For patient comfort, dental extractions and some types of dental treatment are performed under anesthesia. This allows operations and therapeutic procedures to be performed painlessly.
In some patients, the decrease in sensitivity occurs only in the area where the anesthetic drug is administered, while in others it spreads to adjacent tissues - lips, cheeks, chin.
Normally, the effect of the anesthetic lasts several hours. How much exactly depends on the type of anesthesia:
- for infiltration – 3-4 hours;
- for conductor – 5-6 hours.
If the feeling of stiffness does not go away the next day after visiting the dentist, we may be talking about paresthesia.
Content:
- Why does paresthesia occur after tooth extraction?
- How it manifests itself
- How to treat 3.1. Medicines for paresthesia 3.2. Physiotherapy 3.3. Surgical treatment of paresthesia
- Why paresthesia needs to be treated
- How to avoid paresthesia
Sometimes surgery to remove a molar tooth leads to complications. If after it the tongue, lip, chin become numb, taste sensations disappear, they speak of paresthesia. In most cases, this unpleasant condition goes away on its own within one to two weeks, but it happens that it is not possible to do without special treatment.
Mechanism of nerve injury
There are several types of nerve injury. The first and most common complication is direct mechanical injury from the instrument. Trying to remove the broken tip of the tooth, the doctor unnecessarily expands the boundaries of the hole with a drill and often touches the perineurium with a cutter. Also, strong pressure from the elevator on the bottom of the socket, working with root elevators “towards oneself” and “from oneself” leads to destruction of the wall of the mandibular canal and nerve injury. Clinically, at the time of injury, the patient experiences unbearable pain that can be compared to an electric shock with pain radiating to the teeth and lower lip. This type of injury leads to persistent paresthesia, which will last for several months; in some cases, complete restoration of sensitivity is not observed.
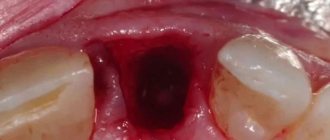
Another mechanism of nerve injury is associated with its compression (squeezing) by the tooth root during its luxation and traction. This mechanism is associated with the anatomically close, contact, location of the tooth root and the mandibular canal. In such patients, clinically and radiologically, the root of the impacted molar is part of the wall of the mandibular canal (Fig. 1,2). The root of the tooth in these cases can be the side wall of the canal, the upper wall, or surround the canal with a root bifurcation. The author had to observe a case when the mandibular canal passed through an impacted tooth, while all the walls of the mandibular canal were represented exclusively by the tissues of the tooth root. When the tooth root is in contact with the mandibular canal, removal often leads to compression of the neurovascular bundle. The patient experiences postoperative paresthesia of the teeth and lower lip, which lasts on average from one to six months. It is important to note that paresthesia in these cases requires treatment, the prescription of neurotropic drugs and physical therapy. If, after the removal of the third molar, the doctor observes in the tooth socket an open area of the neurovascular bundle not covered by bone, it is important not to curettage the bottom of the socket, not to use antiseptics, or to tightly tamponade the socket. The main symptom of nerve compression during extraction is pain when the instrument impacts the tooth root. It is important to distinguish between pain from incomplete anesthesia and pain from nerve compression. If, when dividing a tooth with a drill into a crown and roots (contact with the pulp), the patient did not experience pain, but when removing the roots, he feels acute pain - most likely there was compression of the wall of the mandibular canal and compression of the neurovascular bundle. Most often, such cases occur when the nerve passes on the side of the root of the third molar (usually with one root). In this position, tooth dislocation in the bucco-lingual direction leads to compression. If loosening of a tooth in one direction is painful for the patient, the tooth socket should be expanded on the opposite side and traction should be applied in the direction opposite to the area of compression.
Rice. 1. Contact location of the mandibular canal and the root of an impacted tooth (CBCT). The tooth has a recess through which the neurovascular bundle passes. When removing such a tooth, there is a high risk of nerve compression.
Rice. 2. Anatomical notch in the root through which the neurovascular bundle passes.
Why does paresthesia occur after tooth extraction?
Most often, the problem arises as a result of the “eights” being pulled out.
This is explained by the peculiarities of their location and non-standard direction of growth. The roots of the wisdom teeth go close to the nerve, so during the operation the doctor may inadvertently damage the latter.
Among the reasons for the development of paresthesia after wisdom tooth removal:
- The abnormal location of the unit, the presence of too long and curved roots - when extracting it, it is easy to touch a nearby nerve.
- The opening of severe bleeding after surgery, the appearance of pronounced swelling in the wound area. Because of this, the nerve endings are compressed, do not receive the nutrition they need and begin to work incorrectly.
- Careless actions of the doctor when administering an anesthetic - the needle can damage the lower alveolar process or lingual nerve. Then the tongue, lip and chin become immune to external mechanical influences.
There are factors that increase the likelihood of paresthesia occurring after dental surgery. These include:
- age over 25 years;
- the presence of acute or chronic diseases of internal organs;
- neuralgia;
- history of nerve ending injuries;
- degenerative disorders in intervertebral discs;
- CVS pathologies;
- diabetes;
- pathologies of the endocrine system;
- oncology;
- problems with the gastrointestinal tract;
- deficiency of vitamins and minerals;
- decreased immune defense.
In all these cases, the likelihood of paresthesia increases, so the doctor and patient must exercise special caution and pay due attention to preparatory measures and diagnosis.
How it manifests itself
Paresthesia after tooth extraction should not be confused with the effect provided by the anesthetic. The latter passes without a trace in 4-6 hours. The development of complications is indicated by:
- numbness of part of the face (the patient complains
that a separate area becomes as if plastic, hard); - running “goosebumps” all over the cheek;
- unpleasant burning sensation;
- painful sensations.
These symptoms may last from several days to several months. Sometimes it is possible to get rid of them only after a year. In the latter case, it is customary to talk about a persistent or chronic form of the disease.
How long does it take for a painkiller injection to wear off?
Dentists use several types of anesthesia:
- Applique. An anesthetic in the form of a gel or ointment is applied to the desired area of the gum.
- Conductor. Administered by injection.
- Infiltration. Three-stage anesthesia is usually performed before complex manipulations.
After treatment or tooth extraction, depending on the type of anesthesia, a feeling of numbness remains. If pain relief was carried out correctly, without violating the technology of administering the anesthetic, the numbness goes away after some time.
Experts have identified maximum thresholds for each type of anesthesia:
- after application with gel or ointment, numbness disappears in no more than thirty minutes;
- after conduction anesthesia, the numbing effect lasts up to five to six hours;
- after infiltration anesthesia, numbness disappears within three to four hours.
In order to identify the maximum time threshold, it is also necessary to take into account the individual characteristics of each patient: age, weight, etc.
How to treat
In the first days of numbness, get medical help
not necessarily, since there is a high probability that everything will go away on its own. Only if painful symptoms persist for more than a week should you make an appointment with the doctor who performed the dental surgery.
Since nerve fibers react very sharply to oxygen deficiency, the process of complete recovery takes a long time. The patient may be offered the following treatment options:
- medication;
- physiotherapy;
- surgical.
Medicines for paresthesia after tooth extraction
To restore the functions of the damaged nerve, the patient is prescribed drugs that reduce blood viscosity and stimulate local blood circulation. Good results can be achieved by taking B vitamins.
Physiotherapy
Physiotherapeutic procedures are usually used along with drug therapy. Among the most effective for the described disease:
- Magnetic therapy. It consists of influencing nerve fibers with a magnetic field. Perfectly removes swelling and relieves inflammation.
- Use of electric currents of ultrahigh frequencies. It is designed to relieve muscle tone, increase blood flow to the numb area and block the further spread of inflammatory reactions.
- Introduction of drugs into the area of paresthesia using electrical discharges of minimal intensity. The procedure is designed to quickly restore damaged tissue, relieve pain, and combat the feeling of crawling “goosebumps”.
- Mud therapy. Has a general strengthening effect. Helps increase the body's defenses.
Surgical treatment of paresthesia
Operations for this diagnosis are performed very rarely - only if it is not possible to achieve positive dynamics with the help of medications and physical procedures. The oral and maxillofacial surgeon is responsible for the surgical intervention. After administration of the anesthetic, it restores impaired nerve conduction.
Diagnosis and treatment
To confirm the diagnosis, the doctor collects anamnesis, conducts an examination, and evaluates the reaction of the affected area to various stimuli. One of the most important methods of differential diagnosis is periapical radiograph. Upon completion of diagnostic measures, a treatment regimen is drawn up. This may include:
- injections of drugs that improve blood circulation and reduce blood viscosity;
- taking specialized complexes with B vitamins;
- magnetic and electrotherapy;
- surgical intervention.
The treatment plan is developed individually for each patient. The recovery time for the jaw nerve depends on the degree of damage and treatment methods.
Why paresthesia needs to be treated
Some patients whose symptoms are mild refuse treatment. They get used to living with a numb part of their face and do not want to devote time to long-term treatment measures. You can't do that.
The fact is that in the absence of the necessary therapy, the entire sensitive part of the nerve can be affected. Then the sensitivity of a separate part of the face will be lost completely and forever. Therefore, in order to avoid such a complication, you must definitely consult a dentist if paresthesia does not go away on its own.
Computer anesthesia
In order to eliminate the possibility of developing complications after an injection, modern dentistry uses computer anesthesia.
Advantages of the technique:
- There is no numbness of soft tissues. Computer anesthesia only numbs the area where the anesthetic is injected.
- Computer anesthesia is painless.
- The pressure of the anesthetic is controlled by a computer, so it is administered at the desired speed and in smaller quantities.
- There is no feeling of gum swelling.
- The influence of the human factor is eliminated due to the fact that the computer controls the entire process.
- The tip is shaped like a pen, which is less intimidating for patients who are afraid of injections.
How to avoid paresthesia
To ensure that any tooth extraction occurs without complications,
you need to approach it wisely. Before surgery, the patient must undergo x-rays and an orthopantomogram. These methods will allow the doctor to study the structure of the root system of the tooth and draw up an effective plan for the upcoming treatment. An experienced dental surgeon should be responsible for removal.
It is necessary to understand that fear of possible complications is not a reason to postpone treatment until later. Trust your health to talented specialists, and then everything will be fine. Call our clinic and make an appointment.