Tooth extrusion – what is this procedure? The essence of the method and indications for its use
Tooth extrusion is a separate dental procedure. Nowadays it is performed quite rarely, but in some clinical cases it is precisely this that makes it possible to preserve the root in case of severe destruction of the visible part of the tooth and subsequently, based on it, restore the crown using modern methods of restoration and prosthetics. Extrusion was first introduced to the world in 1973. The author of the technique was Dr. GS Heithersay, who proposed this procedure as an alternative to removing roots with fractures1. Read more about the essence of this method and how such treatment is carried out further in this article.
Treatment of distal bite
Treatment of bite in children
Distal dentition can begin to develop at different stages: from birth, when baby teeth appear, or when changing to a permanent dentition. The sooner the pathology is diagnosed and treatment begins, the less time and less complex technique will have to be used.
Parents can prevent the development and complications of distal occlusion if they follow feeding recommendations, monitor breathing methods, prevent the development of chronic forms of ENT diseases and prevent bad habits from becoming established.
If you still suspect a malocclusion, you can contact an orthodontist for the first time when your first teeth appear, from about three years of age.
At an early age, distal occlusion is corrected using removable techniques: muscle simulators, devices for stimulating the growth of the lower jaw and slowing the growth of the upper jaw, tongue barriers.
In addition to orthodontic appliances, depending on the nature and causes of the bite, the orthodontist may prescribe myogymnastics, refer for the removal of supernumerary teeth or to an ENT specialist, and grind the canines that interfere with normal closure.
Treatment of distal occlusion in adults
From adolescence, with a permanent dentition, straightening teeth and correcting pathologies is possible only with fixed equipment - braces or removable aligners. All types of braces are suitable for the treatment of distal occlusion: external metal and ceramic, internal (lingual)
Often, distal bite is accompanied by displacement of the head of the temporomandibular joint. Such patients additionally use a joint splint to correct the movement and position of the jaws.
If it is impossible to correct the position of the jaws with devices due to their abnormal sizes, one has to resort to maxillofacial surgery: widening the lower jaw or narrowing the upper one.
Completed clinical cases of distal occlusion
What is the essence of the procedure
Tooth extrusion is the procedure of pulling a tooth or remaining root out of the gum in a vertical direction. According to this definition, extrusion allows a slight elevation of the root and creates more suitable conditions for a reliable and durable crown restoration. As part of this procedure, the tooth is usually pulled out by 3-4 mm. But to carry it out, it is important that at least the dentinal rim is preserved. Its thickness must be at least 1 mm, and its height must be at least 2 mm. If there is no such rim, the specialist may try to pull it out from under the gum.
Tooth extrusion is a procedure for pulling out a tooth or remaining root from the gum.
This procedure in some cases allows you to avoid root removal and subsequently restore the crown on it. However, if the root is damaged, its complete extraction followed by replacement with an implant will be the best solution. By the way, extrusion promotes the formation of bone tissue, so the procedure can also be performed as an alternative to artificial expansion of the jawbone for subsequent installation of implants.
Indications for extrusion
As mentioned above, this method is indicated for severe destruction and fracture of the crown of the tooth, as well as for a root fracture, but only if the fracture is in the gum. For reference: according to ICD-10, the root fracture is assigned the number S02.5. Among other indications for the use of this method, dental experts highlight retention. This diagnosis is made when the coronal part does not completely erupt or remains in the gum. This situation is especially typical for wisdom teeth.
“They performed extrusion on me. There was a tooth that was constantly being destroyed. The doctors increased it several times, but it became so dark and chipped all the time. When I once again came to the appointment, they again removed all the composite, they cleaned something there for a long time, and then they said that’s all, I can’t build it up anymore. Instead of removing it, they suggested pulling out the root a little. I agreed. The procedure went well and there was no pain. In the end, they installed a crown, and it’s holding up so far.”
Ira, review on the website www.32top.ru
This procedure can be life-saving if the carious cavity is localized below the gingival level. By removing the affected surface, it is possible to prevent the influence of harmful microorganisms on the mucous membrane and its inflammation.
Traction is also prescribed for retention
Another indication, which was already mentioned above, is insufficient thickness and height of the jaw bone to securely fasten the implant. Extrusion of the tooth root allows you to free up some space between it and the alveolus, which will promote the growth of bone tissue cells and connective epithelium.
Reasons for the formation of distal occlusion
The formation of the jaws is influenced by many factors, some of which determine the bite before the birth of the child or during intrauterine development. Some causes of malocclusion can be controlled and malocclusions can be prevented at an early age. Most often, distal occlusion is the result of a combination of many factors, which we will discuss below.
Genetic causes
Distal occlusion is inherited in approximately 66% of cases. If there is a hereditary predisposition - malocclusion in the parents, the distal bite is formed at an earlier age. Without timely prevention, further exposure to external factors on the bite will only worsen the anomaly.
Features of intrauterine development
The growth of the fetus, including the formation of the jaws, is disrupted by an unfavorable environment and the state of health of the mother. The main harmful factors include: maternal illness, lack of vitamins, high levels of radiation, alcohol consumption.
Features of feeding and early development
Normally, in newborns, the lower jaw is slightly underdeveloped and pushed back in relation to the upper. The growth of the lower jaw occurs due to its intense movement and natural tension during breastfeeding. After about six months, the child develops a correct orthognathic bite. Feeding from the wrong bottle (with a hole for milk that is too wide) in the first months of a baby’s development does not provide the necessary load on the lower jaw. Consequently, it does not grow and remains in a distal relationship with the maxilla.
Sucking on a pacifier, finger, or other objects for too long can aggravate the distal bite and increase the sagittal gap. It is recommended that your child be weaned off the pacifier by the age of 2 years.
With the further development of the baby, you must not forget to introduce moderately solid foods into the diet in a timely manner. Without load and chewing training, the jaws weaken and do not grow.
Childhood diseases
Diseases that affect the malocclusion development can be divided into 2 groups:
- Respiratory tract diseases.
Rhinitis, sinusitis, adenoiditis, deviated septum, other pathologies and diseases that disrupt natural nasal breathing. If a child is forced to breathe frequently or constantly through his mouth, his mouth is slightly open and his lower jaw is lowered. This position of the jaws is fixed and turns into a distal bite. - Diseases that negatively affect the development of the body as a whole.
Rickets, endocrine system disorders, lack of fluoride, calcium and other beneficial substances affect, among other things, the normal growth and formation of the jaws and teething.
Tooth decay or early loss of baby teeth
Loss or poor condition of teeth also negatively affects jaw growth and the formation of a normal bite.
Contraindications to the use of the method
Like any other dental procedure, extrusion has its contraindications. For example, it can only be carried out if the adjacent soft tissues and teeth are in satisfactory condition, since they will act as supports for fixing the traction structure.
The procedure will not be possible if the roots are too short or severely curved, and the condition of the canals and crown does not allow the installation of at least one of the elements of the corrective system: ligatures, a button or a pin with a hook.
Therefore, before prescribing extrusion, the doctor must assess the condition and length of the roots, their location. If the patient is diagnosed with an occlusion pathology in which there is no free space for traction, the procedure will not be possible. And one more thing: the method is indicated exclusively for pulpless teeth, so the nerves will first have to be removed if this has not been done previously.
Consequences of distal occlusion
Improper closure of teeth always means an uneven distribution of load on different teeth - while individual teeth do not participate in the chewing process, others have to process a larger volume of food with greater intensity. This predictably causes teeth to wear out faster. The entire dental-jaw system as a whole is at risk of premature damage:
- periodontal tissue. Gum recession, gum pockets, and inflammation are formed.
- tooth enamel. Under pressure in the gingival area, chips appear on the enamel - wedge-shaped defects. If the teeth are not closed properly, they wear down.
- The roots of the teeth become mobile and gradually weaken, increasing the risk of pulpitis and periodontitis.
- temporomandibular joint.
Distal occlusion can cause disorders and disturbances in the gastrointestinal tract due to ineffective food processing.
Methods of carrying out the procedure
There are two main methods of extrusion. Let's look at each type in a little more detail:
- orthodontic is a more gentle method, which is often combined with correction with a brace system. This method is indicated for impacted teeth, but it requires more time and patience to achieve results. Pulling is carried out by installing an appropriate structure,
- surgical is a rather radical method, which is fraught with serious complications if errors are made on the part of the doctor. But if everything is done correctly, the result can be obtained much faster. The method does not require long-term wearing of the traction system. We will talk further about how extrusion is carried out in this case.
In the meantime, it should be noted that after surgical traction, the patient is given a temporary restoration for the period of tissue and ligament restoration. It allows you to quickly restore aesthetics.
Types of extrusion
There are two types: orthodontic and surgical method:
- An orthodontic design that is more gentle and allows for the simultaneous installation of braces.
- Surgical extrusion involves surgical intervention, but with this method it is not necessary to wear orthodontic devices.
Preparatory stage
Before the procedure, regardless of the chosen method, it is important to undergo a full diagnostic examination to ensure that the patient has no contraindications. You will need to take an X-ray or undergo a computed tomography scan, and a procedure performed by a prof. hygiene to remove plaque and deposits, as well as remove the nerve from the causative tooth if the crown is preserved and depulpation has not been performed previously.
Before the procedure, the patient should undergo a computed tomography scan
How is extrusion performed using the orthodontic method?
In this case, traction is carried out using a special orthodontic system. Its design includes the following components:
- arch or bracket - one of these parts is fixed on elements adjacent to the causative tooth using a composite or special orthodontic rings. If the patient already has braces, the bracket is not installed;
- a screw or a special pin with hooks is attached to the causative tooth, that is, to the remaining crown. If there is not enough hard tissue for this, the pin is fixed in the root canal using dental cement,
- traction – they combine the above-described structural elements and create a force effect.
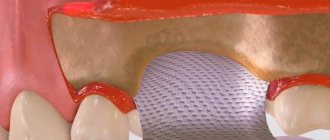
The photo shows the surgical method.
The system is fixed under local anesthesia, since to install it the doctor has to cut the fibers that connect the gum to the root. This manipulation is called fibrotomy. Due to this, the specialist gives the root mobility in order to speed up the pulling process and prevent it from returning to its original position.
Extrusion Concept by Dr. Stefan Neumeier
After extraction of a molar, its resection, replantation and extrusion, a minimally invasive operation is allowed to install an implant in bone tissue, the volume of which is sufficient for this type of procedure. Further procedures with the implant are carried out after complete restoration of the alveoli and gums and have an aesthetically and functionally important clinical purpose. Two years after the installation of the implants, X-rays can be used to detect complete restoration of the bone tissue around them and the absence of signs of rejection.
INTRODUCTION
When a tooth falls out, the physiological load on the periodontium is no longer exerted, which leads to resorption of the alveoli, in most cases causing destruction of the vestibular wall of the tooth. If periodontal or osteolytic processes reach the tooth root, the probability of destruction of the vestibular bone lamella reaches more than 50%. The successful implementation of prosthetics on implants to replace a lost tooth is determined by a number of parameters. An important role here is played not only by complete osseointegration of the implant, but also, above all, by the presence of at least 1 mm of bone wall around the implant. Thanks to the latter, the likelihood of longer-term stability of soft tissues increases, thereby significantly reducing the risk of peri-implantitis [5, 8].
Many authors have proposed their own options for eliminating or minimizing the possibility of resorption after tooth extraction. The Socket Preservation method is a comprehensively studied and widely used method for preventing resorption processes. However, the safety of the bone is not guaranteed at all [1–4]. Thanks to augmentation methods, predictable and durable clinical results are achieved [7].
And yet, these methods often require serious surgical intervention and, accordingly, a high level of professionalism among specialists performing such operations [11, 12, 14]. The use of autologous material as a bone replacement is impossible in most cases, and the larger the defect, the lower the probability of predicting the outcome [11, 13, 14].
The concept of extrusion by Dr. Stefan Neumeier is a fairly gentle and minimally invasive method of surgical intervention, which allows not only to preserve the bone structure of the alveoli, but also to additionally build up hard and soft tissues. This concept represents the optimal option for long-lasting implant prosthetics. The concept involves first carefully removing the unrecoverable tooth, then resecting it, replanting it, and then extruding it [34]. The autologous bone obtained in this way ensures the preservation of the original volume of the alveoli and is durable. This creates ideal conditions for successful implant prosthetics, as well as for ensuring stable bone walls and soft tissue around the implant.
CLINICAL CASE DESCRIPTION
In November 2009, the patient was determined that tooth 36 could not be restored. The clinical picture shows a tooth with a crown without damage, the edges of the crown open to view and the periodontal complex without visible changes (Fig. 1).
Rice. 1
In this case, probing to determine the pathological gum pocket is not required; a wide layer of densely grown gum is observed in the cervical area. An X-ray from 1995 demonstrates incomplete filling of the root canals, resulting in periapical inflammation in the area of the mesial roots (Fig. 2).
Rice. 2
TREATMENT PROCESS
The tooth was carefully removed. In this case, special attention is paid to preserving the bone structure of the alveoli and marginal gums. When removed, the apical granuloma of the mesial root comes out along with the tooth (Fig. 3-4). The periodontium on the root surface remained undamaged. The tooth is placed in a physiological saline solution. Next, the apical side of the alveolus is scraped out with a sharp spoon and a surgical round bur.
Rice. 3
Rice. 4
In this case, the preservation of the integrity of the periodontal alveoli on the cervical girdle is carefully monitored.
At this stage, the alveolus is filled with blood. The extracted tooth is then resected so that the circumferential ligament is preserved around the root surface of the tooth by at least 2 mm. In multi-rooted teeth, the resection zone is located 2 mm below the root furcation. After complete removal of decay from the tooth cavity and root canals, the voids are filled both from the occlusal and apical sides with self-adhesive RelyX cement from 3M ESPE (Fig. 5). Then the tooth divides in the furcation zone, 2 segments arise, consisting of a clinical crown and root with 2 mm of the circular ligament apparatus. During extraoral treatment, the tooth is placed in a saline solution.
Rice. 5
Then, precise replantation of these treated root fragments into their alveoli is carried out.
In this case, due to the formation of a blood clot in the alveoli, the fragments arranged themselves spontaneously. With the help of composite and adhesive technology, these fragments are immovably fixed on adjacent teeth (Fig. 6-7). Re-suturing of periodontal fibers occurs after a few days, when complete immobility of the fragments has become apparent. Tires can also be used as an additional fixation.
Rice. 6
Rice. 7
10 days after replantation, extrusion of completely engrafted fragments can be carried out. At the preparatory stage, fiber pins are attached across the fragments using a fluid composite. A small amount of composite is applied to the ends of the posts to prevent the orthodontic bands from slipping (Fig. 8).
Rice. 8
After this, a small splint, previously prepared in the laboratory, is fixed on the occlusal surfaces of adjacent teeth using a bridge. This bridge is used as a support for orthodontic elastic bands, which are then attached to pins from the vestibular side of the tooth to the lingual side. Due to the accelerated extrusion process (several days), it is necessary to set the maximum tension of the rubber bands. In this case, orthodontic elastic bands with a diameter of 4.2 mm are used, since the patient should replace them twice a day. After 14 days, both fragments are firmly attached to the pins and extruded by 3-4 mm (Fig. 9-10).
Rice. 9
Rice. 10
During the process of accelerated extrusion, periodontal fibers are maximally stressed, and the stability of the fragments is significantly weakened. In the ninth week of the healing period, the fragments are re-fixed on adjacent teeth using a composite (Fig. 11).
Rice. eleven
On the control x-ray, complete regeneration of the bone structure of the alveoli is clearly observed with Lamina Dura still noticeable. The level of the intradental septum and bone in the furcation area can be completely preserved or even improved (Fig. 12). Probing of the gingival pocket showed the absence of any inflammatory processes.
Rice. 12
Before installing the implants, the newly adhered fragments are removed. Beneath them, the clinically restored bone structure of the alveolus and the completely preserved septum are noticeable (Fig. 13).
Rice. 13
The subsequent minimally invasive operation of implant installation is carried out without the use of additional augmentation methods and does not involve further surgical intervention (Fig. 14).
Rice. 14
A two-piece Aesthura classic implant from Nemris with a length of 11.5 mm and a diameter of 4.75 mm is installed. Primary stabilization of the implant in the bone is 35 Newton per centimeter. A Nemris prefabricated abutment with a high-load retention element is then screwed in as a basis for attaching the prosthesis (Fig. 14-15).
Rice. 15
After all procedures, a temporary screw-on crown, individually prepared in the laboratory, is installed in the patient’s oral cavity. Using a flowable composite, the protrusions of the crown, as well as its position, are corrected (Fig. 16-17).
Rice. 16
Rice. 17
When making a temporary crown, the areas of contact with adjacent teeth on the approximal and occlusal sides are noticeably reduced for sufficient primary stabilization of the implant, but this does not imply immediate restoration of the functional load of the crown (Fig. 18).
Rice. 18
The temporary crown was screwed in immediately after installation of the implant without the use of cement, which has a positive effect on the healing of the implant, since cement residues are difficult to remove from the just operated soft tissue. After just a few days, it is noticeable that there are no signs of rejection of the temporary crown (Fig. 19).
Rice. 19
After 3 months, the transfer is screwed in and hydrocolloid impression material is applied (Fig. 20).
Rice. 20
In the laboratory, the anatomical shape of the temporary crown can be repeated when making a permanent crown. After installation of a zirconium oxide crown, there are no signs of rejection; a well-formed alveolar process and a wide zone of keratinized gum are observed (Fig. 21-22).
Rice. 21
Rice. 22
The control x-ray after crown installation shows complete ossification of the bone around the implant (Fig. 23).
Rice. 23
The presence of attached vestibular gum and a wide zone of keratinized gum indicate that there is a sufficient amount of vestibular bone tissue on the implant. Thus, the durability of prostheses installed using implants is guaranteed, and the risk of peri-implantitis is significantly reduced. A control X-ray taken two years later, which shows no differences from the original image, confirms these predictions (Fig. 24).
Rice. 24
CONCLUSION
The clinical picture demonstrates the procedures associated with the installation of an implant to replace tooth 36, which has no visible differences from the neighboring teeth. A harmonious process of gum attachment and a pronounced bone structure are the result of installing an implant in bone tissue, the volume of which is sufficient for this type of procedure. Using extrusion methods, both bone and soft tissues are completely preserved, or more precisely, restored. Consequently, optimal conditions are created for the physiological integrity of the bone corresponding to the tooth being replaced. In order to preserve the structures of hard and soft tissues, it is necessary, first of all, to take into account the durability of prostheses installed using implants.
DISCUSSION
Socket- and Ridge Preservation methods are used to prevent resorption processes after tooth extraction. Numerous studies have shown that when using these methods, the set goal is not achieved, but only partial preservation of the structure of the alveoli is ensured [6]. Various augmentation methods have been proposed to correct alveolar tissue defects. Using these methods, predictable and long-lasting clinical results are achieved. At the same time, the use of augmentation methods often requires serious surgical intervention and, accordingly, a high level of professionalism and extensive experience among specialists performing such operations [11, 12, 14]. In addition, the larger the defect, the lower the probability of predicting the result [11, 13, 14].
The extrusion concept of Dr. Stefan Neumeier completely eliminates the consequences of tooth extraction for tissue, and also creates optimal conditions for further implantation. The concept is based solely on the biological patterns of tissue behavior in the oral cavity. The periodontium is of paramount importance here. Successful growth of the root segment is possible only if the connective tissues on the root segment and alveoli remain intact. When replanting a dental segment, one should not only avoid resorption of the vestibular bone lamella, but also additionally build up hard and soft tissues through extrusion of the segment [10].
The method is minimally invasive, absolutely painless for the patient and is used in practice by the dentist with the least amount of labor. The concept of extrusion, taking into account the results achieved through its use, is the optimal method for minimally invasive prosthetics on implants, guaranteeing high quality aesthetic and functional characteristics of structures and their durability. In practice, the scope of application of the extrusion concept is not limited to the preparation of the alveolar ridge for implantation. By minimizing or even eliminating the risk of resorption in tissues where teeth are missing, a higher level of aesthetic and functional characteristics of bridges is achieved. By extruding each root, deep subgingival defects can be moved into the cervical area to create a more favorable environment for crown placement or therapeutic procedures. In addition, the extrusion technique can be used to treat vertical periodontal pockets and marginal gingival recession for aesthetic reasons, thereby providing patients with treatment with the least amount of surgical intervention. In the future, they will definitely come up with other ways to put this method into practice. The extrusion concept of Dr. Stefan Neumeier is a painless and minimally invasive surgical method that involves gentle procedures for implant prosthetics in the event of tooth loss. The clinical results of the extrusion method prove that they are more than equivalent to the results of the widespread use of augmentation methods.
Source: dentalmagazine.ru
Similar articles:
Modern materials for dental implantation
Cancel Read
Ryan Tak On Tse
Facial analysis in digital planning for total prosthetics
Cancellation
This case illustrates the method of systemic diagnosis, planning and staged treatment for total prosthetics on implants.
Ryan Tak On Tse Read
Barry P. Levin, Brian L. Wilk
Aesthetic rehabilitation of a patient with existing implantation in the anterior upper jaw
Cancellation
Correct diagnosis, treatment planning, and discussion of patient and physician expectations should occur before treatment begins. It is necessary to anticipate the end result and work backwards to ensure that all steps are taken into account.
Barry P. Levin, Brian L. Wilk Read
Vladimir Lesnukhin, Maxim Lesnukhin
Comprehensive total dental rehabilitation
Cancellation
The patient's main complaint: pain behind the canine on the left upper jaw, unsatisfactory dental aesthetics.
Vladimir Lesnukhin, Maxim Lesnukhin Read
Alexey Frolov
Minimally invasive rehabilitation methods at an outpatient dental appointment
Cancellation
In support of doctors who are just beginning to use the concept of Stefan Neumeyer, with a feeling of deep respect for the Master himself and the dental technician who introduced him, Senior S., this publication was created.
Alexey Frolov Read
Edwin A. McDonald III
Fundamentals of occlusion and biomechanics of the jaws: a new look at old concepts
Cancel
A deep understanding of the basics of occlusion and biomechanics of the jaws is one of the most important and necessary components for providing comprehensive patient rehabilitation in dental practice.
Edwin A. McDonald III Read
Igor Malanin, Diana Badreddin
Relationship between body position in space (posture) and occlusion
Cancellation
Prosthetic dentistry today continues to strive for high technology. In modern gnathology, where progress can be comparable in pace, perhaps, with progress in the field of computer technology, the problem of the relationship between posture and occlusion is most acute. Posturology is becoming an integral part of the clinical practice of many dentists.
Igor Malanin, Diana Badreddin Read
Alexey Savinov
Occlusal factors in the development of TMJ dysfunction
Cancellation
To this day, there continues to be a lot of controversy in dental science regarding the effect that the TMJ has on occlusion or, conversely, occlusion on the TMJ.
Alexey Savinov Read
Patrizia Lucchi
Effective aesthetics with semi-direct veneers
Cancellation
About 25% of children suffer dental injuries during the period of temporary occlusion. As a result, they may experience disturbances or cessation of the formation of permanent teeth, manifested in the form of white, yellow-brown discolorations of the enamel or its circular hypoplasia.
Patrizia Lucchi Read
Leon Hermanides
Adaptation of restorations in parafunctional conditions
Cancellation
Even taking into account the fact that doctors are trying as accurately as possible to determine the prognosis of the results of future treatment, some risks or complications cannot be predicted in any way, and they have to be dealt with already at the rehabilitation stage.
Leon Hermanides Read
Paulo Monteiro
Five Meanings of Adhesive Rehabilitation (Part 2)
Cancellation
In dentistry, there is an increasing need to use different parts to achieve the best aesthetics and functionality of the final result. In addition, adhesive systems now make it possible to preserve more natural tooth tissue.
Paulo Monteiro Read
Sergei Shestopalov
Five levels of occlusion in the diagnosis of temporomandibular joint dysfunction
Cancellation
Traditionally, when examining and treating patients with temporomandibular joint dysfunction (TMD), we take into account the relationships of all “elements” of the human craniomandibular system (CMS): dentition, TMJ, masticatory muscles and the central nervous system (CNS).
Sergei Shestopalov Read
- ‹
- 1
- …
How long does treatment last?
After the procedure, the patient will have to visit the orthodontist once a week so that he can monitor the process and adjust the tension of the rods. Usually, in one week, in this way it is possible to extend the root by about 1 mm. Therefore, to stretch it by 3-4 mm, you need to visit the doctor about 3-4 times, and the process itself can take up to a month.
But the treatment does not end there. It will take some time for the root and ligaments to recover. This process usually takes a couple of months. In the meantime, the patient is undergoing a temporary restoration with the removal of the causative element from the bite and its splinting - this is necessary to relieve the chewing load from it.
Signs of distal bite
Any malocclusion is determined primarily by the position of the dentition when closing. But some occlusal anomalies affect the appearance as a whole: they form facial features, facial expressions, symmetry, and affect body position.
Intraoral signs
In the oral cavity, a distal bite is determined by the protruding upper frontal teeth. Normally, with an orthognathic bite, the upper incisors overlap the lower ones by about 1/3. With distal pathology, a distance is formed between the upper and lower incisors - a “saggital gap”.
Sagittal fissure and bite are normal
External signs
Due to the disproportionate protrusion of the maxilla, the distal bite can be identified by a convex or “bird-like” profile. The nose and upper lip protrude forward, the lower lip sinks. The chin is slanted, disproportionately small, sometimes with a fold - a “double chin”. With severe distal occlusion (with a large sagittal fissure), the lips do not close in a relaxed state and the mouth is always slightly open.
Profile before and after treatment of distal occlusion
The distal bite is visually reflected in the posture - the whole body leans forward a little. A patient with distal occlusion is characterized by a pronounced stoop, an elongated neck bent forward, and a protruding abdomen.
Functional signs
In addition to external signs, distal occlusion is accompanied by inconvenience when swallowing, chewing food, and complicates nasal breathing and speech functions.
However, malocclusions usually develop gradually from childhood, so an adult is more likely to adapt and not experience discomfort.
We have described a number of possible signs that can help identify distal occlusion. But the exact diagnosis and treatment methods are determined only by an orthodontist.
Expert recommendations during treatment
During the period of traction, orthodontic experts recommend increasing your oral care. You should brush your teeth not only in the morning and evening, but also every time after eating. It is also recommended to chew on the opposite side and try to eliminate any mechanical factors that could interfere with the healing process. If the structural elements rub the mucous membrane, you should resort to orthodontic wax.
Orthodontic wax will help protect the mucous membrane from damage
Features of the surgical procedure
This method is most often used in cases where the crown part of the tooth is so damaged that it can no longer be restored in the classical way, or if it is necessary to re-prosthetize / replace the old restoration material. This procedure can also be performed if the patient wants to get results faster and without the need for temporary “aesthetic loss”.
This operation is not classified as complex, but it requires appropriate experience and skill from a specialist. For pulling, the doctor uses a special scalpel, elevator and forceps. You could say he creates a dislocation and then does not completely remove the root, after which he fixes it with sutures.
The photo shows the surgical method of the procedure
Recommendations after surgery
As mentioned above, after the operation the tooth is covered with a temporary restoration. About a week after surgery, the sutures are removed. Over the next 2-3 weeks, the patient must adhere to a special diet - it is recommended to eat only soft, warm food, not too cold or hot. You will also need to strengthen your oral hygiene and treat soft tissues using an antiseptic solution, for example, Chlorhexidine, as prescribed by your doctor.
To treat the mucous membrane, you can use Chlorhexidine
1.5-3 months after the operation, the root acquires sufficient stability, which allows endodontic treatment and prosthetics to begin. Some experts insist that it is better to install a permanent prosthesis only 1-2 years after traction in order to prevent the development of complications. It will take quite a long time for the periodontal ligaments to fully recover.
Classification of distal occlusion
Orthodontists use several classifications of distal occlusion.
Clinical forms of distal occlusion according to Khoroshilkina:
- Dentoalveolar form. This form of malocclusion is caused by individual teeth that grow incorrectly or by improper development of the alveolar process, the part of the mouth from which teeth grow.
- Gnathic or skeletal form. An underbite formed as a result of the disproportionate size and position of the jaws in relation to the skull and each other.
- Mixed form - a bite that combines abnormal development of the jaws and abnormal growth of individual teeth.
Angle subclasses:
- I subclass - the upper incisors are directed forward, sometimes slightly upward. This type of distal occlusion is characterized by a sagittal gap.
- II subclass - the anterior teeth grow backward, close to the lower incisors, there is no sagittal fissure.
1 subclass
2 subclass
How impacted elements are pulled out
Extrusion in this case has its own characteristics. It can be carried out in two different ways, but each of them necessarily includes both surgical and orthodontic stages. These are the two methods:
- delayed - first the doctor dissects the gum and exposes the crown. At the next appointment, 2-3 days later, he attaches a special orthodontic button and rods to the impacted element, after which he installs brackets on the adjacent supporting elements (if there are braces, there is no need for brackets),
- one-step – in one visit, the doctor cuts the gum, fixes the orthodontic system and applies sutures.
With the one-step method, the structure is installed immediately.
During rehabilitation, the specialist prescribes antibiotics and antiseptics to the patient. Again, you will have to adhere to a special diet and exclude any traumatic factors. Pulling in this way can last up to 1 year or even longer.
Advantages and disadvantages of the method
The main advantage of the method is the ability to preserve the root and subsequently carry out prosthetics based on it. Here is a list of other obvious advantages of this procedure:
- the ability to avoid expensive treatment, for example, prosthetic bridges or implantation,
- the ability to extend the life of a living tooth for up to 5-10 years and even more,
- the ability to avoid traumatic surgery to build bone tissue before installing implants.
The main thing is that an experienced, highly qualified doctor undertakes the treatment, since much here depends on the quality and accuracy of the manipulations performed. If a specialist makes mistakes, they can result in resorption and a decrease in root stability, and the development of ankylosis.
Among the disadvantages, patients highlight the duration of treatment and the inconvenience associated with it. Partly, it is the fact that pulling takes quite a long time, during which you have to adhere to strict dietary restrictions and be careful not to accidentally damage the system. But the result of such a correction can be considered the preservation of a living root, the opportunity to avoid more expensive and, by the way, no less lengthy implantation.
1Persii L.S. Orthodontics. Diagnosis and treatment of dental anomalies: a guide for doctors, 2004.