Can just one bad tooth cause great suffering for a physically healthy person? – Maybe, if we are talking about pulpitis
.
How this insidious disease manifests itself, what factors lead to the development of pulpitis and what its treatment is - read in our material.
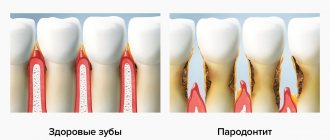
Pulpitis
is an inflammatory reaction of the pulp caused by internal or external traumatic factors. The pulp itself, or the dental “nerve,” is the soft and fibrous connective tissue in the cavity of the tooth, penetrated by lymphatic and blood vessels. There are a great many nerve endings inside the pulp, which is why toothache with pulpitis is considered one of the most severe.
From the history
Long before the advent of modern dentistry, medieval aesculapians knew that exposure to the dental “nerve” provokes unbearable pain. The executioners of the Inquisition also possessed this knowledge, who used primitive instruments like drills for torture - with twisting movements they crumbled enamel, destroyed dentin and reached the dental nerve, causing unbearable pain in the subject. Such torture could last for more than one day, the subject was brought to his senses and the painful execution was repeated again and again until the exhausted person died from traumatic shock.
How does pulpitis occur?
The occurrence of pulpitis
It is generally accepted that caries, especially in an advanced stage, is the most common cause of pulpitis. However, the development of the disease can also be a consequence of tooth trauma, and a consequence of improper treatment by an unqualified dentist.
There are several ways of infection of the pulp and, as a consequence, the occurrence of pulpitis:
- through the crown of the tooth, when the carious cavity grows, becoming a gateway for the penetration of microbes and pathogenic bacteria into the dentin and further into the pulp;
- through the apex of the tooth root (retrograde pulpitis).
Due to its specific pathogenesis, retrograde pulpitis is a rather rare occurrence. The following factors can provoke it:
- infection of the pulp through the blood in systemic viral diseases such as rubella or herpes;
- infection of tooth roots through the maxillary sinuses during sinusitis.
At the same time, one of the most common causes of pulpitis are dental errors:
- a poorly treated carious cavity is untreated caries, which leads to re-infection of dentin and the development of caries already under the filling;
- thermal burn of the pulp due to insufficient water cooling or overdrying of the tooth cavity during treatment;
- chemical damage to tooth tissue during treatment.
! You can protect yourself from the consequences of treatment by an unscrupulous dentist in advance by contacting a well-known dental clinic with a name and reputation. High-tech equipment, the availability of modern equipment and a staff of professional dentists will allow you to undergo a full diagnosis and receive timely, qualified treatment.
What is it – tooth pulpitis?
Pulpitis is a dental term that refers to an inflammatory process that affects the nerve bundle inside the tooth - the pulp. Colloquially, the pulp is often called the nerve of the tooth. Strictly speaking, the pulp is not only nerves, but also small blood vessels, thanks to which a living tooth receives nutrients and necessary microelements. If the pulp is removed (and this often happens during the treatment of pulpitis), the tooth becomes dead and fragile because it does not receive the nutrition necessary for its full functioning and healthy condition.
The inflammatory process in the pulp never occurs on its own - there are always reasons that trigger it. Knowing the reasons why pulpitis appears is necessary and useful; this will make it possible to carry out effective prevention of this dental disease.
Take a short test and calculate the cost of treatment!
Take a short test
Diagnosis of pulpitis
Diagnosis of pulpitis
When it comes to pulpitis, the occurrence of a pronounced pain syndrome is explained simply: the inflamed pulp in the edema phase increases in size, which leads to compression of nerve cells, and as a result, severe pain. You should not try to determine the diagnosis yourself, and if you experience toothache, you should immediately contact your dentist. If time is missed, the infection can spread and lead to serious complications: periodontitis, periostitis and osteomyelitis.
Professional diagnosis of pulpitis is extremely important; further treatment and prognosis for recovery depend on it.
! According to statistics, about 60% of pulpitis is chronic, and acute accounts for about 40%.
Usually, during an examination, the dentist questions the patient about the intensity and location of the pain, finds out when the tooth first became ill, and whether the pain intensifies at night. Previous viral diseases, stress or dental interventions can provoke an exacerbation of pulpitis.
The simplest and therefore most frequently used diagnostic methods include: visual inspection, percussion, probing and radiography.
.
Sometimes dentists diagnose the disease using electroodontometry
, determining the vitality of the pulp by its reaction to an electrical impulse. This method allows you to determine the shape of pulpitis most clearly.
Percussion
This type of diagnosis is carried out along with a patient interview and visual examination, but in itself it is not always informative. The doctor performs a percussion test by lightly tapping the instrument on the surface of the tooth. Percussion of a healthy tooth does not cause painless sensations and is accompanied by a clear and distinct sound. If the pulp is affected or periodontitis is present, the nature of the sound changes, as does its clarity and volume. The presence of inflammation in the periodontium is also revealed by a clinical pressure test - for 30 seconds the doctor applies pressure with his finger on the teeth, and if by the end of the pressure the patient experiences pain and a feeling of numbness, the test is considered positive.
Probing
In the presence of obvious caries, the walls of the cavity are first probed, which is usually painless in case of pulpitis. To make an accurate diagnosis, the doctor evaluates the sensitivity of both the walls and the bottom of the cavity, determines the visibility of the pulp in the carious cavity, its color and the presence of bleeding.
In cases of old, untreated pulpitis, the presence of a large amount of pigmented, loose dentin is determined in the cavity, and when palpating the transitional fold, the patient feels acute pain.
Radiography
Radiography is used to visualize the tooth and determine the localization of the pathological process. This method plays an important role in the diagnosis of pulpitis, and also helps the doctor assess the condition of the periapical tissues of the tooth in order to select subsequent treatment tactics.
Electroodontodiagnosis
Diseased and healthy teeth react to different current strengths, therefore, using electroodontodiagnosis (EDD), it is possible to assess the vitality of the pulp. The doctor determines whether the tooth can be treated and restored or should be removed. Because a tooth may react differently to electrical shocks in different situations, the diagnosis must take into account many factors, including the presence of chronic systemic diseases and the patient's age. External factors, for example, nearby UHF and microwave devices, can also influence the result of electrodiagnostics. Despite the fact that the electroodontic diagnostic method is accessible and informative, due to the large number of contraindications it can only be used as an additional method. To avoid obtaining false results, a competent and responsible doctor follows the research methodology and always acts exclusively in accordance with the instructions for the device.
Forms of pulpitis
The forms of pulpitis differ in the nature of the course of the disease and in localization. According to localization, coronal, total and root pulpitis are distinguished. According to the nature of the disease – acute and chronic.
Complications of pulpitis
If you do not consult a dentist in a timely manner, pulpitis can develop into a more serious disease - periodontitis, cyst or granuloma, periostitis. That is, the inflammation will go deeper and go beyond the tooth root. Such complications can lead to tooth extraction, after which neighboring teeth will begin to shift, leading to malocclusion. Since the disease causes some discomfort while chewing food, the patient may face serious gastrointestinal problems.
Acute pulpitis
- Focal
Pulpitis, in which inflammation affects only part of the pulp; manifested by severe paroxysmal pain every 5-7 hours for 10-15 minutes; the patient can pinpoint the tooth that is the source of the pain.
- Diffuse
Pulpitis, in which inflammation covers the entire pulp; attacks of pain last up to one hour, and sometimes longer; the pain radiates to neighboring teeth and gradually covers the entire jaw and head.
- Purulent
With this form of the disease, irreversible dissolution of the pulp tissue occurs, the pain becomes unbearable; A characteristic sign of purulent pulpitis is dulling of pain when exposed to cold, so the patient often spends time waiting for a doctor with a bottle of cold water applied to his cheek.
- Traumatic
Occurs after trauma to the jaw, after treatment or fracture of a tooth, when the pulp is exposed and causes acute pain when breathing, touching and at rest.
What is special about wisdom teeth?
The maximum set of molars for an adult is 32. In this case, it is considered normal to have 28 teeth, since four teeth are the so-called eighth molars or wisdom teeth. For some, they do not erupt at all, for others, when “eights” appear, complications and pathologies arise, but in other cases, wisdom teeth occupy the correct position in the dentition and do not bother their owner. “Eights” usually appear between the ages of 17 and 27, that is, during the period when a person has already formed an attitude towards hygiene and his own dental health. Why is it important? Due to the remote position of wisdom teeth, it is quite difficult to carry out high-quality cleaning, so only very good hygiene can reduce the risk of dental damage. In reality, it is the third molars that are in the top in terms of the number of cases of caries and its common complication - pulpitis.
Chronic pulpitis
- Fibrous
The symptoms are not pronounced, so the patient may not pay attention to such pulpitis for years;
- Gangrenous
Acute untreated pulpitis, which has passed into the chronic stage, accompanied by suppuration, tissue necrosis, discoloration of enamel and bad breath.
- Hypertrophic
Pulpitis, in which a bleeding polyp is already visible in the tooth cavity, causing pain when chewing.
How to prevent the development of dental caries?
Good dental hygiene helps prevent the development of dental caries, and regular dental examinations detect caries at the very beginning and prevent complications. The distant teeth - wisdom teeth - can be difficult to access for self-cleaning. Maintaining a good level of hygiene requires professional teeth cleaning. Plaque removal using the Air Flow method cleans the most difficult to reach areas. Visiting a hygienist twice a year is a reliable prevention of caries and gum inflammation. Read more about caries prevention measures and dental hygiene here.
Pulpitis in a child
Pulpitis in a child
It is a mistake to believe that treatment of baby teeth is not necessary. Without adequate treatment, caries of a baby tooth in a child, just like caries in an adult, can very quickly turn into pulpitis with all its complications. There are known cases of death after complications of pulpitis due to the development of sepsis, when no more than two days passed from the first pulpitis pain to the development of facial edema and subsequent death.
To avoid any kind of complications, caries of primary teeth in children must be treated on time. And if the moment is missed and pulpitis has already developed, you need to contact the dentist immediately. A competent doctor will do everything possible to ensure that the treatment of a small patient is as painless, comfortable and, most importantly, effective.
Stages and stages of tooth treatment for pulpitis using the devital method
- Stage I.
The tooth is anesthetized and the carious cavity is cleaned. The pulp cavity is opened. - Stage II.
A devitalizing paste is placed into the exposed pulp and the tooth is filled for 3 to 7 days. People still call the paste “arsenic,” although it has nothing to do with this substance. - Stage III.
During your next visit, your dentist will clean the root canals according to medical protocol. - Stage IV.
If there is a risk that the tooth will crack, it is covered with a crown. If the hard tissues are well preserved or only slightly damaged, they are restored. The tooth is strengthened with a fiberglass or metal anchor pin and securely filled with photopolymer material.
The treatment time for pulpitis depends on how damaged the tooth is, the age of the patient, whether there are complications, and how many root canals should be treated.
The most vulnerable teeth
The most vulnerable teeth
Inflammation can develop in any tooth, but there are certain groups of teeth that are more susceptible to pulpitis than others.
The first place in the risk group is occupied by molars or upper sixes. They erupt earlier than others and are in the most vulnerable zone. So the appearance of dark spots on these teeth in a child is not perceived by parents as an alarming signal, therefore, as the process worsens, there comes a time when the child begins to complain of unbearable pain in the tooth - and this is already pulpitis.
2nd place belongs to the upper lateral incisors. But the lower front teeth and canines are least susceptible to such ailments as caries, which means they are practically not threatened by pulpitis. However, it should be borne in mind that it is the lower teeth that most often suffer from the deposition of tartar on them.
Reasons for the development of the disease
- untreated caries or poor quality of filling, when an inflammatory process has developed again under the installed filling,
- preservation of the nerve under the crown - in this case (if the tightness of the prosthesis is broken, there is inflammation underneath) there is a high risk of pulp inflammation,
- tooth injury – inflammation penetrates from the outside, i.e. through cracks and chips that are located on the root or in close proximity to it,
- exposure to aggressive stimuli - temperature and chemical, for example, during previous canal treatment, naturally, with an incorrectly selected dosage of the drug.
Consequences of pulpitis
Consequences of pulpitis
The biggest mistake that some patients make when experiencing toothaches is the desire to endure them, drowning them out with painkillers. This often leads to the development of dangerous complications of pulpitis, acute or chronic periodontitis. In addition to unbearable throbbing pain, high body temperature and complete loss of ability to work are added. Seeing a doctor at this stage of the disease is accompanied by increased psychological and physical discomfort for the patient, and after treating the tooth cavity, where the pulp was previously located, purulent contents with an unpleasant odor come out.
When periodontitis that arises against the background of pulpitis enters the chronic stage, fistulas with purulent contents form on the gums. This stage of the disease is considered the most dangerous to human health. Patients who have passed this stage remember for the rest of their lives the terrible picture of hanging “pus pockets” from their newly extracted teeth. Whenever at this moment it becomes clear that sometimes it is better to prevent than to treat. However, complications of pulpitis can lead not only to tooth loss, but sometimes serious diseases develop that threaten the patient’s life: phlegmon, abscess and sepsis.
Phlegmon leads to the fact that the patient’s general well-being sharply deteriorates, body temperature rises to a critical level, the shape of the face is distorted, and in addition to pain, a feeling of fullness in the jaw occurs. Sepsis is a blood poisoning and the most dangerous complication of untreated pulpitis, in which death cannot be ruled out.
Are you still wondering whether to see a dentist?
Pulp is the general name for the “internal organs” of a tooth. To understand what root canal treatment is, why it is needed, and what the criteria are, let’s look at the structure of the tooth.
A tooth has two main parts: the crown and the root. Inside each tooth there are cavities that are filled with loose fibrous connective tissue - pulp. In the past, root canal treatment was called “removing the nerve.” But the nerve is only one of the components of the pulp.
tooth structure
A tooth is a whole living organ. Through the apex of the tooth root – the apex – a bundle of blood and lymphatic vessels and nerve endings enter the tooth. When, due to advanced caries or as a result of injury, the enamel and dentin of a tooth are damaged, the infection penetrates inside, into the pulp, and inflammation of the internal tissues of the tooth occurs - pulpitis.
Depulpation or treatment of pulpitis includes two main points: cleaning and filling . This is significantly different from installing a regular filling. During cleaning, the doctor removes all the inflamed pulp from the coronal part and all the root pulp. In order to do this efficiently, there are modern diagnostic methods, including computed tomography (CT) and work with a microscope. They allow you to accurately assess the number of root canals, their location, shape and degree of destruction.
depulpation
Until some point, it was believed that the upper sixth teeth had three roots, but now in 80% of cases there is an additional fourth root canal. The lower incisors have one canal, but additional branches can often be seen on a CT scan or under a dental microscope. Previously, they went unnoticed, which means they were infected. The infection spread, complicated inflammation occurred, and the tooth was destroyed. Modern dental techniques, such as the use of CT scans and microscopes, give doctors more opportunities for accurate diagnosis.
The first important criterion in the treatment of pulpitis is maximum cleaning of the canals. They need to be passed all the way to the apex, to the very apex, where the neurovascular bundle enters the tooth. This is done mechanically using special tools, so-called files. After this, the root canal is expanded, removing all the inflamed pulp, and a taper is created so that it can be properly filled with filling material.
Channels are often curved, have micro-branches, and their mechanical processing is limited. On the first visit, after mechanical cleaning, a preparation is left in the tooth, which chemically sterilizes the branches of the canals that are inaccessible for mechanical treatment. After a while, the canals are filled and the tooth crown is restored.
We always try to keep teeth alive so that they perform their functions well. A pulpless tooth is a dead organ. It is like a prosthesis that is neither capable of regeneration nor of perceiving too cold or hot to protect itself. But there are situations when, due to caries or injury, the pulp is damaged, becomes inflamed, and that very familiar toothache occurs, which, due to a natural change in the blood supply to the body, intensifies by night. Previously, arsenic was applied under a temporary gluten filling, and then the nerve was mechanically removed. For such manipulations, dentists are feared at the genetic level. But today in modern clinics, treatment of any pulpitis is accompanied by anesthesia, and patients do not experience any pain.
What are the criteria for treating teeth with pulpitis? They often think that it is enough that the tooth does not hurt and there is a filling. But even if the tooth hurts for 3-4 days or a week without treatment, the pulp dies. Due to infection, the nerve, blood vessels and tooth become dead. But if the pain goes away, this does not mean that the tooth has recovered! It becomes a hidden source of infection, and the next stage may develop when the infection progresses further. The tooth is secured in its bed by a system of ligaments. The space between it and the jaw is filled with connective tissue - periodontium. If the pulp in the tooth has already died, it will become a source of infection, which passes into the periodontium and then we get periodontitis - inflammation of the root tips and tissues around the tooth. In this case, the body tries to localize the source of inflammation, and a cyst may appear (from the Greek κύστις “bubble”). This is a cavity that fills with exudate (pus), and from which bone destruction can begin.
In a living tooth, a possible reaction to cold/hot due to enamel defects quickly passes because the tooth is restored. But if the pulp is inflamed, then under the influence of chemical and mechanical irritants it will hurt for a long time. Depending on the stage of inflammation, the duration of pain increases. As soon as the inflammatory process moves to the periodontium, we begin to feel pain when biting. This happens because the ligaments on which the tooth is suspended in its socket normally absorb pressure. But if the tooth is sick, then the inflamed receptors perceive any pressure as an excessive load and signal about it.
The immune system can hold back the development of such hidden inflammatory processes for some time, but as soon as the immune system is weakened, due to banal hypothermia, the amount of exudate can begin to increase sharply, and then we see gumboil and facial asymmetry. This is already inflammation of the periosteum. There is also a milder course of periodontitis, when a fistulous opening is formed on the gum, and during exacerbation, pus comes out of it. In patients, it happens that something swells, then goes away, an abscess appears and goes away. The presence of a fistula may be an indication that there is a problem with the roots of the teeth.
It is important for patients to know that even high-quality root canal treatment involves depulping the tooth. The tooth becomes dead, and this has much more difficulties than treating caries.
Timely diagnosis, prevention and treatment will save you from complex root canal treatment. But if it has come to this, it is important to understand that this is a responsible operation. It is not quick, it is not cheap, but it is necessary. Root canal treatment can take a long time – two to three visits. This depends on the number, shape of the root canals and the degree of infection.
Treatment of pulpitis
As soon as the diagnosis of “pulpitis” is made, the dentist begins to treat it using one of the methods: preserving the entire pulp, with its partial or complete removal from the root canal system.
The method of preserving the entire pulp is currently not popular, since such treatment often causes a large number of complications. Of course, each case of pulpitis treatment is individual, but in most situations, dentists still choose the third treatment option - complete removal of the pulp.
In cases where, due to the structure of the canal, it is not possible to go through it completely, the doctor uses the method of partial removal of the pulp.
Stages of endodontic treatment
If a patient consults a dentist at the initial stage of pulpitis, treatment is considered simple and usually takes place in one visit. When pulpitis is advanced, long-term treatment in several stages is required.
Stage one
Introduction of anesthesia, isolation of teeth using a rubber dam - a special latex lining.
Stage two
Cleaning dental canals from bacteria, providing access to them through a prepared carious cavity, removing the roof of the pulp chamber and providing access for instruments to the canals.
Stage three
The canals are treated using mechanical and chemical methods. At this stage, it is very important to determine the true length of the canals, for which the doctor enters files into them and takes an x-ray.
The doctor carries out chemical disinfection using disposable dental needles. The use of pastes for pulp necrosis involves the use of special antiseptics or medications for additional disinfection of the canals. Depending on the chosen treatment tactics, the process can take from one to four days.
Stage four
After making sure that the canals are completely cleaned, the doctor proceeds to the final stage - filling. However, after filling the canals, the full treatment of pulpitis is not considered complete. To speed up the recovery process, an experienced dentist must prescribe procedures that will minimize post-filling discomfort and help avoid inflammation.
Treatment methods
Treatment of pulpitis is carried out in a complex: as a rule, the nerve is removed (only in rare cases, when there is slight inflammation, it can be treated with medication and thereby kept alive for some time). After this, the canals are filled and the coronal part is restored if it is destroyed. Diagnosis and treatment monitoring are necessarily carried out using an x-ray - a targeted image of one tooth.
Dental canal treatment The dental canals are cleaned using special instruments and medications. The treatment takes 2 visits - during the first, the nerve is removed and the cavity is thoroughly cleaned. In the second, the quality of the treatment is assessed, the temporary filling is removed and a permanent one is placed.
Price:
from 4,500 rubles more details about the solution
Installation of a core tab After cleaning the dental canals, if the crown is almost completely destroyed, i.e. under the root, it is necessary to restore the tooth. An inexpensive option is to install a pin, but a more rational option is to make a stump tab that completely replicates the structure of the root system. This way the load is distributed more evenly, so the tooth will last longer. Next, you can install a crown or line the top of the inlay with a composite material.
Price:
from 5,000 rubles more details about the solution
Installing a crown Installing a crown after treatment of pulpitis may be necessary if the apex of the tooth is destroyed by more than half. For the lateral teeth, the best option would be to use metal-ceramics, for the front teeth - pure ceramics. In both cases, a crown made of zirconium dioxide is suitable, since it is characterized by increased strength and at the same time has a snow-white tint. A single prosthesis can be attached to the tooth itself (if there is something left of it), or to a pin or core tab.
Price:
from 11,000 rubles more about the solution
Recovery period
Once treatment for pulpitis is completed, the patient will need some more time to fully recover - from one week to a month. During this period, physical therapy is indicated, for example laser therapy using a helium-neon apparatus. This is necessary to speed up the healing process and consolidate the therapeutic effect.
Since pulpitis is an inflammatory disease, after treatment in the clinic it is necessary to take a course of non-steroidal anti-inflammatory drugs at home, such as: Ibuprofen, Ketanov, Naproxen-Acri. However, it should be remembered that all anti-inflammatory and painkillers have their contraindications, so the choice of a specific medication must be agreed with your doctor.
Pulpitis and periodontitis of wisdom teeth
Pulpitis is an inflammation of the internal neurovascular tissue of the tooth. Most often, the disease becomes a consequence of untreated caries. Pulpitis requires root canal filling. If the canals are passable and the tooth is in the correct position, the doctor will attempt to save the tooth. However, the above circumstances will be taken into account: prognosis with prosthetics and the presence of an antagonist.
Periodontitis is the formation of a cyst at the apex of a tooth root. When planning therapy, the doctor will also examine the patency of the canals and calculate the pros and cons of keeping the tooth in the mouth. The patient should remember that the upcoming treatment will be lengthy, will last for months, and therefore financial costs will increase.
Dial-Dent specialists who treated wisdom tooth pulpitis
- Orthopedic dentist S.V. Zukor – diagnostics, drawing up a comprehensive plan for treatment and dental prosthetics.
- Dentist-endodontist O.A. Shchelkanova – treatment of wisdom tooth canals with a microscope, tooth restoration with a composite.
- Dental assistants L. Kharlamova, A. Antoshkina.
See other examples of dental treatment at Dial-Dent here.
Make an appointment for a consultation by phone +7-499-110-18-04 or through the form on the website. You can ask questions about dental treatment and prosthetics to the chief doctor of the clinic, Sergei Vladimirovich Tsukor, on his page on
Forms and symptoms of pulpitis
Patients usually think that the main sign of pulpitis is pain and a large carious cavity in the tooth, but this is not entirely true.
There are acute and chronic forms of pulpitis, depending on the strength of the inflammatory process affecting the pulp. Severe pain, which is often not relieved by painkillers, is characteristic of the acute form of the disease. But, if it becomes chronic, the pain subsides and practically does not bother you anymore.
As for large “holes” in a diseased tooth, the patient may not see them. Pulpitis also occurs as a result of caries hidden under a thin layer of enamel and under a previously installed filling. The pulp can become inflamed in a tooth without caries, although this happens much less frequently, due to an infection brought into the tooth with blood.