NBR is one of the methods of bone augmentation before implantation. Surgery is used to guarantee the primary stability of the implant and eliminate the risk of rejection of the titanium root and the development of tissue inflammation. The lack of bone is filled with a bone substitute, which is secured with a membrane. They use their own or synthetic materials. The method is safe: surgery is performed under local anesthesia, small tissue incisions are made, bone material is grafted, and the process of graft engraftment is monitored.
What is Guided Bone Regeneration
Guided bone regeneration is an operation to compensate for the lack of bone tissue with a substitute, which is secured with a barrier membrane. After the procedure, a framework is formed around the transplant (it is formed by vessels and osteocyte cells that produce new tissue). Natural bone is gradually replacing artificial material.
Extensions using the NDT method are carried out according to classical parameters:
- thickness of the vestibular bone wall (at the cheek) - up to 2-2.5 mm;
- bone thickness between the implant and the root of the adjacent unit - up to 2.5-3 mm;
- The thickness of the bone wall between two titanium roots is up to 3 mm.
Indications
The operation allows you to increase the “necessary” volume for high-quality classical implantation, helps restore the functions of the jaw, and returns the gums to an attractive appearance.
The bone is built up “with reserve”, since after the operation the surface layers will be supplied with a small amount of oxygen due to their lower blood circulation. Therefore, the volume of inevitable tissue resorption is calculated.
In addition to implantation, indications for NRC are:
- rapid restoration of physiological parameters after tooth extraction;
- congenital or acquired defects of the bone around the teeth;
- prevention of tooth displacement, loosening, and loss due to periodontal tissue diseases.
Why does atrophy occur?
What bone materials are used
Osteoplasty involves the use of bone replacement materials. Previously, transplants were used that were not widely used due to frequent rejection of foreign material:
- Allografts
are donated bone from other people. The material was obtained from corpses, processed, sterilized, and stored in bone tissue banks. - Xenografts
are animal bones (cattle, pigs). The material was freed from proteins by heating (to eliminate the possibility of an allergic reaction after transplantation).
We do not use outdated techniques. Nowadays, many synthetic components have been developed that promote the growth of our own bone, which we use to build bone tissue.
Synthetic materials have a high degree of affinity and compatibility with natural bone and are its analogues. These are granular formulations based on:
- calcium phosphates;
- chondroitin sulfate;
- bioglass.
The effectiveness and safety of artificial materials has been confirmed by numerous studies. They are easy to use, take root well, promote the regeneration of your own bone, and are hypoallergenic.
With osteoplasty, a combination of an artificial substitute and a person’s own bone in the form of chips (autograft) is possible. The technique helps preserve the volume of built-up bone tissue and speed up the rate of recovery. The same method helps if you have to grow a large amount of tissue.
If there is a slight shortage, you can only get by with synthetic materials.
Types of membranes
The membrane technique used by the surgeon is needed to isolate the space from fibrous tissue - creating conditions for normal tissue regeneration. There are several requirements for membranes:
- biological compatibility;
- strength;
- prevention of migration of epithelial cells;
- corresponding resorption period.
In practice, two types of membranes are used:
- Resorbable.
They dissolve on their own 6-24 weeks after extension. Membranes are used for small defects (when you need to build up no more than 2 mm) - they do not hold their shape as well as the next type. - Non-resorbable.
They do not dissolve - they are eliminated several months after surgery.
To quickly fuse the artificial material with the jaw bone tissue, in some cases membranes from the patient’s blood plasma are used.
Dental implantology is a relatively young but rapidly developing science. New types of dental implants and biocomposite materials are being actively developed and implemented, and surgical methods are being improved [8, 9, 17, 19, 21, 26, 27, 34].
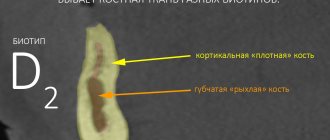
When planning dental implantation, it is necessary to correctly select the location of the implant, the type of implantation system, and evaluate the possible number of implants to be installed. The bone structure of the jaws is of decisive importance, the reliable state of which can only be judged by the results of radiological research methods. At the preoperative stage, it is extremely important to correctly determine the size of the alveolar process of the upper jaw or the alveolar part of the lower jaw, the type of adentia, identify the degree of atrophy of the jaw bone tissue, evaluate its architecture and density to solve the main problems of planning dental implantation and predicting subsequent treatment [16, 24, 34 , 35].
With the help of modern specialized programs for multislice computed tomography (MSCT), it has become possible to obtain dental volumetric tomograms, which allows in difficult situations to correctly plan an implantation operation, select optimal implants and mathematically calculate their installation sites [22-24, 30, 34].
The active development of implantology has shown that treatment results are influenced not only by the doctor’s knowledge and skill in making a diagnosis, preoperative planning and dental implantation, but also by the informed choice of effective and safe supportive drug therapy.
Prescribing a course of antibacterial therapy, anti-inflammatory and desensitizing drugs has become traditional and mandatory in the postoperative treatment regimen for patients.
In outpatient dental practice, non-steroidal anti-inflammatory drugs are most often used for complex therapy of inflammatory processes and pain syndromes in the maxillofacial area, as well as for preventive analgesia before operations and traumatic interventions [4, 5, 7, 10, 11, 20, 29, 33, 37]. Surgical trauma during implantation is accompanied by damage to the alveolar process tissue, which provokes the launch of a cytokine cascade (interleukins, colony-stimulating factors, interferons, tumor necrosis factor-alpha, -beta, tissue growth factor-beta) and the development of an inflammatory reaction. Excessive production of proinflammatory cytokines can lead to a septic state of the wound, as well as to the generalization of the inflammatory process and the development of organ dysfunction. The use of anti-inflammatory drugs before surgery reduces the formation of pro-inflammatory cytokines, which helps reduce postoperative, craniofacial and dental pain, swelling and inflammation. However, when using nonsteroidal anti-inflammatory drugs, adverse reactions may develop. These drugs have a negative effect on the mucous membrane of the gastrointestinal tract, leading to the development of ulcerative processes, reduce platelet aggregation, increasing the possibility of bleeding, predispose to the development of bronchospasm, allergic reactions, decreased diuresis, and the appearance of edema [2, 4, 31, 32, 40 ].
According to statistics, recently there has been an increase in complications from drugs traditionally used for perioperative drug therapy and a significant increase in the number of patients with contraindications to their use.
The increase in complications from drug therapy prompts the search for alternative treatment methods, one of which is homeopathy. The integration of homeopathy into medical practice is facilitated by the creation of complex homeopathic preparations, selected not on the principle of similarity, but on the etiological and pathogenetic principle generally accepted in medicine and familiar to the doctor.
In recent years, complex homeopathic preparations Traumeel S, Osteochel S and Kalkohel have been used in the complex therapy of inflammatory processes in the maxillofacial area [1, 3, 6, 12-15, 18, 25].
The most widely used anti-inflammatory agent in various fields of medicine, including dentistry, is the complex homeopathic preparation Traumeel S, which contains components that influence all parts of the pathogenesis of inflammatory-purulent processes. Traumeel S acts on microcirculation processes, eliminates venous stasis, improves cellular respiration and redox processes, activates the immune system and antimicrobial defense of the body, gives an anti-inflammatory effect, stimulates tissue regeneration, reduces pain and eliminates the consequences of traumatic tissue damage, which allows its use in complex pharmacotherapy of inflammatory-purulent processes and tissue injuries of the maxillofacial area [1, 4, 6, 12-15, 18, 25, 38].
It has been shown that prostaglandins and other metabolites of arachidonic acid, by increasing the mobilization of calcium from bone tissue, promote bone resorption [28, 36, 39]. In this regard, to accelerate regeneration and slow down the process of bone tissue resorption, the drugs Osteochel S and Calcohel were introduced into postoperative complex therapy. Osteochel S improves bone tissue metabolism, optimizes calcium metabolism, and has anti-inflammatory and analgesic effects. Calcohel normalizes metabolism, optimizes the use of calcium in the synthesis of bone tissue, and has an anti-inflammatory, analgesic, and sedative effect [3, 15].
Since practitioners solve problems of varying clinical complexity, it is necessary to improve diagnostic methods, create standardized patient examination schemes for planning bone-reconstructive surgery for bone deficiency, as well as develop a medication support scheme when preparing patients for surgery and in the postoperative period. This will allow you to choose the most optimal surgical method, determine the amount of biomaterial and decide on the stages of operations and medical support for patients. This position should be used in each individual case of plastic surgery for bone deficiency, which will determine different surgical options. Therefore, unified approaches to diagnosis and development of differentiated methods of reconstruction for bone deficiency for dental implantation are required, which was the goal of this study.
Material and methods
This study is based on the results conducted in 2007-2011. osteoplastic surgeries in 356 patients (215 women and 141 men) aged from 25 to 70 years with deficiency of bone tissue of the alveolar process of the jaw for the installation of intraosseous dental implants. There were 203 patients with bone deficiency in the upper jaw and 153 in the lower jaw. To prepare for surgical interventions, a comprehensive examination was carried out: clinical, anthropometric, radiological, and examination of jaw models. Taking into account the functional state of the body allows for an individual choice of methods of preoperative preparation, depending on the presence of concomitant diseases in the patient and the state of the immune status.
Along with the clinical examination, planning of treatment stages was carried out on the basis of radiological diagnostic data. We carried out an initial assessment of the density of osteoplastic materials using computed tomography. To assess the radiological density of osteoplastic materials, we used MSCT and DOT with assessment of the result according to the Hounsfield scale.
The criteria for assessing the results of traditional radiological techniques were similar for all patients. The most difficult task when planning implantation in the lower jaw was assessing the location of the mandibular canal.
When preparing a patient for dental implantation surgery, in some cases it becomes necessary to perform additional bone reconstructive operations in order to restore sufficient volume and shape of the alveolar parts of the jaws. As a rule, such situations are associated with atrophy of the alveolar ridges, post-extraction conditions, and less often with unfavorable anatomical conditions (for example, a critically low location of the lower wall of the maxillary sinus). The main types of such operations are plastic surgery with fixation of the transplant material “onlay” and plastic surgery with fixation of the material inside the bone. Also, if necessary, lateralization of the inferior alveolar nerve or raising the floor of the maxillary sinus (open or closed sinus lift) can be performed. In addition, the use of osteoplastic materials may be necessary during a one-stage implantation operation or to fill a peri-implantation defect in the socket of an extracted tooth. Xenogeneic osteoplastic materials OsteoBiol - “Apatos”, “Gen-os”, “mp3”, “Dual-Block”, as well as their combinations were used as grafts. To close the biomaterial and better adapt it to the bone, the “Evolution” membrane was used.
The results of 6 types of bone grafting operations were studied: subperiosteal transplantation (Group 1), overlay transplantation with bone preparation (Group 2), biomaterial transplantation into the bone (Group 3), reconstruction of the alveolar segment of the upper jaw using access through the alveolar arch with by raising the bottom of the maxillary sinus (4th group), reconstruction of the alveolar process of the maxilla by access through the anterolateral wall with raising the bottom of the maxillary sinus (5th group), reconstruction of the alveolar process and body of the maxilla by access through the distal-lateral wall with raising the bottom of the maxillary sinus (6th group).
All operations were performed on an outpatient basis under conduction or infiltration anesthesia with amide anesthetics using premedication. The follow-up period ranged from 1 to 4 years.
When performing dental implantation, a traditional scheme of medicinal preoperative preparation and postoperative management of patients was used, which included complex homeopathic preparations.
The protocol for preoperative preparation and postoperative treatment of patients included a course of use (21 days) of complex homeopathic medications. Patients used Traumeel S both before implantation and in the postoperative period, and Osteochel S and Kalkohel - in the postoperative period. The drugs were prescribed sublingually, 1 tablet 3 times a day, not combined with other medications or food.
Scheme of medicinal preoperative preparation and postoperative management of patients
Before surgery
patients were prescribed antibacterial and anti-inflammatory drugs.
For 7 days before implantation, patients used the complex homeopathic drug Traumeel S sublingually, 1 tablet 3 times a day.
To prevent infectious complications, 40-60 minutes before surgery, patients were prescribed a single broad-spectrum antibiotic amoxicillin/clavulanate - 2 tablets of 625 mg. If there are contraindications to its use, you can use azithromycin at a dose of 500 mg in combination with metronidazole (500 mg) or clarithromycin (Klacid) at a dose of 500 mg in combination with metronidazole (500 mg).
For preventive analgesia, the nonsteroidal anti-inflammatory drug ketoprofen (150 mg) was prescribed 30 minutes before surgery.
For antiseptic treatment of tissues, a 0.05% chlorhexidine solution was used.
After operation
Patients were prescribed anti-inflammatory and painkillers. Most often, patients used ketoprofen - 150 mg once a day or 50 mg - 3 times a day.
If there are contraindications to the use of ketoprofen, you can use celecoxib - 100 mg 2 times a day or nimesulide - 100 mg 2 times a day.
All patients were prescribed complex homeopathic medications.
Patients used Traumeel S sublingually, 1 tablet 3 times a day in the postoperative period until signs of inflammation disappeared (about 2 weeks).
Osteochel S was prescribed 1 sublingual tablet 3 times a day from the 2nd week after surgery, i.e. The 1st week of its use coincided with the last week of taking Traumeel S. The course of treatment was 21 days.
Patients took Calcohel sublingually, 1 tablet 3 times a day from the 4th postoperative week, i.e. the last week of taking Osteochel S coincided with the first week of taking Calcohel. The course of treatment was 21 days.
For antiseptic treatment of tissues, a 0.05% chlorhexidine solution was used and Metrogil Denta was applied to the seams 3 times a day after meals for 5-7 days.
Antimicrobial chemotherapy drugs were prescribed according to indications.
Amoxicillin/clavulanate at a dose of 625 mg was used 3 times a day. If there were contraindications to its use, azithromycin 500 mg + metronidazole 500 mg 2 times a day or clarithromycin 500 mg 2 times a day + metronidazole 500 mg 2 times a day were prescribed. The duration of the course is 5 days.
To prevent dysbiosis when using antibiotics, the probiotic Linox was introduced into complex therapy - 2 capsules 3 times a day for 21 days.
According to indications, the antihistamine loratadine was administered as part of complex therapy - 10 mg once a day for 5 days.
For all patients, the preoperative preparation and postoperative treatment protocol included the drugs Traumeel S, Osteochel S and Calcohel according to the scheme we proposed.
Results and discussion
Subperiosteal transplantation was performed in 67 patients. Indications for surgery were insufficient height and width of the alveolar bone and a decrease in the occlusal plane. We used xenogeneic osteoplastic materials OsteoBiol - “Apatos”, “Gen-os”, “mp3”, “Sp-Block”, as well as their combinations. Preference was given to “mp3” due to the simplicity and controllability of the introduction of the material and “Dual Block”, which ensures the rigidity of the profile of the created volume of bone material. After 4-5 months, implants were installed. Osteoconductive materials by this time had not clinically and radiologically restructured into mature bone; osteoinductive - represented dense mineralized bone. A 93% success rate was obtained in all patients.
Overlay transplantation with bone preparation was performed in 42 people. The indication for surgery was insufficient width of the alveolar arch and atrophy of the anterior surface of the alveolar process, which made it impossible to install the implant in the correct position in accordance with the occlusion. For this type of operation, preference was given to the “Dual Block” bone block, which ensured the creation of a rigid profile of the created volume of bone material and well restored the volume of lost bone tissue on the vestibular side of the alveolar part of the jaws. For better fixation, the bone blocks were fixed with bone screws and covered with an “Evolution” membrane. X-ray after 6 months, the border between the maternal bone and the remodeled biomaterial was not determined.
In 2 patients, discrepancy of single sutures was noted in the early postoperative period. The presence of the membrane made it possible to completely preserve the osteoplastic material. After treatment, wound healing was completed successfully. The implants and implant-supported dentures functioned well. In 2 patients, after 2-3 years, due to incisal overlap and functional overload, dentures on implants became mobile and were lost. The remaining 40 patients had good results from the operation.
Biomaterial transplantation into the bone was performed in 41 patients. The indication for surgery was a narrow alveolar arch and the need for its displacement to the vestibular side for correct occlusal relationships. The resulting voids were filled with biomaterial, which was covered with an “Evolution” membrane. For this type of surgery, preference was given to the osteoplastic material “Apatos” and “Gen-os”. Moreover, we used “Apatos” in patients with the 3rd and 4th class of bone tissue density according to Misch, which ensured an increase in the density of the bone regenerate in the future, and “Gen-os” in patients with the 1st class of bone tissue density, which made it possible to obtain a bone regenerate of lower density and created better osseointegration of dental implants in the future. After 6 months, X-ray and MSCT revealed a dense bone structure, the implants were surrounded and tightly fused with bone tissue. In patients in this group, 96% success of the operation was achieved.
The operation of reconstruction of the alveolar segment of the upper jaw using access through the alveolar arch with raising the floor of the maxillary sinus was performed in 52 patients. In all patients, the functioning of the implants in prosthetic structures was good; in 4 people, after 1.5-2 years, a change in denture was needed.
Reconstruction of the alveolar process of the maxilla using an approach through the anterolateral wall with elevation of the floor of the maxillary sinus was performed in 46 patients. Analyzing the remodeling of the biomaterial according to radiographs and MSCT in 17 patients, we noted that by the end of the 4th month the shadow of the bone regenerate was vague, the cortical plate at the bottom of the maxillary sinus was not visible. By the end of the 6th month, a dense structure of the reorganized bone was noted. In 29 patients with simultaneous bone grafting and implantation, X-ray studies, including MSCT, showed that the bone after 6 months had a dense structure, the bone pattern was somewhat blurred. The cortical plate was clearly visible both along the alveolar arch and facing the maxillary sinus. Dynamically, the density of the remodeled bone increased after 2 years. According to MSCT data, the bone mass decreased on average by 2 mm in height and remained unchanged in the horizontal and sagittal planes. All 46 patients with delayed and immediate implantation had positive results.
Reconstruction of the alveolar process and body of the maxilla using an approach through the distal-lateral wall with elevation of the floor of the maxillary sinus was performed in 98 patients. Indications for surgery were: a small amount of bone in the area of the molars, pneumatic type of the maxillary sinus with a low location of the bays, including in the area of the tubercle of the upper jaw. In 62 patients of this group, a two-stage procedure was performed, and in 36 patients, a one-stage bone grafting operation with the installation of implants was performed. In 14 patients, final mineralization of the material did not occur after 12-18 months. However, the functioning of the implants was good.
Of the 615 implants, 606 are functional; 9 implants were removed after 2-3 years due to peri-implantitis.
In patients of groups 4-6, during operations we used the “mp3” material as the most adapted for operations to raise the floor of the maxillary sinus. The bone window was closed with an “Evolution” membrane.
Traditionally, radiological monitoring of the state of the area of reconstructive surgery is carried out twice before the stage of implant installation: immediately after the reconstructive operation and immediately before dental implantation (usually after 5-6 months).
In 299 patients, a traditional regimen of medicinal preoperative preparation and postoperative management was used, which included complex homeopathic medications. In 47 (13.6%) patients with small volumes of surgical interventions and in the presence of contraindications to the use of antibiotics, the use of complex homeopathic preparations made it possible to completely abandon the use of chemotherapeutic agents.
Conclusion
Traditionally, it is believed that the installation of implants is possible only 5-6 months after bone grafting. However, our comparative analysis of two-stage and one-stage bone grafting operations with immediate and delayed installation of implants showed equally good results in all groups.
All biomaterials we used were effective, taking into account the choice of material for a specific clinical case. A combination of osteoplastic material, especially with autologous bone, should be recommended.
The effectiveness of the operation for reconstruction of the alveolar process of the jaws and dental implantation was determined based on the following signs:
— patient complaints, including the function of an implant-supported denture;
— clinical evaluation of implant-supported dentures;
— the state of the mucous membrane at the neck of the implant, its density, pocket depth, the presence of bleeding when the probe is immersed;
— X-ray picture of the bone around the implant;
— X-ray picture of the remodeled bone;
— the condition of the maxillary sinus in accordance with the patient’s complaints and the condition of the maxillary sinus in X-ray display;
— oral hygiene index.
The criteria for assessing the effectiveness of bone reconstructive surgery over time were as follows:
— location of the osteoplastic material in relation to the cortical plate of the alveolar ridge;
— adherence of the osteoplastic material to the maternal bone;
— degree and rate of neo-osteogenesis and resorption of bone-plastic material;
— volume of biomaterial (compared to a control study performed immediately after bone reconstructive surgery);
- structure, homogeneity and density of osteoplastic material depending on its type (correspondence with normal values).
The results obtained showed that planning and monitoring the effectiveness of bone reconstructive operations were most successful in patients of groups 2 and 3, where radiation examination was carried out using high-tech methods, which at the planning stage made it possible to obtain complete information about the size and shape of bone defects jaws. Specialized software made it possible to estimate the required amount of osteoplastic material for their replacement.
Anatomical and clinical examination of jaws with bone deficiency and volumetric diagnosis of bone atrophy allow us to offer various methods of bone augmentation and various surgical approaches. And only taking into account all the features of each osteoplastic material (structure, chemical composition), resorption time, its radiological characteristics and density, can the effectiveness of the reconstructive operations performed be correctly assessed. Preoperative drug preparation and individual choice of postoperative pharmacotherapy reduce the incidence of postoperative complications and increase the effectiveness of dental implantation.
Thus, individual planning of the upcoming intervention and its medical support allows one to obtain good results with both two-stage and one-stage dental implantation surgery.
NDT stages
The operation is performed under anesthesia. The surgeon acts according to the classical algorithm:
- He cuts the gum along the hole of the lost tooth, makes several cuts on the side - peels off the gum flap.
- Fixes the implant into the exposed bone (if the operation is organized simultaneously with implantation).
- Replaces the missing volume with a graft, covers it with a membrane with a protrusion of 2-3 mm beyond the bone material. If it does not exclude the fact that the membrane is being pressed into the defect, a titanium mesh is placed on top.
- Secures the membrane (with sutures or screws).
- Brings the edges of the wound together and applies stitches.
The operation lasts 1-1.5 hours.
Technique of the procedure
Before surgery, the doctor examines the patient and examines the condition of the oral cavity. Additionally, laboratory tests are carried out to help determine possible contraindications.
Some patients may require treatment of periodontal disease and other pathologies that can cause complications during the recovery process after surgery. Bone regeneration in dentistry is performed in 5 main stages:
- Anesthesia. Surgery is performed under local anesthesia. At the request of the patient, the doctor can perform the procedure under general anesthesia.
- When the anesthetic begins to take effect, the gum is cut in several places. The doctor first determines the places where the bone will be exposed. After the incision, the gum flaps are detached.
- In places where there is no bone tissue, the doctor applies a graft. The material of the bone substitute is previously agreed upon with the patient. A biological membrane is lined on top of the graft.
- The membrane is securely fixed using sutures and special screws that are used in dentistry.
- Suturing loose flaps of gum tissue to close the wound.
The procedure lasts about 1.5-2 hours. If necessary, the doctor can install a titanium mesh before applying the membrane. This is necessary to prevent indentation of the membrane due to the special anatomical structure of the patient’s teeth.
Can it be done simultaneously with implantation?
Two operations are combined into one if the following conditions are met:
- the shape of the defect allows you to correctly install the artificial root in any of the planes;
- when installed, the implant is located within the bone contour (does not go beyond the tangent drawn to the bone line);
- eliminate a horizontal (not vertical) defect.
The implanted implant can become a barrier to the growth of blood vessels and inhibit the formation of new bone. If the implant protrudes beyond the contour of the bone tissue, the risk of developing fibrous tissue with inclusions of the implanted material cannot be ruled out.
Materials used
Installing an implant allows you to restore the root system, but this requires a sufficiently dense base that can fix the artificial pin, which necessitates the use of osteoinductive agents that stimulate regeneration. Double-layer collagen membranes treated with a restorative drug allow you to restore the natural blood circulation cycle. The material used for the manufacture of membranes includes resorbable and non-resorbable elements that differ in functional properties. During directed regeneration, bioactive compounds and distracting compounds are also used - to obtain the optimal combination, doctors combine various elements that help accelerate integration.