Author: Brodsky Sergey Evgenievich Deputy Chief Physician, Candidate of Medical Sciences in the specialties: dentistry and medical microbiology Any person is inclined to believe that if the nerve is removed from the tooth, then it will no longer hurt. However, this opinion is not entirely true. A dead tooth can hurt, and also react to cold and hot, and this is a phenomenon called hypersthesia, increased sensitivity dental unit. These unpleasant sensations require a visit to the dentist, as they may indicate inflammation that has begun in a dead tooth or other dental problems.
Deputy Chief physician Sergey Evgenievich Brodsky
Sign up for a free consultation
+7
Why can a tooth hurt if the nerve has been removed a long time ago?
In medical practice, there are cases when a tooth that was pulpless a month, or even a year ago, suddenly begins to hurt. At first, it may be a barely noticeable discomfort, a reaction to hot or cold. However, soon the unpleasant sensations develop into acute pain, in addition, it often comes to swelling, suppuration and tumors. An unambiguous answer to the question “why does a tooth that has been healed for a long time begin to hurt?” difficult - doctors currently cite several of the most common and obvious reasons:
- Incomplete depulpation
. In other words, if for some reason the nerve was not completely removed, sooner or later it will definitely make itself felt. The process of pulp removal is very complex, requiring maximum precision and care from the doctor. In this case, experience also plays an important role - a young specialist who is thoroughly familiar with the theory is unlikely to be able to cope with this task better than a dentist seasoned by many years of medical practice. If the nerve is not completely removed, over time you will inevitably have to deal with pain and a variety of complications. By the way, if the patient has a pronounced reaction of the tooth to cold or hot, most likely it is the nerve that has not been completely removed. - Poor quality filling after depulpation.
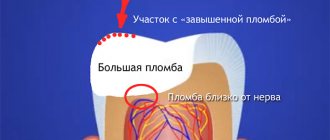
This reason is also quite common in medical practice. For a better understanding of the situation, let us explain: the root canal of a tooth has a thickness of 0.5 to 1 mm, in an expanded form (after processing with special tools) - up to 2 mm. The shape and bends are individual for each individual channel - they can be straight, with bends, with creases. It is not always possible to see this on an x-ray, so the doctor has to work “blindly”, by touch. It is not surprising that in some cases part of the canal remains unfilled. And it is in this part that bacteria accumulate over time, causing inflammation and leading to pain. Also, the filling itself may not lie tightly, allowing access to pathogenic microorganisms. - Increased pressure on the tooth
. The tooth does not just stand in the jaw bone - it is attached to it by numerous threads of connective tissue. If during the filling process the doctor installs a filling that is too high, then the chewing load on this tooth will increase significantly, which, accordingly, will increase the load on the ligaments. Over time, the increased pressure will turn into a constant aching pain, especially evident when pressed. - Infection
. If we assume that the nerve has been completely removed and all the canals have been thoroughly cleaned and securely sealed, there is only one option left - the activity of pathogenic bacteria that entered the root canals and then into the jaw tissue during the treatment of caries or pulpitis. - Insufficient hygiene
. After high-quality depulpation, the patient needs high-quality regular oral hygiene. Even under the most reliable filling, bacteria can accumulate over time if you do not brush your teeth in a timely manner. Some patients believe that dental plaque does not accumulate on the filling material and is not afraid of tartar. In fact, this is not so - bacteria have an equally destructive effect on both tooth enamel and artificial fillings. The infection can get to the root of the tooth and from the gums - this is especially true for people suffering from periodontal diseases. - In fact, one of the neighboring “living” teeth hurts
.
Naturally, it takes time for bacteria to accumulate in an unfilled canal or for an infection to make itself felt. It is likely that a tooth can get sick in a year or after 5 years - it all depends on the degree of neglect of the problem, as well as on the individual characteristics of the body (people with strong immunity tolerate inflammation much easier, so they may not notice alarming manifestations for longer).
In any of the above cases, the tooth will have to be re-treated - the filling will have to be removed, the canals will have to be cleaned and filled again. In addition, a number of additional disinfection measures will have to be carried out.
Diagnosis of the disease
The main diagnostic criterion for pathology is the presence or absence of hyperesthesia in the area of non-carious lesions. Most often, increased sensitivity occurs against the background of wedge-shaped defects in the cervical region. In this case, upon careful examination, an apparently healthy tooth turns out to be affected by erosion; necrosis, enamel chipping, and premature abrasion are also detected.
At the Atlantis Dental clinic, to obtain a complete clinical picture of the causes of hyperesthesia, they are guided by a complete examination algorithm:
- detection of enamel microcracks using optical systems, which allows diagnosing clinical changes in hard tissues at an early stage;
- the reaction to chemical stimuli is determined by probing with a solution of glucose, hydrochloric and citric acid;
- thermal diagnostics (test for hot and cold) is carried out by irrigation using a syringe or an air stream in different directions;
- To identify demineralized areas, clinic doctors use a low-power laser.
As a result of diagnostic measures, the severity, prevalence and localization of hyperesthesia are revealed.
The appointment includes consultation and drawing up a treatment plan with cost determination
sign up for a free consultation
Not ready for an in-person consultation with a doctor? Ask your question by phone
Why can a tooth hurt immediately after nerve removal?
It also happens that immediately after the end of the anesthesia (and the procedure for removing nerves is invariably accompanied by the use of local anesthetics), the patient begins to experience acute pain in the dead tooth. There may be several reasons for this:
- The filling material got from the root of the tooth onto the soft gum tissue . This situation can occur if the material is fed into the root canals under very high pressure. In addition, this often occurs due to incorrect measurement of the channel length. To avoid this problem, it is necessary to take pictures before and after depulpation, and if defects are detected, immediately remove the filling, remove excess paste and reseal the canals.
- Remains of dental instruments in the canal . The needles for widening the canals and removing nerves are very thin. Even though modern instruments are made from high-quality materials, there is a small chance that a small piece of needle will remain in the canal, causing discomfort and pain.
- Damage to the tooth root . During the process of cleaning canals and removing nerves, there is a possibility of drilling through the root of the tooth, resulting in an open cavity leading directly into the jawbone (which, by the way, can also be damaged due to drilling too deep).
- The body's reaction to filling material . Or simply an allergy. Anyone can encounter this, especially if the patient has not previously had to deal with dental intervention. In this case, it is necessary to urgently remove the filling and repeat the procedure using a different material.
All of the above causes of tooth pain after nerve removal are pathological and require urgent medical intervention.
It is important to understand that immediately after treatment, a tooth with a removed nerve may hurt for some time for a number of reasons:
- Depulpation is a process of violating the integrity of nerve tissue, which cannot be completely painless. After the local anesthesia wears off, the patient still feels discomfort and aching pain for some time, which can be relieved with toothache tablets.
- A reaction to cold and hot things in the first couple of days after nerve removal is normal. Due to the violation of the integrity of the tooth tissue, its sensitivity also increases, which goes away after complete healing.
In order for the recovery period to pass quickly and painlessly, it is necessary to strictly follow the recommendations of the attending physician - do not drink or eat for 2 hours after the operation, observe the rules of hygiene, take anti-inflammatory and painkillers.
When should you see a doctor?
Dentists themselves recommend not delaying a visit to the clinic if the slightest alarming symptoms occur:
- Acute throbbing pain in the first hours after depulpation.
- The presence of edema, a swollen cheek or gum, the formation of an abscess under a tooth without a nerve.
- Manifestation of tooth reaction to cold and hot long after dental intervention.
- The pain after the operation does not subside, but on the contrary, it becomes stronger.
- An increase in body temperature (indicates the presence of an inflammatory process).
- Pain when pressing on a tooth or chewing.
If you contact an experienced doctor in a timely manner, any problems can be solved as soon as possible.
Clinical manifestations
The main symptoms of hyperesthesia are short-term acute pain in response to various irritating factors. At the initial stage of the disease, discomfort occurs when touched or exposed to cold air. If you ignore the symptoms, your teeth begin to react to spicy, hot and too chilled foods, including drinks.
The development of the process is characterized by rapidity, and later the unpleasant sensations are accompanied by a sharp pain syndrome and a feeling of soreness under the influence of a chemical, mechanical or temperature stimulus. In some cases, there is increased salivation and difficulty speaking. The attacks are characterized by suddenness and transience, after which the tooth calms down.
Due to pain, in some cases it becomes impossible to carry out hygienic procedures, which leads to the formation of plaque and mineralized deposits, increasing the risk of developing caries. Against the background of increased sensitivity, the growth of gum tissue develops, which, in turn, increases symptoms.
Why does a tooth hurt when pressed?
If the tooth does not bother you until you start chewing or pressing on it, most likely the reason lies in problems with the ligaments that “attach” the tooth to the jawbone, or due to slight swelling that will subside in a few days.
However, there are other reasons:
- A fragment of a dental needle remained in the canal.
- Excess filling material has gone beyond the root of the tooth and landed on the jaw bone.
- The nerve was not completely removed (in this case the tooth hurts even with light tapping).
- During the treatment of caries, an infection got into the root canals.
If you feel a sharp pain when pressing, it hurts to chew and even speak, you must urgently go to the clinic, take an x-ray and repeat the operation to clean and fill the canals, having previously eliminated possible foci of inflammation.
We correct other people's mistakes. Dental retreatment with a 10% discount
Moscow
What is the procedure for devital tooth depulpation?
After the dentist is sure that the anesthesia has worked, the procedure itself is carried out:
- the specialist opens access to the pulp cavity using a drill;
- a special substance is placed into the cavity, which will lead to the death of the nerve;
- the cavity with the medicine is closed with a temporary filling;
- when you return to the dentist’s office, the pulp is removed along with the neurovascular bundle, the doctor cleans the tooth cavity of dead tissue, and performs instrumental and medicinal treatment of the canals;
- after the doctor is convinced that the source of inflammation has been completely eliminated, the canals are sealed;
- The dental crown is restored using filling composite materials.
Interestingly, dentists used to often immediately close a pulpless tooth with a permanent filling, that is, they performed a vital pulpotomy. Today the practice has changed. In almost all cases, a temporary filling is first installed, allowing the specialist to assess the effectiveness of treatment and the stage of healing.
After depulpation, a tooth reaction to hot food may be observed as a result of mechanical intervention. Unpleasant sensations may persist for up to two weeks. To alleviate the patient’s condition, a specialist may prescribe special medications for this period to relieve pain.
Important: if after two weeks the painful symptoms have not disappeared, a repeat x-ray is taken, since prolonged symptoms may be an indicator of a relapse.
What complications may arise?
Pain is one of our body's defense mechanisms. If there is pain, it means one of the systems is not working correctly, and there is a certain pathology. If you do not pay attention to these signals for help in time, you may encounter serious complications:
- Inflammation under the tooth
. At first it will be concentrated in one place. But in the absence of proper treatment, it will spread to nearby tissues, and then, through the bloodstream, throughout the body. - Infection of adjacent teeth
. If the cause of the pain is the proliferation of pathogenic bacteria, it is likely that the infection will spread to the soft tissue of the gums and then spread throughout the entire oral cavity.
If, after removing a nerve, a wisdom tooth hurts, then, contrary to popular belief, it is not necessary to remove it - if it is possible to repeat the treatment, eliminating the source of infection and inflammation, the doctor will definitely do everything in his power to save the tooth.
In the most advanced cases, the doctor usually decides to remove the filled tooth.
Advantages of the Atlantis Dental clinic
What to do if your tooth hurts when it comes into contact with hot or cold food? Of course, visit the Atlantis Dental clinic! We use advanced technologies and medications, and do not prescribe unnecessary manipulations. The key to successful therapy is the high professionalism of doctors, innovative equipment, and an individual approach to each patient!
The cost of treating hyperesthesia for hot and cold, sour and sweet, is flexible and is determined depending on the identified dental problems, the amount of work and the materials used. An integrated approach taking into account all factors guarantees an excellent result, regardless of the age and general condition of the patient’s body!
How to relieve pain?
The process of treating a damaged tooth is very complex and time-consuming. It often takes several visits to the doctor to completely eliminate the cause of the pain. At the same time, in order to somewhat reduce pain, it is quite acceptable to use painkillers, especially considering the fact that most of them also have an anti-inflammatory effect:
- Ibuprofen.
- Aertal.
- Ketanov.
- Nimesil.
- Nise.
- Paracetamol (may help with moderate pain).
In addition, you can numb an open tooth using special lidocaine-based sprays.
Don’t forget: pain relief is just a means to eliminate discomfort, but unfortunately, no pill, even the strongest and highest quality, can cope with the source of the disease.
Classification of hyperesthesia
There are limited and systemic (generalized) processes in which the hard tissues of most teeth are affected. Also distinguished are hyperesthesia associated with loss of dentin as a result of caries and high sensitivity that occurs when dentin is damaged due to heredity, wedge-shaped defect, trauma and toxic damage to the teeth. According to the clinical course and type of reaction, three degrees of the disease are distinguished:
I - heat, cold;
II - salty, sweet, spicy food;
III - all types of stimuli.
Usually the exacerbation phase alternates with remission. At the same time, subsequent attacks when exposed to hot and cold, sour and sweet are characterized by an intensification of the pain reaction and an increase in the time of the attack. At the initial stage of the disease, when using an effective cleanser and correcting the diet, discomfort is significantly reduced or may be completely absent.
Treatment of a dead tooth in dentistry
During the first visit to the dentist, the patient is usually sent for an x-ray, which will help determine the possible causes of pain in the pulpless tooth. Next, the doctor acts based on the current clinical situation:
- The dead tooth is opened and the remaining filling is removed from the canals.
- If there are remnants of nerve endings in the pulp, complete depulpation is performed.
- The root canals are thoroughly disinfected.
- Finishing the channels, cleaning and polishing them.
- Filling of root canals. If there is a one-stage treatment, the doctor uses a filling paste. If there is a need to eliminate the source of infection and inflammation, the dentist will install a temporary filling, which will be replaced with a permanent one in 2-3 weeks.
- Restoring the final shape of the tooth. Restoration work is no less complex a process than canal filling. If the permanent filling turns out to be higher than it should be, an additional chewing load will be placed on the tooth, which may cause discomfort and pain to arise again over time.
It may seem that treating a dead tooth is much easier than depulping a live one. In fact, the opposite is true - finding and eliminating an existing defect is much more difficult than doing all the work on treating a tooth “from scratch.”
What is vital depulpation?
Vital pulpotomy is the amputation of an inflamed nerve under the influence of anesthetic substances. Treatment is carried out in one visit to the dentist. It consists of the following stages:
- anesthesia;
- removal of tooth enamel and dentin with a drill;
- antiseptic treatment of the mouth;
- removal of tissue (fibrous substance, neurovascular bundle) from the pulp cavity and canals;
- filling channels with a composite composition;
- closing the tooth cavity with restoration materials.
Prevention
If for some reason you had to depulpate a tooth, you should not think that now it will never bother you again - without proper preventive measures, the likelihood of pain is very high. To avoid complications, follow simple rules:
- Do not eat or drink for 2 hours after surgery - this will reduce the risk of infection under the filling. Smoking and drinking alcohol are not recommended for at least 24 hours after treatment.
- Take anti-inflammatory pain medications as recommended by your dentist.
- At first, try to reduce the chewing load on the pulpless tooth.
- Regular hygiene. Immediately after treatment, buy a toothpaste to reduce tooth sensitivity. In the future, brush your teeth 2 times a day, do not neglect dental floss and mouth rinses.
- Professional hygiene. Visit your dentist at least once every six months. Make an appointment for a professional plaque and tartar cleaning once a year. To protect your teeth from adverse external influences, go through the procedure of fissure sealing, and to strengthen the enamel - remineralization or fluoridation.
And remember - everything in our body is interconnected. Don’t wait for pain – at the first signs of discomfort after dental treatment, contact your doctor immediately.
Author: Elena Kopylova Dentist-therapist, endodontist, pediatric dentist. Work experience more than 7 years. The information is for reference only. Before treatment, consultation with a doctor is necessary.
How to relieve pain at home?
Immediately after the manipulations, the pain is relieved with NSAIDs (non-steroidal anti-inflammatory drugs), including: Tempalgin, Ketorol, Nise, Nimesil, Paracetamol and others.
In case of slight swelling of the gums, as well as injury to the buccal mucosa, rinsing with herbal decoctions or soda solution (1 teaspoon per glass of warm water) is recommended; washing the affected areas with Miramistin or Chlorhexidine is effective. Antiseptic gels, which are applied several times a day to the inflamed area using the application method, have proven themselves to be excellent.
It is important to understand that pain relief is short-term and does not eliminate the cause of the pathological process. To avoid complications, it is necessary to re-examine, as well as re-treat the canals in compliance with the correct technique and antiseptic requirements.
This cannot be done!
Often, in an effort to relieve pain, patients resort to rather risky methods. Remember what you should never do if inflammation starts:
- taking antibiotics without a doctor’s prescription - at best it will not bring results, at worst it will lead to serious health problems;
- warm the sore spot - elevated temperature favors the proliferation of pathogenic microorganisms, so such “treatment” will only worsen the condition;
- It is undesirable to take a horizontal position so as not to increase blood flow to the diseased tooth.
And finally, you should not let the situation take its course in the hope that the pain will go away on its own. It won't work! In order to get rid of pain, a doctor’s intervention or his recommendations are often necessary.
How are teeth treated under a crown?
An example is the inflammatory process in the apical (deepest) part of the root canal. In case of poor preparation, the canal may not be sealed to its full depth, which leads to the development of infection. To avoid removing the crown, resection of the apical part of the root is performed. The procedure is performed by a dental surgeon and takes from 30 to 60 minutes.
The doctor drills a small hole in the bone tissue. Through it, he cuts off the poorly sealed tip from the root and removes the purulent sac. It should be noted that this method is characterized by minimal trauma. In addition, the procedure is performed under anesthesia, so the patient does not experience pain or discomfort. After removing a section of the root, the remaining part is carefully “sealed” with a special material for further isolation from microbes.
It is important to understand that it is not always possible to do without crown removal. The final decision on the method of treatment is made by the doctor, who may prescribe an X-ray examination to clarify the cause of inflammation. This is due to the fact that additional root canals or suspected cracks require mandatory removal of the structure.