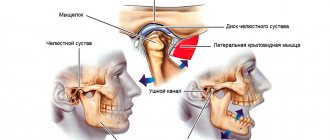
In the modern fast-paced life of every resident of a metropolis, accompanied by the solution of life problems, stress, work pressures, such a problem as TMJ disease (temporomandibular joint) is increasingly emerging. The TMJ is a joint located in front of the ear, consisting of the temporal bone and the lower jaw. The muscles that perform the functions of chewing, swallowing and speech connect the lower jaw to the skull. The TMJ and muscles allow our jaw to move, open and close the mouth, make movements left and right, and extend the lower jaw. The joint and muscles work correctly when the lower jaw moves synchronously in the joint from the right and left. TMJ disorders and muscle dysfunction occur when the lower jaw becomes misaligned during opening and closing of the mouth and other jaw movements. These disorders negatively affect the joints and muscles responsible for the movements of the lower jaw. TMJ disease has many symptoms associated with damage to only the joint or damage to the joint muscles and nerves, which causes pain of varying intensity from a feeling of awkwardness, discomfort in the area of the affected joint to complete shutdown its functions. Another characteristic complaint is joint noise - crunching, clicking, crepitation, and TMJ pathology is accompanied by headaches, ear pain in the absence of infection, jaw locking during chewing, talking, tooth sensitivity in the absence of carious lesions.
Causes of TMJ damage
can be different - infectious, traumatic, most scientists agree that the main cause is a psycho-social factor. That is, during stress, the muscles of the maxillofacial and chewing apparatus become overstrained, which leads to tight clenching of the jaws - bruxism, especially at night. This leads to facial headaches and neck pain, excessive tooth wear and sensitivity.
Other possible causes of TMJ disorders include:
- joint injury,
- decreased bite height due to loss of teeth, especially chewing ones,
- excessive loads when playing athletic sports, malocclusion.
Most people do not notice the pathological changes occurring to them in the initial stages of this disease and consult a doctor when significant changes have already occurred. Therefore, it is very important to regularly visit the dentist in order to identify this problem at the initial stage, when treatment does not yet require surgical intervention. Treatment of TMJ diseases should be comprehensive with the involvement of specialists: dentists, neurologists, osteopaths, psychologists.
Causes of pain in the jaw joint.
Like any other, the mandibular joint is a connection of bones. The lower jaw bone, the head of which is covered with cartilage tissue, is attached to the temporal bone. The articular disc serves as a kind of layer between them. Mouth movements are regulated by the work of the chewing muscles, which are already recognized as the most trained in the body. Together with ligaments, the muscles provide strength to the mandibular joint, while allowing the jaw to move in different directions. The mobility of the jaw is individual for each person and largely depends on the anatomical features of its structure.
Pain in the jaw when chewing or speaking causes significant inconvenience. There are many reasons why it can arise. To prevent complications, it is important to receive timely treatment.
The main causes of pain in the jaw joint:
Fracture
A fracture is diagnosed when complete or partial damage to the jaw bone is detected. A fracture is often the result of a strong mechanical impact on the mandibular joint. Fractures can be open or closed, single or comminuted. The consequences of a fracture can be deformation of the dentition, loosening or loss of teeth at the site of injury, displacement of teeth, numbness of the lower jaw, headache, and dizziness.
Treatment:
- the mandibular joint must be fixed with a tight bandage, and if necessary, the tongue is also fixed;
- ensuring peace;
- urgently seek qualified medical help.
Treatment is aimed at creating conditions for proper bone fusion and restoration of bite.
Osteomyelitis of the jaws
Osteomyelitis is an acute inflammation of the lower jaw bone caused by an infection, usually through a diseased tooth. Symptoms - not only the tooth hurts, but the entire jaw, fever - 38 and above, swollen lymph nodes in the neck, the inflammatory process is confirmed by a blood test.
Treatment:
- removal of infected teeth;
- complete sanitation of the oral cavity with antibacterial drugs;
- in case of complications, an incision is made in the area of the purulent focus and the purulent formations are removed.
- Delayed seeking medical help can lead to an abscess or sepsis.
Temporomandibular joint dysfunction syndrome
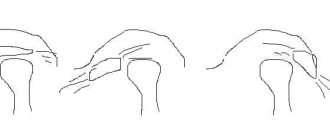
In addition to pain when chewing, dysfunction of the mandibular joint is accompanied by the presence of obvious sounds when moving the jaw, these can be clicks, a “clicking” sound or grinding. Noises of this kind indicate a displacement of the jaw bone in relation to the articular disc. Dysfunction in most cases occurs due to overstrain of the mandibular joint. It can occur as a result of periodic involuntary clenching of the jaw, for example, in sleep. In addition, dysfunction can develop due to stress.
Treatment:
- removal of muscle tone;
- eliminating muscle spasms (taking painkillers, applying cold compresses and ensuring complete rest is often quite enough to eliminate joint dysfunction).
Neuralgia
Various types of neuralgia can also lead to pain. For example, cranial neuralgia, which is a consequence of inflamed nerves of the skull, is often a source of jerking pain. With neuralgia of the glossopharyngeal nerve, the pain is localized in the area of the mandibular joint, and the area of its spread is extensive; the right or left side of the head can hurt completely, starting from the chin up to the temporal part. The pain will increase with palpation.
Treatment:
- prescription of medications;
- local anesthesia.
Arthritis
The most common disease of the jaw joint is arthritis. Depending on the cause, purulent, rheumatoid or traumatic arthritis can be diagnosed. Purulent arthritis. It develops if the maxillofacial joint becomes infected, resulting in purulent formations. The infection can result from diseases such as tonsillitis, influenza, or be the result of hypothermia. Infection in the mandibular joint can also penetrate through the blood, for example, with otitis media. In addition to pain, there is general weakness and increased body temperature.
Treatment:
- taking antibacterial drugs;
- in complicated cases, the purulent focus is opened, and the mandibular joint is treated from the inside with antiseptics;
- ensuring rest of the jaw joint during the treatment period.
Rheumatoid arthritis
It is also a very common disease that is infectious and allergic in nature. The most common culprits for this type of arthritis are streptococcal and staphylococcal infections. The consequences of rheumatoid arthritis are muscle fiber atrophy and tendon damage.
Treatment:
- electrophoresis session;
- physiotherapy;
- restriction of motor activity of the jaw joint during rehabilitation.
Traumatic arthritis.
It is a consequence of hemorrhage in the maxillofacial joint, resulting from strong mechanical impact. It is possible to develop this type of arthritis after dislocation of the lower jaw. The consequence may also be
subsequent deformation of the mandibular joint.
Treatment is similar to that used for other types of arthritis.
Osteoarthritis.
The main factor of occurrence is time. The disease appears due to wear and tear of the mandibular joint. People over 50 years of age are more susceptible. However, it can develop earlier and the cause may be previous diseases of the jaw joint, such as joint dysfunction, arthritis, or even unprofessional dentures. Symptoms in the form of pain appear in the later stages of the disease.
Treatment:
- relieving excess stress and load;
- use of special tires;
- conservative physiotherapy.
How is TMJ dysfunction treated?
While there is no single treatment for TMJ dysfunction, there are different treatments that can significantly reduce your symptoms.
Your dentist will be able to recommend one or more of the following methods:
- Try to relieve muscle spasms and pain by applying hot compresses or taking medications such as muscle relaxants, aspirin or other over-the-counter pain relievers or anti-inflammatory medications.
- Reduce the adverse effects of clenching and grinding by wearing a device sometimes called a bite block or splint. Custom-made to fit your mouth, this appliance covers your upper teeth and prevents them from rubbing against your lower teeth.
- Learn relaxation techniques to control jaw muscle tension. Your dentist may recommend that you attend training or counseling to teach you how to manage stress.
- If your jaw joints are not healthy and other treatments are not helping, jaw joint surgery may be recommended.
Our dental clinic employs a team of specialists involving neurostomatologists, osteopaths, and general orthopedists, which gives good results. Patients with this disease should be very careful, because... This is a chronic disease and, like any chronic disease, can get worse. Therefore, it is necessary to strictly follow the treatment prescribed by the dentist. It is necessary to visit your dentist regularly so that the specialist can monitor your joint and adjust treatment in time to avoid relapses and exacerbations.
Diagnostics
If a person has a sore jaw near the ear and it hurts to open his mouth, he should see a doctor as soon as possible. You should contact a dentist or therapist; if you have an injury, contact a traumatologist or surgeon. If the dentist does not identify a dental cause for the pain, he will refer the patient to an appropriate specialist.
Various tests may be needed for diagnosis:
- X-ray of the jaw.
- MRI.
- Examination by an otolaryngologist using special instruments.
- Blood analysis.
- Bacterial culture of purulent discharge.
Self-help methods for diseases of the temporomandibular joint:
The following self-help methods may provide temporary pain relief:
- Moist Heat: Compressing with a hot pack or bottle wrapped in a warm, damp towel can improve chewing function and reduce pain. Be careful to avoid burns when using high temperature.
- Ice: Ice packs can reduce inflammation, numb pain, and promote healing. Do not place the ice pack directly on your skin. When using, wrap the bag with a clean cloth. Do not use the ice pack for more than 10-15 minutes.
- Diet - Soft Foods: Soft or mixed foods allow the jaw to rest temporarily. Remember to avoid hard, crunchy, and chewy* foods. Do not stretch your mouth when trying to bite off large pieces or the whole fruit.
- Over-the-counter analgesics: Over-the-counter (over-the-counter) analgesics are useful for temporarily reducing pain. Together with your doctor, carefully read the instructions for each medication before using it.
- Lower jaw exercises: Slow, gentle exercises of the lower jaw can help increase jaw mobility. Your doctor or physical therapist can evaluate your condition and suggest appropriate exercises based on your individual needs.
- Relaxation techniques (relaxation techniques): Relaxation can help combat the pain that accompanies TMJ dysfunction. Deep, slow breathing increases relaxation and reduces pain sensitivity.
If you find an error, please select a piece of text and hold LEFT Ctrl and press Enter.
You can send no more than 5 messages in 30 minutes!
Liked? Tell your friends!
What to do if your jaw hurts near your ear when you open your mouth and when you chew
Without a diagnosis, a person cannot choose the correct treatment - which is why jaw diseases cannot be treated on their own. In addition, some of the listed pathologies are useless to treat without hospital conditions.
Although the patient himself is not able to cure such a symptom, sometimes urgent help is required at home, as the pain can be very severe. Following these recommendations can help reduce discomfort:
- You cannot heat the jaw area near the ear : if there is a purulent-inflammatory process, such manipulations will provoke a rapid release of pus and its spread into the bloodstream, which threatens intoxication and general infection. To relieve discomfort, you can apply a cool compress, but only if the pain is not caused by an infection.
- Yawning, chewing, and opening your mouth should be done very carefully.
- To prevent pain from intensifying, you need to temporarily avoid hard and sticky foods, which require increased chewing load. You can't chew gum.
- If it hurts to open your mouth, conversations should be reduced to a minimum.
- If a patient has a jaw injury - he cannot open his mouth, yawn, or speak - you need to call an ambulance and try to provide maximum rest to the damaged joint. Moving the jaw and turning the head can cause bones to shift. For open fractures, the skin around the wound is treated with an antiseptic. If there are bone fragments, they should not be touched.