflate the cost of treatment or artificially complicate the upcoming operation. Indeed, installed implants can be counted, their brand and model can be easily determined from control images, but determining the volume of graft de facto used during sinus lifting or the size of the installed barrier membrane (and, in general, the presence of this very membrane) is not so simple. If for some reason you do not understand why the use of biomaterials is necessary in your clinical case, then they are not needed. We will talk about their use in various clinical situations in subsequent articles, when we study each of the existing methods of osteoplasty. Well, after the operation, it makes sense to “check” with the actual consumption of biomaterials - all grafts and barrier membranes used in modern surgery have special stickers indicating their parameters and serial numbers - one sticker remains in the medical record, the second is pasted into the contract, on a control image or a special form that is given to the patient.
Finally, last but not least:
All existing biomaterials are disposable. One package is intended for ONLY one operation:
This, in fact, means that, firstly, unused remnants of biomaterials cannot be re-sterilized and used, and secondly, that the absence of the above sticker indicates that in your treatment, the “left” material or residues of some kind may have been used. - some other operation. I categorically do not recommend saving on this, because it is impossible to properly sterilize already opened material in a regular dental clinic without losing its properties.
In principle, dear friends, knowledge of the above is quite enough to understand whether expensive, generally speaking, biomaterials are needed for bone tissue augmentation specifically in your clinical case. Just in case, I remind you that
if you don’t understand something, then you don’t need it.
Just remember this article >>.
As part of the RegenerationDay by Geistlich seminars, I manage not only to increase my sense of self-importance, but also to talk with doctors from various clinics, cities and regions of our country. And I can’t help but notice a harmful trend - the excessive abuse of biomaterials, the stupid desire to push them where, in principle, they are not needed. Many see them as some kind of panacea, some kind of “magic pill” that can, if not guarantee, then improve the result of any osteoplastic surgery. Alas, this is not true.
A lot of osteoplastic operations are performed in our dental center - more than two hundred since the beginning of the year. At the same time, the consumption of biomaterials is relatively small - they are used in less than half of the cases. Why? To answer this question, you need to at least read this >> or just stop by our clinic for a consultation.))
Human embryo and sperm
It looks like a war of the worlds, but in fact, you have an egg in front of you 5 days after fertilization. Some sperm are still retained on its surface. The image was taken using a confocal microscope. The egg and sperm nuclei are purple, while the sperm flagella are green. The blue areas are nexuses, intercellular gap junctions that communicate between cells.
Work examples
All works
Implantation for 2 jaws with artificial gum
Complete restoration of the upper jaw on implants
Complete restoration of the upper jaw using a zygomatic implant
Stage III periodontal disease: complex dental implantation Restoration of both jaws in 4 days
Sinus lifting with simultaneous implantation
Implantation of both jaws with ROOTT implants for stage II periodontal disease
Restoration of two jaws with one-stage implantation using sinus lift
Sinus lift with simultaneous implantation
All works
Sign up for a consultation
three ROOTT specialists + diagnostics as a gift
Human tissues and organs under a microscope (15 photos)
Almost all of the images presented here were taken using a scanning electron microscope (SEM). The electron beam emitted by such a device interacts with the atoms of the desired object, resulting in 3D images of the highest resolution. Magnification of 250,000 times allows you to see details measuring 1-5 nanometers (that is, billionths of a meter).
The first SEM image was obtained in 1935 by Max Knoll, and already in 1965 the Cambridge Instrument Company offered its Stereoscan. Now such devices are widely used in research centers.
Looking at the pictures below, you will take a journey through your body, starting from your head and ending with your intestines and pelvic organs. You'll see what normal cells look like and what happens to them when they are attacked by cancer, and you'll also get a visual understanding of how, say, the first meeting of an egg and sperm occurs.
Plaque
To avoid deposits on your teeth that look like unthreshed spikelets, it is advisable to brush your teeth more often.
Remember how beautiful healthy red blood cells looked? Now look how they become in the web of a deadly blood clot. In the very center is a white blood cell (leukocyte).
Red blood cells
This is what you might call the heart of your blood, the red blood cells (RBCs). These cute biconcave cells have the responsible task of carrying oxygen throughout the body. Typically, in one cubic millimeter of blood there are 4-5 million such cells in women and 5-6 million in men. People living at high altitudes, where there is a lack of oxygen, have even more red cells.
Purkinje cells
Of the 100 billion neurons in your brain, Purkinje cells are some of the largest. Among other things, they are responsible in the cerebellar cortex for motor coordination. They are adversely affected by alcohol or lithium poisoning, as well as autoimmune diseases, genetic disorders (including autism), as well as neurodegenerative diseases (Alzheimer's, Parkinson's, multiple sclerosis, etc.).
Human embryo implantation
You are present at the beginning of a new life cycle. A six-day-old human embryo is implanted into the endometrium, the lining of the uterine cavity. Let's wish him good luck!
greenword.ru
Other publications:
Correctors for the metabolism of bone and cartilage tissue in combinations, What does bone tissue destruction mean, Atrophy of the bone tissue of the lower jaw is,