In early childhood, neuropsychiatric disorders such as tics are quite common.
The scientific name is tic hyperkinesis. Parents immediately notice changes in the baby’s behavior. Uncontrolled movements of certain parts of the body or certain muscles in a child cannot but become a cause for concern and questions arise:
- Where did the disease come from?
- Could it have been prevented?
- What to do?
- How to treat?
This list can go on for a long time. One thing is clear - there is certainly cause for concern. And the first thing you need to do is find out as much information as possible about this neurological disorder.
So what are nervous tics in children and what is their danger?
General concept of ticks
This is the most popular pathology of the children's nervous system at an early age. It is simply impossible not to visually notice the manifestation of a tic, although some parents manage to go for weeks or even months without seeing any oddities in their child’s behavior.
Tics are involuntary, stereotypically repetitive, sudden or jerky movements that are the result of spontaneous contraction of individual muscles or groups of muscles.
At the initial stage of development of the disorder, attacks occur quite rarely, and repetitive movements do not cause much concern or problems. The child can even restrain or control them. However, attempts to control the tic cause him:
- internal discomfort;
- feeling of anxiety;
- mental stress.
When control over oneself weakens, tic manifestations occur, and the baby immediately receives obvious relief.
Nervous tics in children are usually detected between the ages of two and fifteen years. In the period of 6–8 years, tic hyperkinesis most often develops, while at 14–15, in approximately half of the cases it disappears spontaneously.
Fun fact: Boys are five times more likely to have the disorder than girls. From a scientific point of view, this is explained by the more stable psyche of female representatives.
What is bruxism and its manifestations
Bruxism is a pathological condition that occurs due to excessive clenching of the jaws.
By the age of 5 years, teeth grinding occurs in almost 50% of children. This occurs involuntarily and is associated with a spasm of the masticatory muscles. Usually the pathology occurs at night, in attacks of 10-15 seconds. Attacks may recur during the daytime. At the same time, daytime teeth grinding causes more concern for parents, since it is more noticeable.
Reference!
Isolated cases of teeth grinding are not dangerous and do not require intervention. If the attacks become chronic, you need the help of a pediatrician.
In addition to grinding teeth, a child may experience the following manifestations of pathology:
- headache;
- daytime drowsiness, lethargy;
- neck pain;
- tearfulness;
- tooth sensitivity is the result of abrasion and damage to the enamel;
- restless sleep with frequent awakenings;
- congestion in the ears.
Dentists identify a triad of symptoms in childhood bruxism (up to 5 years). These are erosive wear of baby teeth, malocclusion and narrowing of the dental arches. Teeth grinding usually goes away on its own when a child reaches puberty. Teeth grinding is a rare occurrence among teenagers and young adults.
Types of nervous tics in children
Each child has his own individuality, and therefore nervous tics that arise for one reason or another are different.
Tic manifestations generally have two types:
- Motor (motor). They are detected by spasms of individual muscles, their groups or movement of limbs and other parts of the body.
- Voice (vocal). They can be recognized in the form of frequently repeated individual sounds, syllables, exclamations, words and even phrases.
Both groups are divided into simple and complex tics. Everything is clear here. A simple form - one short movement or sound, a complex one - several muscle groups are involved, if there are vocal disorders, progress is also observed in them.
Main manifestations
Localization of tic movements most often occurs in the facial or neck muscles. Over time, they can spread from top to bottom. The most common examples of simple childhood motor tics are:
- frowning;
- blinking;
- squinting;
- moving the wings of the nose;
- drawing in air through the nose;
- twitching of the corner of the mouth;
- turning or tilting the head;
- shrug;
- flinching;
- twitching of limbs;
- flexion or extension of fingers;
- snapping fingers.
Vocal tics are manifested by coughing, throat sounds, sniffling, spoken syllables or exclamations. This is a meaningless sound that interferes with speech and gives the impression of stuttering or stuttering. If no measures are taken to eliminate them, the situation will only get worse. Tic movements also progress and reach a new level in the form of:
- grimace;
- head tossing;
- touching various parts of the body with hands;
- contractions of the abdominal muscles or diaphragm;
- squats;
- bouncing.
All of the above nervous tics in children are not all manifestations of the disease. They can be individual and atypical. It all depends on the child’s level of development, his character and temperament, sensitivity to environmental stimuli and a number of other reasons.
Features of the course of the disease
Initially, the child exhibits motor tics, and if the situation worsens, then vocal tics join them. However, there are cases when hyperkinesis begins with sound tics, which significantly complicates diagnosis and delays treatment.
In severe cases, several types of spontaneous movements are observed simultaneously. Sometimes they are accompanied by vocal tics.
Nervous tics in children have their own characteristic features, which make it possible to distinguish them from other pathologies of motor functions. They can be divided into several points:
- Self-control. It should be noted that it works only in the early stages of the disease. This means that the child can control his seizures, but over time it becomes more and more difficult to do so.
- Increased symptoms due to stressful situations. The same tendency is observed at the end of the day due to overwork of the nervous system. The autumn-winter period is the peak of the disease.
- The child's consciousness is not affected in any way. This fact allows us to exclude the development of epilepsy.
- Hyperkinesis does not occur during sleep. This feature is relevant in the presence of vocal tics and confirms the absence of pathologies of the upper respiratory tract.
- A nervous eye tic in a child can at first be mistaken for developing conjunctivitis, but soon everything becomes clear.
The following pattern has been noticed: the earlier the disease appears in a child, the more severe it will be. If appropriate measures are not taken, hyperkinesis develops into a chronic form. In this case, treatment is complicated by the fact that several muscle groups may gradually be involved. Pathological movements move from the head to the lower organs and become more complex, vocal tics are added. Doctors assess them as generalized.
Tic manifestations that arise after the age of ten are almost always classified as transient. This means that they disappear spontaneously and unnoticed, just as they appeared. They are also called transient. They do not require special participation from the medical side.
How long should a baby sleep?
The importance of sleep for babies is difficult to overestimate.
Quality rest, as well as good nutrition, is the key to normal physical and psycho-emotional health of children. During sleep:
- the hormone somatotropin is produced, which plays an important role in the formation of the skeleton;
- Immunity is restored. After falling asleep, T-lymphocytes are activated, destroying viruses and bacteria;
- metabolism in tissues increases;
- cells are renewed;
- the nervous system relaxes.
Babies spend most of their time sleeping during the first three months of life. According to WHO recommendations, the total sleep duration of babies from 0 to 3 months should be 14–17 hours a day. However, these indicators are approximate, because each child is individual. Therefore, if your baby sleeps more or less than the established norm, but still feels good, then there is no need to worry.
Causes
Despite countless years of research into nervous tics in children, doctors have not been able to come to a common point of view regarding the provoking factors. But among many theories, it was found that the most likely are the consequences of traumatic influences. These include:
- Fright.
- Fear.
- Divorce of parents or forced separation from one of them.
- Change of environment.
- First of September. The first days of school are extremely stressful for a child.
- The birth of a second child in the family.
Heredity also plays an important role in the occurrence of tics. Children whose parents experienced hyperkinesis in childhood are much more likely to develop it too.
An unstable situation in the family or immediate environment that a child encounters in kindergarten, school, or in the yard is, of course, the main provoking factor. Children's relationships, communication with peers and adults, can be of a very diverse nature. They often contain conflict situations, and they serve as the starting point of nervous disorders.
Organic brain damage can also cause nervous tics in children. Sometimes they are a consequence of the following events:
- severe maternal pregnancy and difficult childbirth;
- traumatic brain injury;
- a previous neuroinfectious disease.
Separately, it should be mentioned that the reasons for the development of tics may be hidden in a lack of any vitamins, minerals or trace elements.
Since the child’s body is just being formed and is very unstable to external influences, hypovitaminosis can cause disturbances or malfunctions of the nervous system. It has been noticed that the disease progresses in waves. If the child is in a calm, balanced mental state, then tic movements may decrease to minimal manifestations or not be observed at all. At the same time, any stressful situation, fear or anxiety, serves as an impetus for exacerbation of the condition and intensification of tics.
Is the pathology dangerous and what could be the consequences?
Bruxism does not lead to serious health problems, and certainly does not threaten the development and life of the child. Most of all, parents are worried about this phenomenon, and they begin a hospital quest in search of the cause. As a rule, the child grows out of this problem without the participation of a doctor, if it is not chronic. This is due to the development of the chewing apparatus, eliminating problems with the adenoids and normalizing sleep.
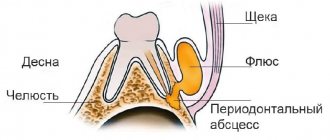
If teeth grinding occurs frequently over several months, then a doctor’s consultation is necessary. Otherwise, bruxism can lead to the following consequences:
- thinning of tooth enamel and increased sensitivity of teeth;
- problems with fillings, they will crumble and crack;
- malocclusion;
- loosening of baby teeth;
- headaches and decreased concentration;
- overload of the maxillofacial joint;
- spasm of the facial muscles.
Excessive tooth wear increases the risk of bruxism during adolescence and young adulthood. Also, severe uncontrolled spasm of the jaws can lead to dislocation of the temporomandibular joint.
Diagnostic procedures
Before starting any treatment, you need to have your child examined by a specialist. After the initial examination, the neurologist refers the patient to undergo electroencephalography. It makes it possible to identify the following indicators:
- local cerebral disorders;
- foci of pathological activity;
- analysis of the state of brain activity.
Repeated studies allow you to monitor the effectiveness of the therapy. A biochemical blood test is mandatory. If the doctor deems it necessary, the child may be sent for an MRI.
Identifying nervous tics in young children, establishing their causes and prescribing adequate treatment is the task of a neurologist. But the direct responsibility of parents is to ensure a comfortable stay for the child at home, in an educational institution or on the street. It is necessary to find out the factors that pose a threat to the baby’s psyche and eliminate them in any way.
Catatrenia as a separate type of breathing disorder during sleep
Catathrenia (sleep groaning) falls into the category of isolated sleep-related symptoms. Attacks of loud sounds, similar to moans or mooing, occur predominantly during REM sleep (80%) mainly in males aged between five and 36 years, with a peak at 19 years of age. The clinical consequences of this condition include deterioration in the quality of sleep and daytime wakefulness, and the social consequences include limitation of social contacts. At the moment, there are two opposing points of view on the nature of catathrenia. According to the first, catathrenia is a form of parasomnia associated with the REM sleep phase; according to the second, it is one of the breathing disorders during sleep. Catathrenia is treated with non-invasive ventilation such as continuous positive air pressure during sleep (CPAP therapy), surgery and oral applicators.
Rice. 1. Polysomnogram during an attack of catathrenia in the REM sleep phase (1 – deep inhalation, 2 – long exhalation, 3 – sound on the sonogram)
Rice. 2. Polysomnogram during an attack of catathrenia in the slow-wave sleep phase (1 – deep inhalation, 2 – long exhalation, 3 – recording sound with a microphone). During these episodes, no changes in activity are observed on the EEG channels
Katatrenia (from the Greek kata
- during and
threnos
- crying for the deceased), or sleep groans (from the English
nocturnal groaning
- night groans), is a rare phenomenon of a change in breathing pattern during sleep. Catathrenia is included in the current third version of the International Classification of Sleep Disorders (ICDS-3) in the section of breathing disorders during sleep along with obstructive sleep apnea syndrome, central sleep apnea, sleep-associated hypoventilation, and snoring [1].
Clinically, catathrenia is manifested by sound phenomena that are similar to groans or mooing, occur periodically during sleep and, despite the fact that they resemble wailing or plaintive crying, are not associated with any pain or expression of emotions on the face.
For the first time, the symptom of night moaning as a result of increased prolonged exhalation in a young man was described by D. Roeck et al. in 1983 [2]. The term “catatrenia” was proposed by R. Vetrugno et al. in 2001. They observed this condition in four patients aged 15 to 25 years, two of them were concerned that moaning would prevent them from living fully in the family with their future spouses [3].
Catathrenia was first included in the ICRS in 2005. At that time, it was positioned as a sleep disorder belonging to the “other parasomnias” group, since it was considered as an unusual form of behavior (vocal phenomenon) during sleep, and changes in breathing patterns were not taken into account [4].
Polysomnographic studies have shown that in most cases (80%) episodes of catathrenia occur during REM sleep. And in the slow-wave sleep phase they develop more often in the superficial (first-second) stages (about 80% of cases) [5].
Attacks of vocalization during catathrenia usually occur two to six hours after falling asleep and last from 2 to 50 seconds, and situations (up to 80% of cases) of group attacks with a duration of a separate cluster from two minutes to an hour are not uncommon. The breathing pattern during an attack has the following distinctive features (Fig. 1): a deep inhalation is followed by a long and labored exhalation, accompanied by a sound described as a grunt or groan. If the attacks form clusters, then an episode of bradypnea is recorded on the sleep polygram, ending with the end of the episode, while blood saturation with hemoglobin usually does not fall below 90%, that is, it does not reach the degree of clinically significant hypoxemia.
On the electroencephalogram (EEG) during an episode of catathrenia, EEG activation is observed directly at the height of inspiration, which continues throughout the entire attack. This feature is typical for attacks that occur during REM sleep. During the slow-wave sleep phase, no EEG activation occurs (Fig. 2) [6]. In addition, during attacks that develop in the REM sleep phase, complete awakening is possible, and its probability directly depends on the duration of the cluster [7]. Electroencephalographically obvious awakening during such episodes occurs in 40–90% of cases, but the patient usually does not remember these episodes the next morning [8].
Sleep moaning typically occurs in young people between the ages of five and 36, with a peak at 19 years of age. The prevalence of catathrenia in the general population is still unknown. It is estimated that this disorder occurs in 0.5% of patients at sleep centers [9]. It is known that men are affected more often than women in a ratio of 3:1. In addition, a family predisposition to the development of this condition has been established: 14.8% of patients have close relatives with the same attacks [4].
The largest number of observations of catathrenia is given in the work of P. Drakatos et al. (2016), who retrospectively studied data from 9000 polysomnographies performed for sleep disorders [6]. Among them, 38 records with obvious signs of catathrenia and another 19 records with suspicion of this condition were found.
The consequences of catathrenia are predominantly of the nature of social maladjustment. For example, young people who go to serve in the army cannot adapt to the team for a long time due to their peculiarities. And women are susceptible to emotional distress because they have difficulty finding a life partner who is not bothered by this condition.
As for daytime symptoms, catathrenia most often manifests itself as increased levels of daytime sleepiness (46%), unrefreshing sleep (88%), and decreased concentration and memory during the day (76%) [10, 11]. However, it should be noted that the only source from which statistics on such complaints were collected is a study by J. Alonso et al., published in 2021 [11]. Using social networks, the researchers recruited people (n = 191) suspected of suffering from catathrenia and asked them to complete a voluntary survey aimed at identifying not only the common complaints mentioned earlier, but also comorbidities. It turned out that 44% of respondents periodically suffered depressive episodes, that is, the sample was not representative, since it included many patients with mental disorders who actively seek help on social media.
Patients themselves rarely notice the manifestations of catathrenia. This condition is more disturbing to those people who, for certain circumstances, sleep next to them (spouses, roommates, travel companions, etc.). Patients themselves more often begin to notice attacks when they become clusters (they account for 6%), during which they wake up.
In the longest longitudinal study of catathrenia, lasting five years, C. Guilleminault et al. did not record changes in the clinical picture over time [12]. However, according to Z. Hao et al., catathrenia can gradually transform into primary snoring or obstructive sleep apnea syndrome [13]. J. Alonso et al. suggested that the long-term consequences of catathrenia could be central or mixed (if a central component is added to the obstructive one) sleep apnea [11, 13].
Due to the insufficiently convincing social and medical consequences of catathrenia, ICRS-3 is considered an isolated sleep-related symptom under the heading “Breathing disorders during sleep.” In other words, this condition is not considered a disease and the criteria for its diagnosis have not yet been agreed upon. However, researchers agree that polysomnography is the gold standard for confirming the presence of this phenomenon.
The differential diagnosis of catathrenia includes central sleep apnea, obstructive sleep apnea, and snoring. Catathrenia differs from central apnea by vocalization (moans or mooing), and from primary snoring, firstly, by the time of sound occurrence (the sound of snoring occurs on inhalation, catathrenia - on exhalation), and secondly, by the characteristics of sound phenomena, which has been proven in study by J. Iriarte et al., where an oscilloscope was used [9]. According to the Yanagihara classification (classification of laryngeal noise, where type 1 means an insignificant amount of noise, and type 4 means almost complete replacement of the laryngeal sound by noise), catathrenia belongs to the second type, and snoring belongs to the fourth. In obstructive sleep apnea, the sound occurs during the recovery of breathing during inhalation and is often described as a “snore.” It is also necessary to distinguish catathrenia from nocturnal attacks of bronchial asthma: with asthma, wheezing, not similar to mooing, is observed when exhaling.
In one of the first studies performed by J. De Roeck et al. (1983), a hypothesis was put forward about the mechanism of development of the moaning sounds characteristic of catathrenia. During the REM sleep phase, a functional narrowing of the glottis occurs (phase I), resulting in a greater expiratory force, then the upper respiratory tract critically narrows (phase II), which is accompanied by a functional and/or organic disruption of the centers that control breathing during sleep ( phase III) [2]. During exhalation, the glottis remains almost completely closed, which is why these peculiar sounds appear [14]. The predisposition to narrowing of the upper respiratory tract may be congenital: Z. Hao et al. found in people with catathrenia a decrease in the angle of the lower jaw along the Frankfruit horizontal line (a line running from the lower edge of the orbit to the upper edge of the external auditory canal, which determines the range of movements in the lower jaw) [13].
Despite the fact that in the current ICRS-3 catathrenia is included in the category of breathing disorders during sleep, debate continues about which category this phenomenon should be classified into: parasomnias or breathing disorders during sleep. Both points of view have followers.
Thus, D. Pevernagie (2017) argues his position by the fact that immediately before an attack of catathrenia, short-term EEG activation is observed in 2/3 of cases. The author also emphasizes that the closure of the glottis is an active motor process that occurs against the background of incomplete awakening of some brain centers, similar to the phenomenon of behavioral disorder in the REM sleep phase [7].
C. Guilleminault et al. (2008) advocate that catathrenia should be classified as a sleep breathing disorder. They substantiate their opinion by the fact that catathrenia is accompanied by bradypnea (before the onset of the episode there are slight pauses in breathing at the height of a deep inspiration) and in most cases can be corrected through non-invasive ventilation with continuous positive air pressure during sleep (CPAP therapy) [12].
A group of Japanese researchers suggested that disruption of monoaminergic transmission involving norepinephrine may play a significant role in the pathogenesis of catathrenia. Scientists discovered catathrenia in a four-year-old boy suffering from Pitt-Hopkins syndrome, a genetic disorder characterized by mental retardation and distinctive facial features: raised palpebral fissures, a beak-shaped nose, prominent ears, a wide mouth with a pronounced Cupid's bow, and intermittent hyperventilation with shortness of breath. In Pitt–Hopkins syndrome, the activity of the TCF4 gene is affected, which directly affects the ASCL1-PHOX-RET pathway, and if it is defective, the development of the noradrenergic system of the brain is disrupted [15].
Catathrenia can be observed in patients with degenerative diseases of the central nervous system (Parkinson's disease, progressive supranuclear palsy, Alzheimer's disease, etc.) along with other sleep disorders [16]. In these cases, the cause of its development may be the disconnection of the activity of cortical-subcortical structures that affect the regulation of breathing, and not a direct lesion of the respiratory center.
Three methods of treating catathrenia have been proposed: CPAP therapy, surgery and the orthodontic method (use of oral applicators). In a review by M. Songu et al. the ineffectiveness of pharmacological treatment of this phenomenon, including antidepressants and clonazepam, has been demonstrated [17].
When using CPAP therapy in automatic mode, a positive effect is achieved in 80% of cases. Thus, after three months of using the device, a significant improvement in condition, defined as a decrease in the number of attacks per night and good health throughout the day, was noted by both patients and those around them. In 20% of cases, the desired effect was not achieved, but the frequency of attacks still decreased by 60% [18].
When using surgical treatment methods, the number of attacks of catathrenia is significantly reduced, but they do not disappear completely. According to S. Guilleminault et al., who are based on the results of a questionnaire survey, surgical intervention (adenoidectomy, tonsillectomy, septoplasty) was successful in only 50% of cases. In addition, the effect of the operation was short-lived: after an average of four months, symptoms of catathrenia returned. The same study surveyed people who used oral applicators that keep the lower jaw in an extended position while sleeping, and 40% of them reported a positive effect of this treatment [12]. With a combination of surgery and an oral applicator, successful treatment results were observed in almost 90% of cases. There have been no prospective studies of the effectiveness of these treatments for catathrenia.
Thus, catathrenia is a rare and still poorly understood sound phenomenon that leads to social stigmatization. Despite effective, albeit inconvenient, treatments, the mechanisms of development of this condition remain unclear.
Treatment
Very often, children who are diagnosed with tic hyperkinesis do not need special therapy. It is absolutely meaningless, and only correction of the patient’s lifestyle helps. However, if the tics become generalized, then treatment cannot be avoided. But which method the doctor chooses depends on the severity of the disease, age and physical characteristics of the child.
An integrated approach to treating tics in children is possible. It includes:
- Activities aimed at properly organizing the child’s daily routine. Protecting him from stress, anxiety and other troubles.
- Drug-free therapy. This complex includes a visit to a psychotherapist, physiotherapeutic procedures, and reflexology.
- Treatment with medications.
At the initial stages of the development of tics in young children, only routine measures are sufficient for visible positive dynamics. Rationally organized time for activities and rest, timely going to bed, proper nutrition, and exercise are the key to a positive outcome from a nervous disorder.
Family psychotherapy is of no small importance. If the situation in the family has given impetus to the development of tics, then you need to try to correct it. Under no circumstances should the child witness quarrels or scandals. It is necessary to create a calm, trusting environment so that the child feels loved and protected. You should not pull back or remind him of his nervous disorder, as this will only aggravate the situation.
Good results in the prevention and treatment of tics are provided by educational games using fine motor skills, art therapy, and relaxation. The most commonly used physiotherapeutic methods to combat this disorder are:
- biofeedback method;
- audiovisual stimulation method;
- acupuncture;
- laser therapy;
- ozokerite applications;
- massage of the cervical-collar area;
- electrosleep.
In cases where drug treatment cannot be avoided, sedatives are first prescribed.
They have a general calming effect, remove nervousness and irritability. If the expected effect is not observed, the doctor prescribes tranquilizers. Their scope of action is the relief of emotional stress, anxiety and fears. With progressive tic hyperkinesis, which is not amenable to gentle treatment, more severe drugs are used. These include antipsychotics and antidepressants. Unfortunately, these medications have a lot of side effects and are used only as a last resort, only as prescribed by a doctor and strictly following the dosage. The main indicator for use is the safety of the child, taking into account the special sensitivity of the not yet formed organism, including the nervous system.
Treatment of tics in children is usually carried out on an outpatient basis, since hospitalization can be an additional source of anxiety. For the same reason, drug therapy is avoided by injection.
Diagnostics
Most children who have this problem during night or daytime sleep do not even know about it. Therefore, most often, parents diagnose the problem.
Some signs:
- Teeth grinding when your baby sleeps;
- Complaints of pain in the face or jaw after waking up in the morning;
- Pain when chewing.
If you experience any of these signs, contact your dentist to examine your mouth for wear and damage. Spray air and water on teeth to test sensitivity.
If damage is found, the dentist may ask your child several questions, such as:
- How do you feel before bed?
- Are you worried about anything at home or at school?
- Are you angry with someone?
- What do you do before bed?
The exam will help the dentist understand whether the cause is anatomical (misaligned teeth) or psychological (stress). Select an effective treatment plan.
Possible consequences
Nervous tics in children of different ages, regardless of the cause, are signals that not everything is all right with the child, his mental state is at the limit of his capabilities, and he needs immediate help. If the irritant is removed in time, the tic manifestations go away spontaneously.
What happens if you leave everything as is? There are several possible scenarios here:
- Epilepsy. Tics may be symptoms of the early stages of this severe neurological disease.
- Severe neuroses, psycho-emotional disorders. Untreated hyperkinesis progresses in the child’s body, causing new manifestations of the tic condition. Lack of qualified help leads to the development of depression and other critical conditions.
- Tourette's syndrome. Although this mental disorder is not a consequence of parental inactivity, its clinical picture necessarily includes both motor and vocal tics.
Even if hyperkinesis disappears on its own after a week without any consequences, it is necessary to go to the doctor and undergo diagnostic procedures. This is a guarantee of the child’s health, and is done with the aim of eliminating the above diseases.
What about worms?
There is a common belief that teeth grinding may be a sign of a parasitic disease. This is due to the fact that preschool children often suffer from helminths. And it is precisely at this age that teeth grinding is typical. Also, this assumption was explained by the fact that when infected with helminths, salivation increases. This provokes clenching of the jaws, which leads to teeth grinding. But according to specialist research, this is just a coincidence. A direct connection between the presence of worms in a child and bruxism has not been identified.
Adaptation in society
Children, as we know, are cruel by nature, so it will be very problematic for a child with obvious manifestations of hyperkinesis to adapt to a new team. But it’s not his fault that the nervous tic happened to him. When communicating with adults, it is very important for him to feel a tolerant attitude. And if at home they constantly focus attention on this topic and reprimand the child, believing that he is doing this on purpose, the situation only gets worse.
Parents should be completely on the side of the child, and he should feel this not only in words. This is what it should look like:
- all conversations about nervous disorders, including tics, should be prohibited, especially in the presence of a baby.
- do not focus on the problem, behave freely and naturally.
- conduct an explanatory conversation with teachers or educators of the team that the child attends, and call on them for assistance.
- choose a suitable leisure activity for your child. Single active sports, such as skiing or swimming, are encouraged.
- provide nutritious and varied nutrition.
During adolescence, a teenager’s body is unpredictable, and also undergoes hormonal changes. If at this stage nervous tics are also detected, then this can generally turn into a personal tragedy. First of all, self-esteem suffers; the child withdraws into himself, does not want to communicate with anyone, and is fixated only on his illness.
The parents’ task is to consider the threat in time and take all measures to eliminate it. Even if the tics do not go away on their own, there is every chance that properly selected therapy or medication will help get rid of them. In any case, you can and should strive to live a full life.
Features of sleep for babies from 0 to 3 months
Some manifestations of restless behavior in children after falling asleep can be explained by the peculiarities of the structure of their sleep.
A baby's sleep, like an adult's, consists of two phases:
- Orthodox or slow-wave sleep. During this period, the brain is inactive, the body is relaxed, breathing is even and calm. It is during slow-wave sleep that a person fully rests and restores physical strength.
- Paradoxical or REM sleep. The paradoxical phase is characterized by an increase in body temperature and pressure, rapid heartbeat, breathing, and rapid movement of the eyeballs under closed eyelids.
During sleep, both phases replace each other: first comes slow sleep, then fast sleep, and so on in a circle. The structure of sleep in infants in the first months of life is unique: its main part is REM sleep, during which the baby may grimace, twitch his arms and legs. This behavior of a baby during sleep is absolutely normal and should not bother parents. As the child grows older, the period of the orthodox phase gradually increases, and the child begins to sleep more peacefully.
Prevention Tips
To prevent a child’s nervous tics from developing into more serious mental disorders over time, all possible measures must be taken to prevent them. You don't need anything supernatural to do this. It will be enough not to forget that the baby sees the behavior of the parents and people around him, draws his own conclusions and evaluates the events taking place due to his level of development.
The psyche of a child at an early age is unstable and vulnerable, so any clarification of the relationship between parents in a raised voice is a stressful situation that can lead to tic manifestations. It is in the family that the child should feel support and understanding. This is his fortress, in which, if necessary, he can hide from all his fears. If there is no such relationship, then the risk of developing tics is quite high.
Children living in a calm, friendly environment are very rarely susceptible to nervous tics. To avoid having to treat the consequences of mental imbalance in a child, it is enough to create comfortable conditions for him. They are as follows:
- avoidance of anxiety and stressful situations;
- healthy, full sleep;
- high-quality and healthy food, a ban on fast food and overly sweet and fried foods;
- compliance with the daily routine, proper organization of rest;
- dosed computer use and TV viewing;
- maximum exposure to fresh air;
- classes in sports sections that match the interests and temperament of the child;
- inadmissibility of overwork.
In rare cases, raising the younger generation does not involve punishment. They are certainly necessary, but within reason. Physical impact is immediately excluded. Only moral methods of influence are acceptable. The child must clearly know what offense he is being punished for and how he should have done the right thing. At the same time, you should assure the child that punishment does not affect his love for him. Only in such a situation will he draw the right conclusions and receive minimal nervous shock.
Even if the appearance of nervous tics in a child could not be avoided, it should be remembered that this is not the worst thing that could happen to him. Modern medicine, combined with parental care and attention, can work wonders.
How to normalize sleep in infants up to one year old
Newborns do not yet have nightmares, severe stress or emotional overload. It is not for nothing that in most cases, sleep disturbances are now considered a physiological norm. And yet, it is entirely possible for parents to create conditions for their child so that he does not wake up at night. What is important to do?
- Establish a clear daily routine. It is advisable that feeding, bathing, periods of sleep and wakefulness take place at the same time. And as experts say, you need to start creating a daily routine literally from the first days of a baby’s life, otherwise it will be more difficult to “implement” a strict routine later.
- Create an optimal microclimate in the room where the child sleeps. It is believed that the room should be 18-22 °C and 40-60% humidity. Many parents speak very highly of air humidifiers, which help create an ideal indoor microclimate - not only maintaining the desired level of humidity, but also purifying the air.
- Provide your child with optimal sleep conditions. It doesn’t hurt to pay attention to the bedding in the crib - it is advisable that it be made from natural fabrics. The child’s clothing is also important – comfortable and soft, providing ideal thermoregulation. In such a child will not be either hot or cold.
- Make sure that the child does not become overtired in the evening hours. Even a baby has busy days. But it is advisable that the child still have “quiet time” before going to bed - no extra guests or active games.
Consult your pediatrician. Let the specialist recommend anti-colic remedies and pain-relieving ointments for the gums that are suitable for the baby. Many doctors recommend swaddling and co-sleeping for sensitive baby sleep.
Both the first and second causes a lot of controversy. There is an opinion that swaddling can inhibit the development of motor functions in a child, cause dysplasia, impair blood circulation in the extremities, or even cause even greater restlessness at night.
Co-sleeping is good for many, but in the future it will be difficult to “move” the baby into a separate room, since he will get used to sleeping with his mother. Weigh the pros and cons
As experienced parents say, this is a difficult time when a child periodically cries in his sleep, you just need to get through it. Everything will pass with age.