This is roughly how teeth were straightened at the end of the 19th century.
In the modern world, it is not customary to die from crooked teeth. The maximum that will happen to you is that it will become unpleasant to open your mouth wide, the jaw joint will fall out, the depreciation costs of periodontal teeth will increase, and you will begin to see the dentist more often.
In principle, 99% of teeth alignment problems today can be corrected without problems. To do this, there are supports that create pressure on the teeth and bones, moving them. Non-removable braces are fixed on the outside or inside of the teeth; they can solve many problems, but they require constant care and a visit to the clinic once a month. An alternative is aligners, transparent aligners. You can take them off, brush your teeth as usual and eat whatever you want.
In most cases, orthodontic treatment requires from 8 months to 2 years, depending on the complexity of the case. Large-scale changes, such as moving the adjacent seventh tooth to replace the missing sixth, can take 3 years. Plus, there is a possibility of failure, because you need to do a lot of counting.
You can simulate a possible situation based on CT data, tele-radiography and 3D modeling (this is after filming the oral cavity with a scanner). This more or less insures against hidden cysts, supernumerary teeth and other joys that may emerge during the treatment process.
So today:
- What modern orthodontics can do and how much it costs.
- How we correct the bite using braces and aligners.
- Why do we use miniscrews (implants) and palatal expanders in addition?
- When will the result be? And what are we doing to secure it?
- What can go wrong when installing braces or aligners.
About food and beauty
Patients often come to us with something like this: “Listen, give me six teeth here, make them straight.
I’ll get married there, and then I don’t really care.” And we usually refuse if the patient does not understand what he is doing from a medical point of view. Because orthodontics is not just about “teeth visually look straight”, but about normalizing their position when there is “ideal” or almost “ideal” occlusion - that is, the teeth are closed with the greatest number of interdental contacts, tooth meets tooth. That is, on the one hand, it’s aesthetics, on the other, the most important thing is function. Aesthetics at the expense of function can be done faster, but we never do that. Simply put, the human dental system consists of three components: teeth, muscles and joints. When your teeth are uneven, food gets clogged in them, caries occurs, contact points wear out faster and the functionality of chewing food goes down. You can live, but it will be difficult to enjoy a steak.
In orthodontics there is such a thing as Andrews' six keys of occlusion. In general terms, these are the positions of a single tooth and its relationship to both the adjacent tooth and the antagonist tooth, that is, the same “ideal” bite. During the treatment process, we strive to get them all. So, if the surface of the teeth is absolutely flat and there are no bumps on it, due to pathological abrasion, for example, then chewing food becomes very difficult. The teeth begin to work like millstones. And to eat something stronger than cream soup, you have to try. Because this requires point contacts, that is, the meat should be torn as if by the back teeth.
The area of all point contacts in the central occlusion is about 4 square millimeters. The peak strength of the chewing muscles of an adult, according to Weber, is 390-400 kg. So primates are dangerous, even if they are pampered modern Homo with their small teeth and weakened muscles - in comparison with the same chimpanzees who do not mind snacking on a fresh small antelope. If the area of these contacts increases due to abrasion, the meat is ground. Food intake begins to lengthen, and, accordingly, the chewing muscles begin to get tired. You generally begin to think that it is better to limit yourself to dessert.
Occlusion keys from Dr. Lawrence Andrews' book Straight Wire. The concept and appiance. 1 key - the relationship of the molars. 2 - angle of inclination of the crowns - each tooth has/does not have its own angle of inclination. 3 - torque - inclination of the crowns: the angle is formed between the perpendicular to the occlusal plane and the tangent in the middle of the vestibular surface of the clinical crown of the tooth, individual for each tooth. 4 - rotation - teeth in the dentition should not have rotation around their axis. 5 - tight contact - no gaps between teeth. 6 - occlusal plane. Should be aligned, there should not be a distance of more than 1.5 mm between the most prominent cusp of the mandibular second molar and the incisal edge of the lower central incisor
But that's not all. In addition, a bunch of problems begin:
- Habitual dislocation: it becomes unpleasant to open the mouth wide. In very terminal stages, any opening and closing of the mouth is painful, but this process does not occur abruptly, almost imperceptibly for the patient.
- Food gets caught in the cracks or joints of teeth, making them more difficult to clean and requiring treatment more quickly.
- If some teeth are missing and part of the jaw is nonfunctional, muscle load changes and a headache may begin. But these cases are closer to orthopedics.
Well, all sorts of beauty stories: the oval of the face changes, hollowing or sagging of the cheeks may appear, asymmetry, visual aging occurs earlier, etc. In general, teeth are again about comfort. Even without them it is difficult to die. If any of this resonates with you, welcome to the wonderful world of orthodontics. Do not worry, it will not hurt.
Modern diagnostic methods in the transversal direction
Diagnostics in orthodontics is of great importance, since the diagnosis is usually a combination of several anomalies. One important diagnostic criterion is Element III of the Andrews philosophy. Element III WALA ridge (Will Andrews and Larry Andrews) is based on the fact that the width of the mandible is determined by the marginal ridge. Today, cone beam computed tomography (CBCT) is one of the most dynamically developing three-dimensional diagnostic tools in orthodontics. In this regard, in our opinion, the use of CBCT for diagnosing transversal measurements of the skeletal structures of the jaws is very promising.
Inadequate diagnosis of multifactorial dentoalveolar anomalies often leads to the choice of incorrect treatment tactics, resulting in unstable occlusion. Diagnostics in orthodontics is of great importance, since an orthodontic diagnosis is usually a combination of several anomalies. A small, at first glance, deviation from the norm entails further changes in the closure of the teeth. Thus, any anomaly of occlusion is a symptom complex of several anomalies of the teeth, dentition and jaws, considered in three mutually perpendicular planes.
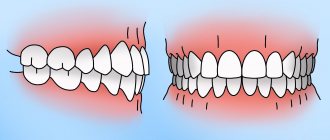
The goal of orthodontic treatment is static and functional occlusion. One of the main conditions for achieving the six keys of normal occlusion according to Andrews is the proportionality of the jaw bones to each other. Orthodontists use a huge number of cephalometric analyzes to diagnose skeletal and dento-alveolar disorders in the sagittal plane and pay insufficient attention to the analysis of direct teleroentgenograms (DRG), which gives the concept of transversal disorders. When there is a mismatch in the size of the jaw bones in the sagittal plane, the dentition tries to “compensate” by creating occlusal contacts, as a result of which we observe protrusion or retrusion of the incisors. In the transversal plane, due to changes in the width of the nasomaxillary complex, teeth erupt crosswise or change inclination to “avoid” cross-occlusion. This compensation is typically manifested by lingual inclination of the lower molars and premolars, and vestibular inclination of the upper (Fig. 1).
What can orthodontics do and how much does it cost?
At the moment, there are only three ways to straighten teeth in orthodontics:
- Vestibular braces. These are permanent pieces of ceramic or metal, fastened with wire and glued to the teeth.
- Lingual braces. Attached to the back of the teeth. They are for those who want to be invisible.
- Aligners. These are plastic mouth guards that are removed before eating. They are only suitable for 80% of patients.
The cheapest thing in orthodontics is metal braces.
Treatment with them costs from 240 to 480-500 thousand rubles in Moscow according to our price list (we take components above the average segment, the cost takes into account work throughout the year). The cost of treatment with aligners is approximately the same. The light version will cost approximately 240 thousand rubles. And the most expensive thing is the internal braces, which are glued on the tongue side. The price is around 500 thousand rubles. The final cost will depend on the duration of treatment and the number of visits; the fewer, the cheaper. If we predict treatment for 2 years, then it will be slightly more expensive. Before placing the aligners, we do a wedge check, where we see the final result: how the teeth will stand in the end and how many trays we will need.
Yes, of course, there are clinics where a patient comes and is told: “Yes, our braces cost 20-30 thousand rubles.” He happily rubs his hands, signs the contract, and then the installation begins... The patient paid for the braces, and then he pays for the installation, for observation, for gluing, for the shift, there are a lot of additional payments.
And any person without a medical education can come to an orthodontic store, say “hello” and buy braces. He can even install them himself. On the Internet I once came across such craftsmen, their argument goes something like this: “Why pay an orthodontist, look, I bought it there myself, glued it on myself, something seems to have leveled out.”
In orthodontics, the patient pays not for braces, but for the doctor’s work. And here’s who already works. Some people don’t bother: they put on braces, the teeth are more or less aligned, but if the tooth doesn’t fit on the tooth, the function suffers, the joint clicks - that’s okay.
There is also support and a guarantee. We have a 5 year guarantee on all services. And if something goes wrong, we will replace everything without any questions asked. Let me remind you that according to Russian legislation, the guarantee for dental services is only 1 year.
What to choose
Usually we use braces if we need to do something global.
For example, large-scale movement of tooth roots, especially molars, is required. I had a case in my practice when we removed the lower sixth teeth and moved the seventh and eighth teeth in their place. That is, we completely pushed the sevens and eights forward by 10-11 mm. There are cases when the lower teeth, for some reason, have moved upward very strongly and it is necessary to carry out dental intrusion. Aligners will not allow you to open your bite well or integrate your lower teeth well. To introduce the anterior teeth and lower them, we use segmental mechanics. We can’t just go ahead and put one single delay, it won’t get implemented. That is, we make special arches that deal purely with the insertion of the front teeth.
Aligners. We even out the bite on these
In general, there is no big difference between braces and aligners. The only difference is that the aligners are removable, you should always remember about them. But braces don't. Plus the biomechanics are slightly different - but you won’t feel it.
Patients with aligners often complain that when we push their teeth back, small spaces form between the teeth. And food can get in between these gaps. Previously, the teeth were all tightly together, that is, there were no gaps, but here small gaps may appear between the back teeth
If there are no contraindications, we allow the patient to make his own decision. Some just come and say: “No, aligners don’t suit me, I’ll forget about them,” or vice versa: “No, I’ve already worn braces, I’ll never wear braces a second time in my life.” Please.
According to my observations, patients like treatment with aligners the most because, firstly, there are no problems with eating. I wanted nuts - I took off my mouthguard and chewed on the nuts, I wanted kebab straight from the skewer - please. The main thing is to rinse your mouth after eating so that nothing gets clogged under the aligners, and put the mouth guard back on.
There are limitations with braces. Almost everything you want to eat needs to be chopped. Too hard food is not allowed.
Plus you need to get used to careful care. There is a risk that with improper hygiene, dental plaque will increase.
There are a lot of auxiliary equipment on the market now - special brushes, brushes, irrigators. With their help, you can clean everything perfectly, but this procedure takes a little more time. And often they clean the top above the bracket, but under the wire they are lazy with brushes, and plaque accumulates there. In general, it all depends on hygiene. If the patient cleans everything thoroughly here, then there should be no problems with either plaque or caries. By themselves, neither braces nor aligners damage teeth or cause caries.
By the way, internal braces, in addition to the fact that they are not visible at all, have a great advantage - even if you brush your teeth poorly, then stains after removing braces, caries, all this will be on the inside of the teeth, and not on the outside.
Auxiliary things
Often, before installing braces or aligners, I perform additional procedures. They help us speed up the process by four months. In addition, I most often take one of the following:
- Palatal clasps. Necessary for the correct inclination of the back teeth. They provide enough space for teeth to be aligned and help correct overbites where the upper teeth sit inside the lower teeth.
- Distalslider and mesiaslider. Helps move teeth back and forth.
- Palatal expander. Needed to expand the upper jaw with a pronounced narrowing to the sides from the center of the palate.
- Miniscrews. They are usually installed in place of missing teeth and serve as a support for the elements of the braces system.
Distance slider
Mesiaslider
It just sounds scary, but in fact, patients tolerate it very easily. Probably the biggest discomfort in this whole procedure is that a gap appears between the front teeth. That's all. The process itself is not painful, plus by skeletal expansion of the upper jaw, we not only create space in the anterior region to align the front teeth, we also expand the nasal passages. If a person has problems, for example, with nasal breathing, then by skeletal expansion of the upper jaw we can improve nasal breathing and reduce the risk of sleep apnea. To some extent, we extend the life of patients.
Approximate logic when choosing torque
| LOW TORQUE Recommended for the treatment of non-extraction cases with crowding and/or narrowed dentition (regardless of class), as well as protrusion or protrusion of teeth | HIGH TORQUE Recommended in cases of tremors, extraction or distalization of anterior teeth, as well as in cases of retrusion or tendency to retrusion of teeth |
STANDARD TORQUE Dr. Dwight Damon suggests using standard torque in cases where braces need to be positioned as close to the gum as possible to improve incisor exposure (smile arches), in cases with low occlusal plane angles and severe open bites. Standard torque is also suggested for mandibular anterior teeth in cases with periodontal ligament restriction or damage.
How will the position of the maxillary central incisor change when choosing different torque options?
The graph shows the arc “play” zones in the bracket slot for each torque option in accordance with its color. For Damon braces, this zone is equal to the nominal value of ± 10.5° (rounded to 11 on the graph for convenience).
In other words, in the absence of additional forces, a bracket with a selected torque will not move a tooth located in its “playing” zone of the arch (zone on the graph).
Example 1: if the tooth is in the position of the torque value from +11 to +13, then no bracket will move it, because for any torque option, the arc in this range will be in a passive position and will not interact with the groove. Example 2: High and standard torque brackets will not move a tooth with a torque of +11° to +26° in the absence of additional forces. Example 3: the tooth stands with a high torque and an additional force (spring, chain) acts on it, moving it back. If in this situation a high-torque bracket is glued to the tooth, then the most extreme point at which it will stop is +11°, which is normal. If in this situation you stick a bracket with a standard torque, the tooth will go into retrusion up to +4°.
The most modern Damon prescription system available in Russia is the Damon Q braces system. On the official Ormco website you can read more information about Damon Q braces.
Also, using a convenient bracket picker, you can assemble a set and buy Damon Q online.
When will the effect take place?
From the first stages, when you put on braces or aligners, people usually immediately feel the changes.
Some patients who wear braces notice that their teeth begin to move during the process. At first, the teeth aligned with each other, and then the dentition aligned or the tooth grew crooked, and then its position returned to normal. Patients really like this. Some then ask for before/after photos and make stories. For some, the very fact that teeth move gives a pleasant sensation. They like that they are constantly wearing something, constantly brushing their teeth. That is, some part of life is devoted specifically to the oral cavity. And others sometimes get bored after a year or a year and a half. This is most often due to the fact that you don’t have an extra snack, that food gets stuck, and it’s difficult to brush your teeth. With aligners, it’s somehow easier to deal with all this.
Main types of tooth movement
1. Corpus: the root and crown of the tooth move the same distance in the same direction a. mesial-distal movement = parallel movement (or right-left when looking at the tooth from the lips/cheeks) b. vestibulo-oral movement = narrowing/widening of the dentition (or back and forth if looking at the tooth from the lips/cheeks) c. dentoalveolar elongation/intrusion = extrusion/intrusion (or up-down)
2. Rotational: rotation around its axis
3. Oblique-rotational: the root and crown of the tooth move different distances in different directions a. mesial-distal tilt (angulation or right-left tilt) b. vestibulo-oral tilt (inclination = torque or forward-back tilting)
How much to wear
Usually, at the diagnostic stage, we can already estimate how long the treatment will last. Normally - from 8 months to 2 years. It all depends on the severity. If the case is very simple, we can cure it in 8-12 months. Sometimes for four or five. This usually works when the patient has already worn braces, but he has had some kind of relapse, and we just need to correct the teeth a little, or if the deformation occurred due to the loss of teeth, so-called secondary deformations. Often, up to two years of treatment may be required. It happens that treatment takes 2.5-3 years. These are really complicated cases. Much like I described above with the movement of teeth. When treatment lasts more than 3-4 years, it means there is a mistake somewhere in terms of diagnosis - something was not taken into account, something was not calculated, and pitfalls began to emerge. To prevent this from happening, detailed diagnostics are needed.
Where is the torque lost?
An arc that has the same size as the groove is called full-slot. Arches used for orthodontic treatment using the passive self-ligation technique are always smaller than the slot size, i.e. not full-slotted. Full-slot arches are not used in practice for two reasons. The first is the large forces produced by a full-slot arch. The second is the high resistance to sliding of the arc in the groove as a result of the coincidence of the dimensions of the groove and the arc. Accordingly, the arc always has some freedom of movement and can “play” in the groove. This “play” of the arc in the groove is called geometric loss of torque.
In the Damon system, the play of an arc with a section size of .019 × .025 in a groove with a size of .022 × .028 is 10.5 ° in one direction (according to the manufacturer). The arc cross-section size .019×.025 is the maximum for the passive self-ligation technique and the smaller the arc cross-section size, the greater will be the play of the arc in the groove and, accordingly, the greater the loss of torque.
There is also force loss of torque, where the arc may not have enough force to create a torque even after overcoming the geometric loss. However, there are currently no clear data on the magnitude of power loss.
Thus, it must be understood that when working with the passive self-ligation technique, the torque embedded in the bracket groove will not be fully realized automatically.
Example. The figure shows that when a tooth is in an abnormal position, for example, with a high torque (1) and a bracket with a standard torque is glued to it, the rectangular arch presses on the walls of the bracket groove, as a result of which the tooth begins to align towards the normal torque and stops 10.5° before its correct position (2). If an additional force is applied to the tooth (for example, an elastic chain), the tooth will move until the arch begins to press with its edges on the walls of the bracket groove, and this position will differ from the normal position of the tooth by 10.5° from its correct position (but in the direction of low torque) (3).
Why do we spend so much time on diagnostics?
In general, from the profile, from the full face, without even looking into the oral cavity, we can characterize the patient’s skeletal frame, that is, the initial position of the jaws based on the proportions of the face, and roughly estimate what we will see in the mouth.
This is the most important part of orthodontic treatment. Our diagnostics consists of several stages:
- Photo.
- CT.
- Teleradiogram.
- 3D modeling.
I usually start with photography.
I look at the frontal view, the profile of the patient and generally assess the asymmetry, whether there is a displacement of the lower jaw. Next, I ask the patient to open his mouth slightly, looking at the exposure of the incisors. When the lips are completely relaxed, ideally the upper incisors should be visible somewhere 2-4 mm from under the lip. If a person’s incisors are too visible, for example, the upper incisor is completely visible at rest, and the upper incisors completely overlap the lower ones, this is the so-called deep bite. Then, naturally, we look at and implement the implantation of the upper incisors in order, firstly, to reduce their exposure, and secondly, such patients most often have a gummy type of smile, that is, so that when smiling, less gums are visible.
Next, we evaluate the smile itself, look at the position of the incisors - how much the incisal edge follows the contour of the lower lip, and how we can make adjustments accordingly so that the smile is, let’s say, more aesthetic.
Plus, we evaluate the lips - we measure the length of the upper and lower lips. Because the patient may have a large exposure - when the upper incisors are clearly visible, for example, half, by 5-6 mm. This may be due to anatomical features when a person has a short upper lip, and not due to the fact that his incisors are incorrectly positioned.
Then we turn the patient at an angle of about 45 degrees, this is necessary to assess the tone of the lips. From this angle, the tension in the lips is very clearly visible. If, for example, a person’s teeth have moved forward very far, it is difficult for him to close his lips, there is tension. Usually such patients walk with their mouth slightly open.
Naturally, we need to reduce this tension and consider treatment tactics to move the teeth back as much as possible, so that it is easier and easier for the lips to close. Then we evaluate the nasolabial folds. For example, if there is underdevelopment of the upper jaw, when there is an incorrect bite and the lower jaw is in front of the upper jaw. That is, if they have a problem specifically with the upper jaw, they very often have these very pronounced nasolabial lips due to the posterior position of the upper jaw itself. If the jaw is deep, then the nasolabialis is strongly pronounced. Or, on the contrary, hypotonia is when the lip is not convex, but hangs like a curtain.
At the next stage, we definitely do a CT scan. We evaluate the bone tissue and see if there are any cysts that are not visible on the panorama. Once in one clinic I saw a case where a boy of about 14 had an orthopantomogram before treatment, everything was clear there. A year later he came, he had some kind of lump on the roof of his mouth, he said: “Well, a lump just appeared.” We started looking, did a control ortho, there was a large cyst on several teeth. Before that, the teeth were absolutely healthy, there was no trauma, it was just, apparently, a congenital cyst, which increased during orthodontic treatment. They pulled up old photographs, but she was not visible in them.
CT scan helps us find hidden cysts
If a CT scan reveals not only a cyst, but any pathology of any of the teeth, then it must be eliminated before orthodontic treatment begins. The exception is large and multiple dental restorations, which are best performed in the final bite.
Otherwise, it can grow, and if it takes over several teeth, we can simply lose these teeth by depulping them. Plus, on a CT scan we evaluate the width of the jaws: how wide the upper jaw does not match the lower jaw. This provides parameters for maxillary expansion. Sometimes there are hidden pathologies of crossbite, when it seems that there is nothing complicated, you put on braces, but you get a crossbite when the lower teeth begin to overlap the upper teeth in the lateral sections, although this was not the case before the start of treatment.
On a CT scan, you can evaluate the position of the articular heads - whether there is a posterior position, that is, whether the lower jaw is displaced back or not. Treatment tactics will greatly depend on this. Because if we have pictures of the posterior position of the articular heads and the patient’s upper front teeth are tightly pressed to the lower ones and deeply overlap them, this very often happens, and he may not even present to the clinic dysfunction of the temporomandibular joint, then we are still in In our treatment tactics, we will push the jaw forward a little. In order to avoid problems with the joint in the future, so that the patient’s problem is immediately solved and there is no need for retreatment.
The next thing we do is a TRG - a teleradiogram. It allows you to assess whether there is any pathology that caused it. For example, incorrect position of the lower jaw, incorrect formation, relative position of the jaws. Allows you to determine the inclination of the teeth, type of growth, and so on.
And most importantly, thanks to modern technologies, we can combine the virtual models of the patient that we scanned with the patient’s CT scan, with TRG. After we have figured out the treatment plan, made a virtual setup, that is, moved the teeth to a new position, we can evaluate how much our parameters will change, how harmonious everything will look immediately after treatment.
We also make a 3D model. And we combine it with the received data. Plus, I try to make videos for patients so that they can see where the teeth will move, due to what, and so that they understand how the treatment will proceed.
CT scan of the temporomandibular joint
The diagnosis itself takes about an hour for the patient - to take all the data, for the doctor - two to three hours. Therefore, our diagnostics cost 24,500 rubles, and not 5, as in the clinic around the corner.
Such diagnostics are not needed to answer the question of whether orthodontic treatment is indicated or not. Any orthodontist can tell this simply based on the results of the examination. Such diagnostics are needed to answer the question of how to implement this orthodontic treatment, in what way. And give the patient an idea of what it will be like, how long it will last, what equipment the doctor will use, and how the patient’s condition will change during and after treatment.
Inadequate diagnosis of multifactorial dentoalveolar anomalies often leads to the choice of incorrect treatment tactics, resulting in unstable occlusion. Diagnostics in orthodontics is of great importance, since an orthodontic diagnosis is usually a combination of several anomalies. A small, at first glance, deviation from the norm entails further changes in the closure of the teeth. Thus, any anomaly of occlusion is a symptom complex of several anomalies of the teeth, dentition and jaws, considered in three mutually perpendicular planes.
The goal of orthodontic treatment is static and functional occlusion. One of the main conditions for achieving the six keys of normal occlusion according to Andrews is the proportionality of the jaw bones to each other. Orthodontists use a huge number of cephalometric analyzes to diagnose skeletal and dento-alveolar disorders in the sagittal plane and pay insufficient attention to the analysis of direct teleroentgenograms (DRG), which gives the concept of transversal disorders. When there is a mismatch in the size of the jaw bones in the sagittal plane, the dentition tries to “compensate” by creating occlusal contacts, as a result of which we observe protrusion or retrusion of the incisors. In the transversal plane, due to changes in the width of the nasomaxillary complex, teeth erupt crosswise or change inclination to “avoid” cross-occlusion. This compensation is typically manifested by lingual inclination of the lower molars and premolars, and vestibular inclination of the upper (Fig. 1).
Rice. 1. Negative inclination of molars indicating the angle of their lingual inclination.
The relationship between transversal disorders and functional occlusion
The compensatory changes in teeth in the transversal plane described above are graphically depicted in the literature in the form of a Wilson curve. Thus, excessive inclination of the molars of the upper jaw to compensate for the deficit in the width of the upper jaw is manifested by a pronounced Wilson curve, i.e., the palatal cusps are located below the buccal cusps (Fig. 2).
Rice. 2. In-depth Wilson curve. The buccal cusps are located above the palatal cusps, the “sagging cusps.”
Many articles describe the negative impact of the discrepancy between the CO (central occlusion) and the CR (central jaw relation) on the sagittal and vertical parameters of the dentofacial system. It is described in the literature that “sagging” palatal tuberosities form premature contacts when the teeth are closed, thereby provoking a vertical displacement of the articular process. In the case of premature contacts on the last molars, the patient is forced to move the lower jaw to ensure occlusion. A common symptom in patients with anomalies of occlusion (narrowing of the upper jaw) is the location of the palatal cusps of the lateral teeth of the upper jaw below the occlusal plane, as well as dentoalveolar compensation, expressed by the inclination of the upper lateral teeth vestibularly. Thus, in the absence of cross-occlusion, sagging buccal cusps and a pronounced Wilson curve become the starting point for vertical displacement of the articular process to achieve maximum fissure-tubercle contacts. Moreover, normalization of skeletal abnormalities along the transversal, flattening of the Wilson curve, coordination of the dental arches are an important component for eliminating the discrepancy between the CO and the CO.
The relationship between transversal disorders and periodontal condition
A large number of studies prove that there is a high risk of gingival recession in orthodontic patients if dentoalveolar compensation is attempted for the narrowing of the maxilla. According to the literature, the limit of changes in the size of the dentition in the transversal direction is much less than in the sagittal direction, since due to compression of the thin layer of cortical bone of the alveoli on the vestibular side, minor movements of the teeth can lead to fenestration, loss of bone tissue, and thinning of the gingival tissues. Elimination of premature contacts on the working and balancing sides has also been shown to improve the patient's periodontal status (Fig. 3).
Rice. 3. Recession after orthodontic treatment due to transversal discrepancy in the size of the jaws (lack of cortical bone on the vestibular side of the upper molar) (a) and discrepancy in the size of the dentition in the transversal direction (b).
Diagnostic methods in the transversal plane
In case of changes in the size of the upper jaw along the transverse, the temporomandibular joint (TMJ), periodontal tissue and airways are most susceptible to negative influence. To identify disorders, diagnosis is necessary in all three (sagittal, vertical, transversal) planes. This paper describes some methods for diagnosing transversal anomalies of the dentofacial system, which, in our opinion, need to be included in the examination protocol for orthodontic patients. Regardless of the diagnostic method preferred by the doctor, he should focus on the following criteria for a normal ratio in the transversal plane:
- teeth are located in the center of the alveolar process;
- teeth are aligned in the alveolar process;
— the teeth are in correct contact with the antagonist (Fig. 4).
Rice. 4. The location of the molars in the middle of the alveolar process.
This is important for:
— stability;
- functions;
- TMJ health;
- periodontal disease.
Transversal diagnostics as an integral part of achieving functional occlusion
Traditionally, in orthodontic diagnostics, more attention is paid to measurements in the sagittal and vertical planes. However, the correct definition of transversal parameters is no less, if not more important and informative. Research proves that occlusal interference due to an inadequate Wilson curve plays a decisive role in discrepancies between the CO and the CO, thereby having the most negative impact on periodontal health and craniofacial development.
Analysis by Andrews
In 1970, Andrews described 6 keys of normal static occlusion. Subsequently, Andrews et al. developed a 6-element philosophy for optimal diagnosis. One important diagnostic criterion is Element III of the Andrews philosophy. Element III WALA ridge (Will Andrews and Larry Andrews) is based on the fact that the width of the mandible is determined by the marginal ridge. According to Andrews' definition, the marginal ridge is determined by the most protruding part of the alveolar process on the vestibular side. The WALA ridge coincides with the mucogingival junction at the center of resistance of the mandibular molars. In non-growing patients, the width of the lower jaw and alveolar process, and accordingly the WALA ridge, do not change during orthodontic treatment. Thus, WALA ridge is a stable basis of Element III of the Andrews philosophy (Fig. 5).
Rice. 5. Borders of WALA ridge: front view (a) and view from the occlusal surface (b).
Element III assumes that the upper and lower molars should be located in the center of the alveolar bone, have correct inclination and adequately occlude with the antagonists, i.e., the supporting cusps of the upper molars are located in the fissure of the antagonist teeth. To determine the discrepancy between the upper and lower jaw along the transversal, a certain algorithm is used.
Step 1
The width of the lower jaw or the horizontal distance from WALA ridge on the right to WALA ridge on the left is determined.
According to Andrews' research, optimally positioned mandibular molars should be aligned in the alveolar ridge such that the FA-facial axis point, or crown center, is 2 mm behind the WALA ridge. Based on the above, the width of the lower dentition is determined by the formula:
(WALA ridge on the right – WALA ridge on the left) – 4 mm.
Step 2
The width of the upper dentition depends on the optimal inclination of the upper molars. To determine this width, it is necessary to measure the distance from the FA point on the right molar to the FA point on the left molar. Then evaluate the existing inclination of the upper molars and determine the distance that will appear between the FA points on the right and left when the molars are optimally aligned, using the formula: 1 mm = 5° change in inclination.
The difference obtained in millimeters is subtracted from the original parameter FA on the right and FA on the left. The final result represents the existing width of the maxilla. In order for the molars of the upper and lower jaw to have an optimal transverse relationship with each other, the width of the upper jaw should be 5 mm greater than the width of the lower jaw.
All of the above is clearly demonstrated in the following clinical example:
Lower jaw:
WALA ridge left – WALA ridge right = 50 mm (Fig. 6).
Rice. 6. Width in the WALA ridge area.
FA right – FA left = 44 mm (Fig. 7).
Rice. 7. Width in the FA-FA area.
Accordingly, according to the formula (50 - 4 mm), the FA-FA distance should be 46 mm, i.e. 2 mm more than the existing one (46 - 44).
Conclusion: it is necessary to align the lower molars by 1 mm on each side (change the inclination by adding 5° of vestibular coronal torque to the lower molars).
Upper jaw:
The optimal width of the upper jaw is 46 + 5 = 51 mm.
Initial distance FA left – FA right = 45 mm.
According to direct TRG, the inclination of 16, 26 is increased by 5° on each side, i.e., when the axial position of the upper molars is normalized, the FA point on the right and left will shift orally by 1 mm. Therefore, true FA right – FA left = 45 – 2 = 43 mm. Thus, we need to expand the upper jaw by 8 mm.
CBCT Analysis
Today, CBCT is one of the most dynamically developing three-dimensional diagnostic tools in orthodontics. With the help of CBCT, orthodontists are able to accurately measure any parameters without any distortion. In this regard, in our opinion, the use of CBCT for diagnosing transversal measurements of the skeletal structures of the jaws is very promising. The Ricketts and Andrews methods for quantifying skeletal discrepancies are based on the use of specific anatomical landmarks—the width of the maxilla and mandible. So in Ricketts' analysis these are the points Mx-Mx for the upper jaw and Ag-Ag for the lower jaw.
The Andrews analysis uses the WALA ridge and FA as anatomical landmarks. The WALA ridge measurement on the left and right represents the width of the lower jaw, and the FA measurement on the right and left (using the method described above) determines the width of the upper jaw. Although both of these methods are invaluable for orthodontic diagnosis, the use of CBCT significantly differentiates the identification of anatomical landmarks, thereby minimizing the possibility of error.
As identifying measuring points for the upper jaw, the most optimal point will be point M from the Ricketts analysis, and for the lower jaw, the point from the WALA ridge analysis is taken, since these points correspond to the absolute minimum width of each jaw.
Computer analysis algorithm
1. Open the multiplanar view to simultaneously display sagittal, coronal and axial slices (Fig. 8).
Rice. 8. Multiplanar view.
2. To determine the width of the lower jaw, scroll down the image to determine the furcation of the first molars. Then we scroll the image until the center of the lower molars is identified on the coronal scan (Fig. 9).
Rice. 9. Determination of the width of the lower jaw.
3. Turn on the full-screen axial view and, using the measurement lines as guides, measure the lower jaw until the intersection of the reference lines from the most protruding point of the cortical plate on the right and left (Fig. 10).
Rice. 10. Measuring the width of the lower jaw.
4. For the upper jaw, a similar method is used with the only difference being that the measurements of the Mx point are determined on the axial and coronal reformates, as in the Ricketts analysis (Fig. 11).
Rice. 11. Measuring the width of the upper jaw.
5. Analysis of the width of the upper and lower jaws is carried out at the level of the first molars. By subtracting the width of the upper jaw from the width of the lower jaw, we determine the difference between the two jaws. Both the Ricketts and Andrews analyzes demonstrate that the optimal jaw difference is 5 mm in adult patients. Preliminary analysis with molars aligned in the alveolar process, located at its center, with good intercuspidation, showed a constant difference in jaw width of 5 mm. Previous Penn CBCT analysis showed the same ideal result of 5 mm. To determine the degree of expansion of the jaws for their ideal relationship, it is necessary to subtract 5 mm from the jaw difference. Thus, one of the main conditions for achieving stable and functional occlusion is the correct inclination of the molars, their location in the middle of the alveolar process and the correspondence of the width of the dentition to each other, which will allow to achieve good fissure-tubercle contact of the antagonist teeth and avoid the negative impact of orthodontic treatment on the TMJ and periodontal tissue.
When should I come again?
Typically, a patient wearing aligners comes in for an appointment once every 2-2.5 months.
If nothing needs to be sanded and no additional step is required. We immediately issue all mouth guards for the period until the next appointment. With braces, I prefer to see a patient on average once every 5-6 weeks. In the first stages, we can sometimes let you go for 2 months. In the end, when the bite and position of the teeth are normalized and we are preparing for removal, we look once every 3 weeks. We are already making compensatory bends and adjustments there - we arrange the teeth in more detail so that everything fits together beautifully, so that the teeth stand correctly, in general, we bring it to the ideal. Most often, patients do not particularly notice this.
How will it all end?
Orthodontic treatment always ends with retention devices - these things hold the teeth in their new position.
When we treat with aligners, we most often make retention aligners; they are very similar to those the patient already wears. Therefore, he does not experience any discomfort. If, for example, the patient is tired of wearing mouth guards or we remove braces, then we can glue thin wires - retainers - to the side of the tongue. Most often, patients completely forget about their existence. There is a category, very, very, very rarely, when they interfere with someone, these are just isolated cases. Overall, patients are very satisfied with orthodontics.
PS If you come to our clinics, then say that you are from Habr, there will be a 5% discount.