Herpetic, or herpetic, stomatitis in children is very common. This is an infectious disease that affects the oral mucosa. It is caused by the herpes simplex virus, transmitted by airborne droplets or through contact with its carrier. Primary infection is almost always associated with a decrease in the functions of the immune system.
The manifestation of individual symptoms of herpes stomatitis in children depends on the form and stage of the disease. The forms of the disease include mild, moderate and severe, which is quite rare in childhood.
At the initial (incubation) stage, there are no obvious symptoms of the disease.
During the prodromal period of herpes stomatitis in children, the following appear:
- loss of appetite;
- sleep disorders;
- nausea and vomiting;
- enlarged lymph nodes.
When the disease reaches its peak, the following signs become noticeable:
- the appearance of blisters and ulcers on the oral mucosa;
- swelling and bleeding of the gums;
- heat;
- cough and runny nose (not always);
- general malaise.
During the period of decline of herpes stomatitis in children, the temperature drops, the general condition improves, but rashes in the mouth persist for some time.
Herpetic stomatitis: symptoms
Taking into account the nature of the disease and the characteristics of its course in the patient, two forms are distinguished: acute and chronic recurrent. In the first form, the symptoms are very pronounced, the disease is more severe, and all signs usually disappear completely after adequate treatment. In the chronic relapsing form, the symptoms are less pronounced, long periods of remission (“rest”) are observed with periodic relapses.
Acute herpetic stomatitis most often occurs in young children and adolescents. In adults, this disease occurs much less frequently, since their immune system works better and more actively than children's. This disease is also called herpetic aphthous stomatitis, due to specific aphthous ulcers in the patient’s mouth. The main signs of stomatitis in children and adults are:
- Swelling and redness of the mucous membranes of the mouth.
- Single or grouped vesicles with serous contents in small areas of the mucous membrane. When such bubbles collapse, erosive spots with a whitish coating in the center are formed. Such erosions are very similar to true aphthae, so the disease was previously classified as herpetic aphthous stomatitis, although in fact we are talking about two different types of the same disease.
- Pain when eating and drinking, burning and itching in the mouth.
- Weakness, fever, nausea, possibly vomiting and diarrhea. These symptoms almost do not appear with mild degrees of the disease; with moderate and severe degrees they are quite pronounced.
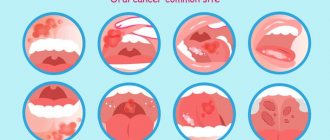
What the oral cavity looks like with herpetic stomatitis can be seen in the photo.
Stomatitis in a child - what to do?
In pediatric patients, stomatitis is the most common diagnosis, which occurs even in children during the neonatal period. The concept of stomatitis itself combines several diseases that are expressed by ulceration and/or inflammation of the mucous membrane in the oral cavity.
Causes of stomatitis in children
Stomatitis can develop for a number of reasons, but the most common are allergic and infectious. Inflammation of the oral mucosa in children can be caused by:
- Herpes, chickenpox, influenza and rubella viruses. The main symptom of the viral form of stomatitis is rapidly bursting blisters that transform into extremely painful oval ulcers covered with a yellowish coating.
- Bacteria (staphylococci, streptococci and others). Symptoms of bacterial stomatitis consist of the appearance of a putrid odor from the oral cavity, redness of the mucous membranes and the formation of superficial erosions on it.
- Fungi (candida, mycoplasma and others). The main symptom of candidal stomatitis is the formation of a dense cheesy coating on the inner surface of the cheeks, tongue and gums. The child's breath smells like sour milk.
- Mechanical damage, allergies in combination with infection of the mucous membrane (aphthous stomatitis). The symptomatic picture includes the formation of round, well-defined ulcers, covered with a dense white coating and surrounded by a pronounced rim (granulation).
The onset of the disease can be triggered by a lack of vitamins, a stressful situation, general hypothermia (even mild), immunodeficiency and an allergic reaction, anemia and dehydration of the body. However, most often stomatitis is diagnosed after a course of treatment with antibiotics and sulfonamides.
Symptoms of the disease in children
The first signs of stomatitis in children resemble a common cold and ARVI. They appear 4-8 days after infection. The most common symptoms are:
- temperature rise to 38-40 degrees;
- general malaise, tearfulness;
- increased gag reflex and nausea;
- enlarged lymph nodes in the neck.
Less commonly, children may be bothered by cough and runny nose, conjunctivitis. A day after the appearance of these symptoms, a gray, white or yellowish coating forms in the child’s mouth (depending on the type of pathogen), and later - ulcers or watery blisters.
Already at this stage, the child needs complex therapy, which can be started after detailed diagnosis. First, a culture is carried out to determine the causative agent of the disease, and its sensitivity to drugs is also determined. In addition, consultation with a pediatric gastroenterologist, allergist and endocrinologist may be required. Only after this can the doctor prescribe appropriate treatment.
Treatment methods for stomatitis in children
The tactics of therapeutic measures to combat stomatitis in children are determined by the diagnostic results and consist of a set of standard procedures, the action of which is aimed at reducing symptoms, and taking medications appropriate to the type of pathogen.
For viral and herpetic stomatitis, children are prescribed the following medications:
- antiseptic drugs - Stomatidin and Hexoral;
- anti-inflammatory and painkillers - Paracetamol, Nurofen, Ibuprofen;
- antiviral and antiherpetic drugs - Bonafton, Acyclovir, Viferon and Zovirax;
- healing preparations for treating ulcers - Vinilin, Karotolin.
Additionally, folk remedies can be used: sea buckthorn and rosehip oil, centenarian oil and decoctions of chamomile and sage.
For fungal stomatitis, drugs with antimycotic and healing effects are used:
- Pimafucin;
- Clotrimazole;
- Fukortsin;
- Candide.
Additionally, the mucous membranes are treated with Nystatin tablet powder. Children are advised to take Diflucan and Fluconazole tablets, Imudon and pain relievers (Nurofen, Paracetamol and Panadol).
For aphthous stomatitis, the set of drugs depends on the source of the disease:
- for the allergic nature of stomatitis - antihistamines in the form of creams, ointments and tablets (Loratadine, Cetrin);
- for an infectious nature - Hexoral and Lugol, as well as Iodinol;
- for stomatitis caused by gastrointestinal problems - Bonafton, Dekaris and others.
Treatment of ulcers in the oral cavity is carried out using boric acid, the drug Aekol, sodium tetraborate and Cholisal gel.
For stomatitis caused by the activity of pathogenic bacteria, treatment of the oral cavity with antimicrobial drugs Chlorhexidine and Miramistin, Furacillin and Metrogyl is recommended. In the case of a prolonged course of the disease or in the absence of a visible effect, antibiotics are prescribed orally. In childhood, the drugs Ampiox, Kanamycin, Gentamicin are indicated. At the same time, they strengthen the child’s own immunity with Interferon or Viferon and vitamin complexes.
Basic rules for treating stomatitis in children
In addition to regularly taking medications and daily treatment of the oral cavity with special solutions prescribed by your doctor, you must follow several general rules:
- Dieting. It is important to exclude spicy and salty dishes, coarse, too hot or cold foods from the child’s menu. You should also give up sweets.
- Oral hygiene. During an exacerbation of stomatitis, when the symptoms are most severe, brushing your teeth with brushes is not recommended. It is better to give preference to rinsing with disinfectant solutions and herbal decoctions.
- Personal hygiene of the child. It is better for the sick person to provide a separate set of dishes, which must be disinfected daily by boiling or special detergents. The same applies to the child's toys and personal belongings.
An equally important point in the treatment of stomatitis in children is strict adherence to the doctor’s recommendations. Despite the abundance of drugs that help get rid of symptoms, their independent selection and use can lead to the transition of the disease to the chronic stage, or even aggravate the course of the disease with numerous complications.
Acute herpetic stomatitis in children and adults: treatment
When herpetic stomatitis is detected in adults and children, it is possible to determine how and how to treat this disease only after differential diagnosis: the herpetic and aphthous types are very similar in symptoms, but the drugs used for therapy are completely different. Therefore, first of all, you need to do tests and make sure that the cause of the disease was the herpes virus.
When treating the disease, antiviral drugs, immunomodulators (to stimulate the immune system), local antiseptic treatments, and vitamin complexes are used to maintain the body's defenses. Additionally, symptomatic medications are used: painkillers, antipyretics for high body temperature in children (above 38.5 degrees).
The doctor prescribes all medications and treatment regimens individually, taking into account the patient’s age, the general condition of his body, the severity of the disease and its form (acute or chronic). In addition, proper dental care is also important - both during and after treatment. The doctor will give all the necessary recommendations for care and help you choose hygiene products individually.
Herpetic stomatitis during pregnancy requires a special approach. In addition to local treatment with antiseptics, it also requires antiviral therapy, but the doctor selects the drugs very carefully, taking into account the possible risks for the pregnant woman and the fetus. Treating yourself in this situation is extremely risky; self-medication can cause serious complications in the body of the mother and her unborn child.
“32 Dent” clinics provide all types of dental services, including gum treatment. Dentists are equipped with the latest equipment, and doctors have extensive experience working with a variety of, even the most complex, clinical cases. By contacting us, you receive high-quality treatment and lasting results at an affordable price.
Sources:
- Personal experience as a dentist;
- Danilevsky N.F., Leontyev V.K., Nesin A.F., Rakhniy Zh.I. Diseases of the oral mucosa. - M.: OJSC "Dentistry", 2001;
- Ivanova E.N. and others. Diseases of the oral mucosa. - Rostov n/d.: Phoenix, 2007;
- Ed. prof. A.L. Mashkilleyson, prof. E.V. Borovsky. Diseases of the mucous membrane of the oral cavity and lips. - M.: MEDpress, 2001;
- Kolesov A.A. Pediatric dentistry. M.: Medicine, 1991;
- Vinogradova T.F., Maksimova O.P., Melnichenko E.M. Periodontal disease and oral mucosa in children. M.: Medicine, 1983;
- Whitley RJ, Roizman B. Herpes Simplex virus Infection // The Lancet. 2001.
Instructions for use of ACICLOVIR
Adults:
Infections caused by Herpes simplex viruses types 1 and 2:
200 mg 5 times a day with an interval of 4 hours (except for the period of night sleep). The course of treatment usually lasts 5 days, but can be increased according to the patient's condition and response to therapy. In patients with immunodeficiency (for example, after bone marrow transplantation) or in patients with impaired absorption from the intestine, the dose may be increased to 400 mg 5 times a day or the possibility of intravenous use of the drug should be considered.
Prevention of recurrent infections caused by Herpes simplex viruses types 1 and 2:
- in patients with a normal immune system:
200 mg 4 times / day with an interval of 6 hours or 400 mg 2 times / day with an interval of 12 hours between doses. The use of the drug should be started as soon as possible after the infection occurs; in case of relapses, it is recommended to begin use in the prodromal period or after the first signs of infection appear. For many patients, the desired effect can be achieved using 200 mg twice a day with an interval of 12 hours. In some patients, relapses can be observed at a dose of 800 mg / day. - in patients with immunodeficiency:
200 mg 4 times / day with an interval of 6 hours. In patients with severe immunodeficiency (for example, after bone marrow transplantation) or in patients with impaired absorption from the intestine, the dose can be increased to 400 mg 5 times / day or it is necessary to consider the possibility of intravenous use of the drug.
Treatment should be interrupted every 6-12 months to study possible changes in the course of the disease.
The duration of prophylactic use is determined by the length of the period of risk of infection.
Infections caused by Varicella zoster:
800 mg 5 times a day with an interval of 4 hours (except for the period of night sleep). Treatment should last for 7 days.
For patients with immunodeficiency
it is necessary to consider the possibility of intravenous use of the drug.
Treatment with acyclovir will be more effective if started as soon as possible after the rash appears.
Treatment of chickenpox
in immunocompromised patients should be started within 24 hours of the onset of the rash.
- Varicella (Chicken pox):
20 mg/kg body weight (not to exceed 800 mg) every 8 hours for five days. Treatment should be started when the first signs and symptoms of the disease appear. - 2-5 years - 400 mg 1 time / day;
- children under 2 years old
- 200 mg 1 time / day.
Adults (if kidney function is impaired):
In the treatment and prevention of infections caused by Herpes simplex viruses,
in patients with severe renal impairment (creatinine clearance <10 ml/min), a dose reduction to 200 mg of acyclovir twice daily with an interval of 12 hours is recommended.
In the treatment of chickenpox
in patients with severe renal impairment (creatinine clearance less than 10 ml/min), it is recommended to adjust the dose to 800 mg of acyclovir 2 times a day with an interval of 12 hours. In patients with moderate renal impairment (creatinine clearance 10-25 ml/min) - 800 mg of acyclovir 3 times a day with an interval of 8 hours.
Children:
Treatment and prevention of infections caused by Herpes simplex viruses types 1 and 2 in immunocompromised children:
Children over 2 years of age
should take the adult dose, and
children under 2 years of age
should take half the dose.
Treatment of chickenpox:
children 6 years and older
- 800 mg 1 time / day;
Treatment should last 5 days.
For the treatment of chickenpox in children with immunodeficiency, it is necessary to consider the possibility of intravenous use of the drug.
There are no data on the prevention of recurrent herpes simplex virus infections or the treatment of herpes zoster virus infections in immunocompetent children.
In elderly patients
clearance of acyclovir decreases. Particular attention should be paid to dose reduction in elderly patients with reduced creatinine clearance. Before using large doses of acyclovir, especially in elderly patients, it is recommended to assess the degree of dehydration and creatinine clearance.
Elderly patients and patients with renal failure
have an increased risk of developing neurological side effects, these reactions are usually reversible after cessation of treatment. Long-term or repeated courses of treatment with acyclovir in immunocompromised individuals may lead to the development of virus strains with reduced sensitivity to acyclovir.