Quite often, wisdom teeth cause problems to a person. They erupt at approximately the age of 20-25 years, when the dentition has already formed and in most cases their appearance is accompanied by complications. The extreme molars do not serve any useful function, so dentists often recommend that patients have them removed.
It should be understood that wisdom tooth extraction is a rather complicated procedure for both the doctor and the patient, especially the removal of molars on the lower jaw.
When you need to remove the bottom "eight". Indications
Wisdom teeth are distinguished by late eruption, which occurs at 20-30 years of age. During this period, the dental system is practically formed and the third molars often do not have enough space in the dentition. Eruption causes various complications and in most cases requires removal of the molar. In addition, in humans, with evolution, a decrease in the size of the jaws occurs, since, due to the nature of nutrition, the chewing load is constantly decreasing.
Most people do not take good hygienic care of their last teeth. They are located at the end of the dentition, and it is often technically impossible to clean them well. This leads to the accumulation of plaque, damage to the enamel by the carious process and its complications (pulpitis, periodontitis). Root canal treatment is very difficult due to difficult access. Therefore, eights must be removed in 90% of cases.
Removal of a fully erupted wisdom tooth
Removal of the lower wisdom tooth is indicated in the following cases:
- Excessive pressure on neighboring teeth, which can lead to their destruction;
- Injury to surrounding tissues;
- Constant biting of the mucous membrane of the cheek;
- Carious lesion that cannot be eliminated due to difficult access;
- Complications of caries: pulpitis, periodontitis, periostitis;
- Dystopia – location of the molar outside the dentition;
- A tooth that is a chronic source of infection;
- Formation of perihilar cysts, granulomas;
- Malocclusion and displacement of other teeth.
Wisdom teeth. Execution cannot be pardoned...
How to place commas correctly in the title? What do you need to know and what to guide you when deciding whether to preserve or remove these teeth that are problematic from a dental point of view? Let's try to figure it out.
“Wisdom teeth” or “eight teeth” usually appear in a person closer to 20 years of age, plus or minus a few years (much more often plus than minus)... Not everyone really becomes wiser by this age, but people began to call them that, hinting specifically at their late appearance. At the same time, despite the name, 8s don’t make us smarter, but we’ll get tired of listing the hassle. Why is this happening?
This is how it is in nature: everything that it does not need gradually disappears. Man has long been getting his food not in the forest, but in the supermarket, eating not raw tough meat and plant roots, but a refined Big Mac... Therefore, we no longer have a great need for so many chewing teeth and such large massive jaws as our ancestors had. And that’s why we are evolving in the direction of reducing jaws and the number of teeth. Even now there are quite a few “advanced” individuals in evolutionary terms who generally lack the rudiments of the 8th teeth (and not only them, but sometimes also incisors and canines, which is less pleasant). Although, at the moment, this is rather an exception to the general rule. But the lack of space in the jaws for all 32 teeth, on the contrary, is rather the rule. And since wisdom teeth are the very last to appear, they usually lack this very place in the dentition. That's why we have so many problems with them. This is just one of the factors, but perhaps one of the main ones.
Now let’s look at exactly what problems “wise teeth” can cause us.
Complete tooth retention.
Retention is a condition in which a tooth, for various reasons, could not erupt at the right time and in the right place. Well, with complete retention, accordingly, the tooth does not show out at all and remains lying inside the jaw.
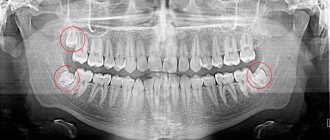
Red arrows show wisdom teeth, which lie completely in the thickness of the lower jaw. This is complete retention. Also, this patient naturally received a “bonus” of a completely impacted central upper incisor (shown by the blue arrow).
This arrangement could be considered quite good. Because the tooth lies inside the jaw, doesn’t touch anyone, doesn’t bother anyone... it would seem, and God is with it. In general, this is how it is. It’s probably not worth running as fast as you can to pick it out of your jaw. In this form, it can lie there all its life and not cause any trouble. Or maybe not entirely so. A so-called tooth may appear around such a tooth. follicular cyst. Therefore, it is best to observe such unerupted teeth by doing an orthopantomogram at least once a year*. Well... or remove such a tooth, forever forgetting about it and the need to monitor it. After all, there are many other things in life that you have to constantly think about and remember.
Partial retention.
By analogy, here we are talking about those cases when the wisdom tooth was still able to partially erupt, but not completely. What most often bothers him? Either a powerful bony protrusion of the jaw, or an incorrect position of the rudiment, or a neighboring 7... in general, there can be many reasons, the essence remains the same - part of the unerupted tooth remains inside, and part sticks out outside. This is the most common situation and it is this that most often leads to various really tangible problems. Which one exactly?
— pericoronitis is perhaps the most common complication of a partially erupted wisdom tooth. This is inflammation in the tissues surrounding this most problematic tooth - in the gums and bone. It manifests itself as pain, swelling and redness of the gums, difficulty swallowing, and fever.
In the farthest nook of the lower jaw you can see a partially erupted number 8 and the inflamed gum above it.
Often, patients try to self-medicate in such situations - they rinse the tooth with various drugs that are at hand (from chamomile decoction to five-star cognac), swallow painkillers uncontrollably, or, worse, antibiotics. Indeed, such measures (especially antibiotics) may subside the inflammation. But an unresolved cause will sooner or later lead to a relapse. Moreover, any inflammation in the area of wisdom teeth can easily develop into an abscess or phlegmon of the face and neck, and these are serious, life-threatening surgical problems. And they are treated, among other things, by making external incisions on the face and neck. And this is really serious. I won’t insert unappetizing pictures here; a query in any search engine will help create additional motivation for any unbelieving Thomas.
I hope I have scared you enough so that you don’t feel the urge to self-medicate in such cases. You definitely need to visit a dental surgeon. If he sees no problems in the further teething of the figure eight, he will simply remove the gum hanging over the tooth (“hood”) and prescribe the necessary medications. If the tooth objectively can no longer erupt normally, then it will need to be removed. This is the only way to eliminate the cause and protect yourself from relapses of inflammation, as well as from serious purulent complications of an initially trivial problem.
— caries of the root of the adjacent 7th tooth. Often, when the 8 is “stuck” and has no chance of cutting through further, but does not bother, patients do not even think about contacting a doctor, because "does not hurt". In fact, such a semi-erupted tooth makes it difficult to maintain normal hygiene in this area and this leads to caries damage to the neighboring tooth. Moreover, the most unpleasant thing about this option is that caries develops near the very base of the tooth, develops unnoticed, and the cavity can remain invisible for a long time. As a result, a huge “hole” grows, going deep under the gum, and it is not always possible to restore such a defect qualitatively. As a finale - the loss of a good neighbor due to the “wise tooth” not being removed in time. Moreover, it will be possible to make up for the lost 7 only with an implant (which is not cheap) or a removable prosthesis (which is inconvenient to use and significantly reduces the quality of life)
On the x-ray, the arrow shows a carious cavity that arose on the 7th tooth due to its careless, wise neighbor. On the right is about the same thing, only in a live photo. The stuck figure eight is shown in green, and the caries that arose on the number 7 as a result of it is shown in blue.
- resorption (simply resorption) of the root of the adjacent 7th tooth. In general, the situation is similar to the previous one, with the same consequences. The only difference is that, having rested against its neighbor, the “wise tooth” can turn out to be very persistent and, with its pressure on the 7th tooth, cause the resorption of its hard tissues.
On the x-ray we see a wisdom tooth resting on the upper 7th. In the photo on the right is the same seven, after removal. This is the kind of root resorption that a stubborn wisdom tooth can cause due to its pressure.
- loss of bone from the adjacent 7th tooth... this is the third variation on the theme that behind a problematic, but seemingly not bothersome wisdom tooth, an innocent, good and necessary neighbor can easily suffer. An incompletely erupted wisdom tooth, resting against the 7-point, can create a space in which food debris will accumulate. This will cause periodontal pocket formation and bone loss between the 8th and 7th. But the result is still the same - removal of both teeth, bone grafting and implantation of the 7-piece.
Here the wisdom teeth decided to create problems for their owner as a couple. The lower one collapsed and rested on the 7th, causing bone loss. The top one, deprived of his partner, crawled down to meet him. What happens from this - read on.
- chronic injury to the mucous membrane. Often crookedly erupted wisdom teeth (especially the upper ones) when chewing cause chronic injury to the mucous membrane of the cheek and gums on the opposite jaw. This is unpleasant both in itself and in terms of prognosis - any chronic injury to the same place can lead to malignancy.
An upper wisdom tooth that grows unevenly towards the cheek (the gray arrow points to its tubercle) causes chronic injury to the mucous membrane (yellow arrow)
- blocking normal movements of the lower jaw with the possible development of problems of the temporomandibular joint. This is a rarer problem, but it still occurs. Each tooth in the dentition has its own pair on the opposite jaw - an antagonist tooth. And 8s are no exception. When wisdom tooth is removed or does not erupt , the other, opposite one, moves out. As a result, it can block the movements of the lower jaw and cause it to shift into an unphysiological position when chewing. This can be completely asymptomatic until symptoms begin in the joint - clicking, crunching, pain... etc.
Here the top eight lost their antagonist “thanks” to natural forces...
...and here thanks to the strength of the dentist. True, when removing one eight, you should immediately think about removing the antagonist. Well... or immediately put an implant and a crown in place of the removed wisdom tooth... if life seems too simple and bland to you.
Well, now a few words about what could happen to wisdom teeth , which still managed to erupt in their place and quite evenly. Can they really cause inconvenience in such a situation? It turns out they can.
Erupted wisdom teeth.
The main problem with properly grown 8s, despite everything, is their inaccessibility... both for hygienic measures and for quality treatment. Laziness, haste, and an increased gag reflex are the most common reasons why the hygiene of wisdom teeth is, as a rule, insufficient to prevent the occurrence of caries on them. For the same reason, quality treatment is difficult. Poor visibility, difficulties with applying a rubber dam, frequent “exclusive” structure of the canals, making them difficult to pass even for well-trained and equipped endodontists, difficulty opening the patient’s mouth (and even with normal opening, getting close to the figure eight with an instrument is not so easy), the same increased gag reflex in the patient... All these objective difficulties often force one to make a decision to remove the apparently good 8-ok. Because it’s better to remove it well once and forget about the problem, than to redo the same tooth many times, and then... remove it anyway.
There are doctors who unreasonably expand the indications for the treatment of 8th teeth, i.e. seemingly showing genuine care for the patient’s teeth, but in reality... But in reality, what happens first is the treatment of small caries, after a short time - relapse of caries, then pulpitis, then periodontitis... and, finally, natural removal after a few years. It seems that nothing has changed, except that the doctor manages to remove several “harvests” from the same problem before actually solving it. This does not always happen maliciously; some actually believe that they are prolonging the life of 8s for the benefit of the patient. Moreover, patients themselves often ask for this. At the same time, I often heard from opponents of the removal of the 8th teeth that “there is always time to remove”, “what’s mine is mine and I won’t give it up for anything”, “then, if something happens to the 7th, it will be possible to install a bridge with a support at 8." I think all the previous examples speak quite eloquently about the fact that it is not always possible to “delete” on time. If it’s such a pity to part with your teeth in favor of the dentist, then you can take them away and make a stylish decoration for a long memory... both your health will benefit, and your wisdom will always remain with you.
As for 8s as a support for bridges, the time has already passed when it was possible to talk about this seriously. Today, implantation solves the problem of the absence of any tooth without the need to “sharpen” neighboring ones. In addition, wisdom teeth, in principle, should not bear the load of their more functionally loaded colleagues (6s and 7s), because They are not at all suited for this work. Try to force a podium model, who has been on diets all her life, not just to lift a barbell, but to set a new world record in women's weightlifting... I'm afraid she will simply be crushed by sports equipment that trained female athletes can easily lift. For to each his own... It’s the same with teeth. The 6th and 7th teeth have 3 or even 4 multidirectional powerful roots, which nature designed to withstand heavy chewing loads. And in the eighth teeth, the roots almost always grow together into a single monolith, which has a cone shape and is not at all so stable - God forbid it could hold itself in the jaw. And if some irresponsible orthopedic dentists try to put an additional load on such a root, then this 8 comes to an end quite quickly, just like the “weightlifter” model... Another trouble that orthodontists often have to deal with... 8s they can grow... and grow seemingly correctly and well, but at the cost of the fact that the remaining teeth will be completely shamelessly moved, and the doctor will state that your teeth are crowded .
And since this process is not momentary, it is usually noticed too late. The price of such inattention is the removal of 8s and wearing braces.
So, to summarize, in the vast majority of cases, eights are a real headache for both patients and dentists. Modern man (if he does not live in the forest the life of our distant ancestors) really needs them insofar as. Those. If your wisdom teeth have grown evenly and in their place, you are able to care for and cherish them along with everyone else, then, thank God! Let them chew. Although I can admit from my own experience, such lucky people are an overwhelming minority. If signs of one of the above-mentioned problems appear, then there is no need to hesitate, be afraid and regret losing a part of yourself... Wisdom teeth are far from the most valuable thing about us. And without them, life does not get worse, but rather the opposite. This “on the contrary” is what I wish for you!.. With or without wisdom teeth.
Removal of the lower impacted figure eight
A common complication is wisdom tooth retention, which is incomplete eruption. It can erupt above the gum as part of the crown or as one or two bumps. In this case, the second part of the crown will be covered with a gingival hood. With insufficient hygienic care, food accumulation, gum inflammation, and pericoronitis (inflammation of the hood) occur. In the case of pericoronitis, the dentist excises or cuts the gingival hood. But if the situation is constantly repeated and bothers you, then it is better to remove such a tooth. Chronic inflammation of the gums is a source of infection that spreads throughout the body and can provoke an exacerbation of other diseases.
Indications for figure eight removal
To remove a wisdom tooth or try to save it is a question that only an experienced dentist can answer, based on the clinical symptoms that concern the patient, the direction of tooth growth, the presence of an inflammatory process and other factors. Here is a list of indications in the presence of which it is worth getting rid of a problematic molar:
- abnormal location of the figure eight in the jaw bone - when the wisdom tooth grows evenly, this is rather an exception than a common situation. More often, the figure eight erupts at an angle, damaging the tissues of the cheek and tongue, destroying the roots of neighboring healthy teeth (sometimes they grow horizontally, without even appearing on the surface of the gum; a molar can only be detected on an x-ray);
- pericoronitis or too slow eruption of a molar is an indirect indication for removal; if the tooth is simply covered with a hood, then the doctor can remove part of the soft tissue to avoid the inflammatory process. Removal is carried out only when the patient has taken too long with his visit to the dentist;
- carious process - since it is difficult to fully care for eighth molars, this often leads to the development of caries due to the accumulation of bacterial plaque in the gingival hood;
- inflammatory process - if the infection has also affected the soft tissue of the gums, then it is better not to delay the removal of the problematic tooth, this can lead to the development of gumboil or the formation of a purulent cyst.
Complicated eruption of wisdom teeth
As already mentioned, whether it is worth removing a tooth is up to the attending physician to decide. The practice of foreign and Russian dentists differs; while European doctors prefer to extract eighth molars right away, Russian doctors are in no hurry to remove them (if the tooth has grown, it means it is not superfluous). Therefore, if the dentist insists on immediate surgery, it means there is a strong indication for it.
Anesthesia
Before the operation, complete anesthesia of the required area of the jaw is carried out. The most commonly used is local anesthesia, which is carried out using a carpule syringe and an anesthetic. Anesthesia of the lower jaw occurs 8-10 minutes after the injection. The duration of the analgesic effect depends on the drug used and is 2-4 hours. The operation itself is completely painless, but after the anesthetic wears off, the patient begins to feel pain. Therefore, after the procedure, the specialist gives prescriptions about the need to use medications (painkillers, anti-inflammatory, antimicrobial agents).
Easy removal
Simple extraction is the extraction of a tooth without the use of additional tools or techniques. A simple operation is observed after complete eruption, correct positioning of the molar, and the absence of serious pathologies. The doctor applies forceps and, after rocking movements, removes the molar from the jaw
The following stages of the procedure can be distinguished:
- Anesthesia;
- Selection and preparation of tools;
- Tooth ligament separation;
- Application and fixation of forceps;
- Luxation of a molar;
- Extraction from bone;
- Checking the hole;
- Stop bleeding;
- Recommendations for the patient.
Difficult removal
Removing a wisdom tooth in the lower jaw is often difficult. The operation differs in its duration, the use of a special instrument, and the use of a drill. Often the tooth is sawed and removed in parts. In this case, the figure eight is incorrectly positioned or impacted. Removal consists of the following steps:
- High-quality pain relief;
- Preparation of tools and auxiliary materials;
- Separating the tooth ligament or creating access;
- Application and fixation of forceps;
- Extraction of a molar in whole or in parts;
- Inspection of the bone socket, cleaning it if necessary;
- Stop bleeding;
- Stitching;
- Prescriptions and recommendations for the patient.
Removal process
Whether it is painful to have a wisdom tooth pulled out depends not only on the psychological mood of the patient himself (if he is tense, scared and does not want to cooperate with the dentist, the process may indeed not go so smoothly and may cause pain). Another factor influencing the course of the operation is the type of removal; whether a simple procedure will be performed or a complex one. The first step to consider is simple wisdom tooth extraction.
Easy removal
Simple extraction involves the use of only dental forceps and elevators; the process does not involve cutting the soft tissue of the gums, does not separate the roots, and does not use a drill to drill out the bone. Such a procedure, especially if carried out efficiently and carefully, is not accompanied by pain during and after extraction. Simple removal takes place in several stages:
- Anamnesis collection. The doctor asks the patient about complaints, conducts an external examination, and, if necessary, x-rays. The medical history is studied, allergic predisposition is assessed, concomitant diseases are determined, and blood pressure levels are measured. All of these factors can directly affect the course of the operation.
- Conducting anesthesia. Most dental clinics prefer to remove wisdom teeth using local anesthesia. Extraction under general anesthesia is carried out for critical indications and only in a hospital setting, under the supervision of an anesthesiologist.
- Extracting the tooth from the socket using elevators and forceps. An elevator is a special device consisting of a pear-shaped handle, a rod and a working part that acts as a lever. It is applied to the molar being removed, resting on the wall of the socket or adjacent tooth. A simple extraction lasts from 5 to 15 minutes, sometimes the process can take 30-40 minutes, after which the final stage begins.
- Removing the remaining parts of the tooth from the socket and washing the wound with antiseptic solutions. If there is evidence for this, the doctor will inject an anti-inflammatory drug.
After tooth extraction, dentists try to suture the gum to reduce the risk of wound infection and bring its edges closer together.
The process is not accompanied by pain, since the anesthesia is still in effect. Next, the doctor gives recommendations on proper care of the socket during the recovery period.
Difficult removal
For patients who had to have their wisdom teeth pulled out during Soviet times, the fear of dentists remained for many years, because previously the procedure was painful and lasted for several hours in a row. In modern clinics, a drill with a special bur, forceps, elevators and other equipment are used to separate the roots of the eighth molar and reduce the volume of bone tissue.
Previously, dentists' offices were poorly equipped; the doctor had to separate the roots with a chisel and hammer. The coronal part of the tooth was first broken off, and the tip of a chisel was placed on the interroot septum, which was hit with a hammer. If the dentist had the skill, he could divide the root in 1–2 strokes; in difficult cases, the procedure was delayed for several hours.
Perhaps this fact, preserved in the memory of many patients when removing figure eights was very painful, still frightens them, forcing them to delay a visit to the doctor.
Most often, the wisdom tooth is positioned incorrectly and grows at an angle, so an x-ray is necessary before removal. Almost no dentist will undertake an extraction without examining an x-ray, unless the situation is critical, when there is no time or opportunity to conduct an examination. The doctor will also pull out the complex figure eight in several stages:
- Anamnesis collection.
- Preparation for extraction - removal of hard dental plaque, rinsing the oral cavity with antiseptics.
- Carrying out anesthesia in the required dosage so that with the injection the patient does not feel pain for 2-3 hours in a row.
- Cutting the soft tissue of the gums, separating the roots using a drill and extracting them.
- Cleaning the hole from remnants of bone tissue, roots and sawdust.
- Smoothing the sharp edges of the socket using a drill or bone nippers.
- Wash the wound with antiseptic solutions and inject an antimicrobial drug (as indicated).
- Suturing the edges of the wound to avoid infection.
Particular attention is paid to patients whose eighth molar is impacted, that is, has not erupted
Many people face this problem when the dentition does not have enough space for full eruption. In this case, sharp pain occurs in the gums, since the molar growing sideways or horizontally is not visible above the soft tissue, but pushes the neighboring tooth from the inside. If the tooth still erupts on top, but is covered with a hood of gums, this often causes serious suppuration. Such situations require immediate surgical intervention.
Possible consequences after removal
Complications can occur after any surgical procedure. These include: bleeding from the wound, suture dehiscence, inflammation of the socket (alveolitis), increased body temperature over 38 degrees, numbness of the jaw, bone fragments or tooth remains in the socket.
A normal reaction of the body in response to surgery is the appearance of pain, discomfort, unpleasant sensations in the surgical area, a slight increase in temperature, swelling of the angle of the jaw, and facial asymmetry. These symptoms occur due to soft tissue injury, damage to blood vessels and nerve endings. The pain should subside over time and disappear after 5-10 days.
If after 3-4 days the pain does not decrease and the symptoms of inflammation increase, you should consult a dentist. The most unpleasant complication is alveolitis - inflammation of the socket of an extracted tooth. It manifests itself as acute pain, redness and swelling of the gum tissue, a significant increase in temperature, and general symptoms. The wound may discharge purulent contents or necrotic plaque. In this case, treatment by a dentist is necessary.
Types of Impacted Teeth
The term “impacted” can be applied not only to “eights”, but also to other teeth that are hidden in soft tissue. Depending on the degree of immersion of the tooth in soft tissues, complete or partial retention is distinguished. In addition, the depth of the tooth is also important. If it is located in bone tissue, then it is an impacted tooth with bone immersion. There is also the concept of an impacted dystopic tooth, that is, one that is located out of place or grows at the wrong angle (the so-called displacement of the dental axis). There may be several options here:
- medial impacted tooth (tooth tilted forward);
- distal impacted tooth (tooth deviates backwards);
- horizontal impacted tooth (the impacted tooth is located horizontally relative to the dentition);
- reverse impacted tooth (the tooth is upside down - the root part is located at the top and the coronal part is at the bottom).
Prevention after surgery
After the last molar is removed, the specialist gives instructions that must be strictly adhered to. This is done to prevent complications, speed up wound healing and restore the body. The doctor recommends:
- Do not eat food for several hours after surgery;
- On the first day, you can apply a cold compress to reduce swelling and inflammation;
- For the first two days, you should not rinse your mouth, so as not to remove the blood clot from the hole from which healing will occur;
- Hygienic care can be carried out as usual; teeth in the surgical area should be brushed very carefully;
- Take painkillers and other medications prescribed by your doctor;
- From the second day, the mouth can be rinsed with antiseptic solutions, decoctions of medicinal herbs, and mouth rinse;
- It is recommended to eat soft foods, avoid too hard, spicy, hot foods;
- Bad habits (smoking, drinking alcohol) should be eliminated;
- During the week you cannot visit the sauna, bathhouse, or gym.
Clinical researches
Asept products are clinically proven effective. For example, clinical studies have proven that regular use of professional toothpaste ASEPTA REMINERALIZATION improved the condition of the enamel by 64% and reduced tooth sensitivity by 66% after just 4 weeks.
Clinical studies have proven that regular use of professional toothpaste ASEPTA COFFEE AND TOBACCO for a month improved the hydration of the mucous membrane by 3.3 times, the remineralizing efficiency increased by 3.9 times, at the same time, the cleansing effect has increasing dynamics and reaches 60 .5% at 4 weeks of use.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- Report on the determination/confirmation of the preventive properties of personal oral hygiene products “ASEPTA PLUS” Remineralization doctor-researcher A.A. Leontyev, head Department of Preventive Dentistry, Doctor of Medical Sciences, Professor S.B. Ulitovsky First St. Petersburg State Medical University named after. acad. I.P. Pavlova, Department of Preventive Dentistry
- Report on determining/confirming the preventive properties of toothpaste “ASEPTA PLUS” COFFEE and TOBACCO Author: doctor-researcher A.A. Leontyev, head Department of Preventive Dentistry, Doctor of Medical Sciences, Professor S.B. Ulitovsky. First St. Petersburg State Medical University named after. acad. I.P. Pavlova, Department of Preventive Dentistry
- The effectiveness of the use of Asept “adhesive balm” and Asept “gel with propolis” in the treatment of chronic generalized periodontitis and gingivitis in the acute stage (Municipal Dental Clinic No. 4, Bryansk, Kaminskaya T. M. Head of the therapeutic department Kaminskaya Tatyana Mikhailovna MUZ City Dental Clinic No. 4, Bryansk
Bleeding
If bloody discharge appears from the socket of an extracted wisdom tooth, you should call your doctor and report the situation. Minor gum bleeding can occur due to tissue injury, high blood pressure, or problems with blood clotting. In most cases, this does not threaten health and goes away on its own. If bleeding is severe or frequently repeated, you should inform your doctor and come for an examination. To prevent complications, you should rest more for several days, avoid physical activity, and monitor your blood pressure.
Pain in the socket
Everyone experiences pain after removal surgery and worries for several days. The intensity of pain will depend on the traumatic nature of the operation and the complexity of the surgical interventions. During the postoperative period, the dentist recommends using painkillers. If the pain does not disappear, but intensifies after 3-4 days, this may indicate complications. A professional examination and consultation with a doctor are required.
Causes of retention
As you know, wisdom teeth are largely a vestigial organ and have lost their importance in the process of evolution. About 10% of the world's population does not have the rudiments of wisdom teeth at all, while in others they erupt without complications and harmoniously take their place in the dentition. There is a third option, when a person has the beginnings of wisdom teeth, but various difficulties arise during eruption. Retention is one of these complications. Among the most common causes of such teeth, experts identify:
- hereditary factor;
- early loss of baby teeth (removal of an impacted wisdom tooth in a teenager is often associated with this factor);
- too dense or thick gingival walls;
- crowded dentition and malocclusion.
When should a wisdom tooth in the lower jaw not be removed?
There are no absolute contraindications to removal, but there are relative ones:
- The figure eight does not need to be removed if it is correctly positioned, functions and does not injure surrounding organs;
- The operation cannot be performed without preliminary preparation if the tooth is located in the area of the tumor or puts pressure on a large vessel or nerve;
- For some diseases, it is necessary to prepare the body for surgery (rheumatism, diabetes, blood diseases, etc.)
You can carry out high-quality removal of a wisdom tooth of any complexity at the Berezka dental clinic. Specialists perform various surgical procedures effectively, safely and painlessly. All manipulations are carried out professionally and taking into account the individual characteristics of each patient.
Possible complications after extraction
After removal of the extreme molar, patients experience swelling and swelling in the cheek and gum area, numbness of the face, moderate bleeding, discharge of ichor and pain. Moreover, these manifestations are companions of non-infectious inflammation and are considered the norm. They do not pose any danger and will disappear within a few days if the healing process is normal. The rehabilitation period after wisdom tooth removal lasts about one to two weeks.
More serious side effects should be expected if errors were made during the operation, or if the patient himself took the doctor’s recommendations lightly and violated the rules of rehabilitation.
A common complication after tooth extraction is osteomyelitis - an inflammatory lesion of bone and soft tissue. Suppuration begins inside the tissues. Osteomyelitis occurs if an infection gets into the socket during or after surgery. There is an increase in temperature, severe swelling of the gums and cheeks, severe persistent pain, general weakness, sleep disturbance and headaches.
Without medical intervention, infection and sepsis may spread.
Other consequences include abscess, paresthesia of the tongue, gumboil, and neuritis. All pathologies are accompanied by pain and deterioration in well-being. Therefore, if after one and a half, maximum two weeks, the pain, discomfort and swelling have not completely gone away, you should consult a dentist.
Wisdom tooth removal is a complex operation, and all risks should be carefully weighed before planning it. These teeth should be removed only if there are serious medical indications, and if there is an opportunity to save them, then it is worth taking advantage of it.