If a person feels pain in the jaw, radiating to the ear and temple, we may be talking about arthritis of the mandibular joint. The pathology is not just painful, but also dangerous. If not diagnosed in a timely manner, it can lead to severe complications, including paralysis of the facial nerves. Therefore, the first thing to do when such symptoms appear is to consult a specialist. In 10-18% of cases, diagnosis and treatment of TMJ arthritis is the responsibility of dentists and occurs in people from 25 to 45 years old.
Causes of temporomandibular joint arthritis
Arthritis does not show pronounced symptoms immediately; its development can be asymptomatic for a long time or with minor pain. Out of habit, a person reacts to pain by taking painkillers, which only makes the situation worse. Anesthetics relieve symptoms, but do not remove the cause. The disease “takes over” more and more healthy tissue and, as a result, instead of treatment, the patient receives disability. Let's figure out why TMJ arthritis can develop.
- 1. Mechanical injury. Impact, the habit of clenching teeth tightly, and active chewing of hard food can lead to damage to one or more components of the joint. Articular tissues respond to damage with pain and dilation of blood vessels. Simply put, blood enters from the vessels directly into the tissue, causing swelling, inflammation, and, if treatment is delayed, suppuration.
- 2. Infection. The inflammatory process develops as a result of pathogenic microorganisms entering the joint through the blood or through direct and contact routes. The direct route of infection involves inflammation of the TMJ as a result of an open wound (knife or gunshot wound). If microorganisms have penetrated into the cartilage from infected muscle or bone tissues, then the pathology of transmission is called contact. All diseases of the oral cavity (as well as ear, nose and throat) can lead to arthritis of the temporomandibular joint through the hematogenous route, through the blood.
- 3. Systemic inflammation. Some pathologies of an inflammatory nature (herpes, hepatitis, mycoplasmosis, chlamydia, lupus), if not treated in a timely manner, affect connective tissue throughout the body.
Treatment tactics for arthrosis of the mandibular joint
Ideally, starting treatment for TMJ arthrosis is optimal at stages 1 or 2. First of all, it is important to exclude risk factors - excessive mechanical stress, prolonged opening of the mouth, for example at a dentist appointment, etc. Therapy should be continuous and comprehensive - individual orthopedic measures or diet are not enough.
- Diet. To reduce the mechanical load, the patient is recommended to switch to soft foods, and during an exacerbation - to purees, juices, cereals and fermented milk products.
- Daily routine and lifestyle. It is very important to get enough sleep and limit stress, since any stress causes you to reflexively clench your teeth, which can aggravate the situation.
- Dentist consultation. Provoking factors include dental defects, missing teeth, and malocclusion. These problems are easily solved today, and patients with jaw arthrosis are primarily referred to the dentist and orthodontist.
A dentist and an orthopedist always take part in the treatment of jaw arthrosis.
Symptoms of TMJ arthritis
Depending on the cause of the disease and the nature of the inflammation, arthritis manifests itself with the following symptoms:
- sharp pain when moving the jaw. Increases in opening/closing of the mouth, strongly radiates to the temple, back of the head, tongue;
- when you try to open your mouth wider, the jaw moves to the side;
- inability to close teeth tightly;
- hearing loss, dizziness;
- crunching when moving the jaw.
If at least 2 signs are detected, we recommend that you do not wait for the consequences, but contact the dentist. Correct diagnosis ensures the necessary treatment and recovery in a short time. In the later stages, the dentist will not help. And treatment will cost much more.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Features of diagnostic measures for TMJ dysfunction
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
How is arthritis of the lower jaw joint treated?
If pain and stiffness symptoms occur, it is necessary to ensure the TMJ rests. Move your jaw less, take only liquid food, and do not clench your teeth tightly. Visiting the dentist is a must. Only a qualified specialist will be able to tell why the joint is inflamed and prescribe the optimal treatment. Diagnosis consists of blood tests and x-rays. Depending on the situation, we recommend:
- cold compresses;
- drug treatment (broad-spectrum antibiotics, painkillers);
- physiotherapy.
If conservative treatment is ineffective, surgery will be prescribed. Traditional methods of treatment are not only ineffective for arthritis of the temporomandibular joint, they are often dangerous. Decoctions, compresses and ointments according to grandmother's recipes can relieve pain and swelling, but they will not remove the cause of the disease; moreover, some of them can inflame the joint even more. The consequences are impossible to predict, especially with the hematogenous method of infection of the joint. 20% of patients who treated themselves develop joint paralysis.
Symptoms of arthrosis of the jaw joint and diagnosis of the disease
The first signs of the disease usually appear between the ages of 32 and 50 years. If the patient is well informed about the symptoms and treatment of arthrosis of the jaw joint, the disease can be recognized in its infancy.
Symptoms of arthrosis of the jaw - a reminder for self-diagnosis!
You should be alert to the following changes:
- regular clicking in the joint when moving the lower jaw - the crunching seems to “send to the head”;
- limited mobility - for example, when yawning, the mouth does not open as wide as before;
- deterioration of hearing - sounds become muffled, the ears are often blocked, a characteristic noise is heard (as if a seashell was applied to the ear), deafness develops over time;
- blurred vision, which is usually accompanied by pain in the eye from the affected joint;
- pressing and bursting headaches, especially in the temporal, parotid-masticatory region;
- frequent cramps, usually painful;
- nasal congestion;
- dizziness and other problems with the vestibular system;
- abnormalities in the functioning of the salivary glands (usually dry mouth);
- facial asymmetry that has not been observed before - caused by misalignment of the jaw, the formation of bone spurs or swelling of the joint;
- fatigue when chewing food, discomfort when chewing hard and tough foods;
- morning stiffness in the jaw joint;
- decreased facial expression and difficulty swallowing food;
- increasing pain in the joint;
- toothache and tooth wear;
- numbness of the skin or mucous membranes near the affected joint;
- a feeling of “jumps” in the joint - sometimes even noticeable from the outside.
Acute piercing pain with arthrosis of the jaw joint can radiate to the ear, temple or back teeth on the affected side. However, more often patients suffer from a dull, aching pain in the jaw. In old age, pain due to arthrosis of the lower jaw may be absent, giving way to aches (including when the weather changes), heaviness and discomfort in the joint.
If, shortly before the onset of symptoms of jaw arthrosis, you have suffered from arthritis of the jaw joint, an acute infection, an exacerbation of chronic otitis, facial trauma or tooth loss, consult a doctor immediately.
Medical diagnosis of arthrosis of the jaw
When diagnosing arthrosis of the lower jaw, the doctor uses X-rays to determine the type of changes in the joint - sclerotic (replacement of normal bone tissue with abnormal one) or deformational (associated with bone abrasion or the growth of bone growths - osteophytes).
Also, x-ray examination allows us to determine the stage of arthrosis of the facial jaw:
1st - onset of the disease without significant changes in the bone;
2nd - destruction of the articular head with noticeable signs of the recovery process;
3rd - pronounced growth of bone tissue, which prevents movement in the joint;
4th - complete immobility of the jaw due to the fact that the elements of the joint are not consistent with each other.
In addition to x-rays of the jaws, the doctor may prescribe a general blood and urine test, a biochemical blood test, zonography of the affected joint, or diagnostic arthroscopy.
Between the onset of the disease and its final stage, 20-30 years may pass, or maybe 6-12 months. Do not ignore the first symptoms of arthrosis of the jaw joint. Arthrosis of the jaw is completely reversible only at the 1st stage!
Diagnostic methods
Medical diagnosis is carried out using x-ray examination, the results of which make it possible to determine the type and stage of changes occurring.
In addition to radiographic diagnostics, in order to make the most accurate diagnosis, laboratory tests of urine and blood, as well as additional instrumental research methods, can be used.
Self-diagnosis reminder
Changes such as:
- the appearance of crunching/clicking sounds when performing various types of movements;
- decreased jaw mobility, manifested when eating, yawning, etc.;
- hearing impairment;
- decreased visual ability;
- pain of a pressing or bursting type, localized mainly in the temporal or parotid-masticatory region of the head;
- periodic convulsions accompanied by painful sensations;
- dysfunction of the vestibular apparatus;
- increased fatigue when chewing food, difficulty eating solid foods;
- partial loss of facial expression;
- numbness of the skin and mucous membranes in the area of the affected joint.
Bursitis
Vascular angiography is performed to determine the boundaries of the inflammatory process. Contrast arthrography is a diagnostic procedure during which a liquid contrast agent (urotrast, cardiotrast, diodone) is injected into the joint cavity, and then X-rays are taken.
If septic bursitis is suspected, aspiration of synovial fluid is performed for analysis using Gram staining and bacteriological culture.
Which doctors should I contact?
The diagnosis and treatment of bursitis is carried out by a doctor - an orthopedic traumatologist or (for purulent bursitis).
Treatment of bursitis
Therapy for the disease must be comprehensive. It begins with ensuring the rest of the pathological joint, relieving swelling and pain. To do this, it is necessary to reduce or completely eliminate movements in the affected joint and minimize the load. For this purpose, orthoses, bandages and other fixing orthopedic devices are used.
Cold compresses reduce swelling and inflammation. Compression bandaging (squeezing the joint with elastic bands or other devices) reduces pain. Traditionally, drug treatment for bursitis begins with the prescription of non-steroidal anti-inflammatory drugs, which help to quickly relieve inflammation and reduce pain. Chondroprotectors are used to restore joint tissue. Antibiotics are prescribed only for bacterial inflammation of the periarticular bursa.
Modern methods of treating acute bursitis include intra-articular injections with glucocorticosteroids. This allows you to reduce the risk of relapse of the disease and quickly relieve pain, reduce swelling of the synovial membrane of the bursa.
Corticosteroid injections are not recommended for septic bursitis.
In addition, to reduce the severity of pain, swelling and accelerate the regeneration of damaged joint tissues, local remedies are used:
- compresses with dimexide, which have a strong absorbable effect;
- ointments with chondroitin sulfate, glucosamine, and collagen;
- ointments with non-steroidal anti-inflammatory components.
In case of septic bursitis, the inflamed bursa is opened and drained, the pus is pumped out and the joint cavity is washed with antibiotics and antiseptics.
Repeat aspiration may be indicated if swelling, tenderness, and erythema persist. In some cases, the patient may be recommended intravenous antimicrobial therapy. In the subacute period, during the chronic course of the process, physiotherapy sessions are required (ultrasound, microcurrents, electro- and phonophoresis, UHF, dry heat, balneotherapy, paraffin therapy), which can effectively relieve local symptoms of bursitis.
Surgery to excise the bursa is a last resort and is used only in very advanced cases of the disease.
Complications
If inflammation develops near a joint, its mobility may be limited and subsequent muscle atrophy.
In most cases, the duration of the disease is limited to one to two weeks and does not pose a serious danger to human health. However, when an infection occurs, the risk of developing an inflammatory process increases, and serous inflammation quickly turns into purulent inflammation. The spread of the purulent process to surrounding tissues can occur as a phlegmonous inflammation with necrosis of the bursa wall and the formation of subcutaneous and intermuscular phlegmon. In advanced cases, long-term non-healing fistulas form.
The breakthrough of pus into the joint cavity leads to the development of purulent arthritis.
Complications can also develop as a result of untreated bursitis - such complications include scar adhesions, tendon rupture, salt deposition in the cavity of the synovial bursa, arthritis (inflammation of the joint), osteomyelitis (inflammation of the bone), sepsis (blood poisoning), complete immobility of the joint (contracture) .
Prevention of bursitis
Preventive measures are aimed at eliminating the causes and risk factors of bursitis:
- thorough cleansing of wound surfaces, treating the wound with antiseptics for cuts, scratches and abrasions;
- timely treatment of infectious and chronic diseases;
- eliminating the possibility of traumatic joint damage;
- moderate and varied physical activity;
- correct warm-up technique before training;
- fight against excess weight;
- prevention of possible injuries with the help of protective devices for joints - knee pads, bandages and others;
- unloading of joints in the presence of occupational risks (if you have to kneel for a long time, you must not forget about knee pads; when working at a computer, provide comfortable support for the forearm, etc.) and undergoing annual preventive examinations.
Sources:
- Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 3.
- Akhtyamova N.E. Modern approaches to the treatment of bursitis (recommendations for an outpatient surgeon) // RMZh. – 2021. – No. 3. – P. 193–196.
- Bursitis of the elbow joint. Clinical recommendations. All-Russian public organization Association of Traumatologists and Orthopedists of Russia. Moscow. 2021.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
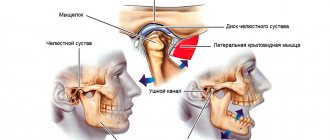
Causes of TMJ damage
can be different - infectious, traumatic, most scientists agree that the main cause is a psycho-social factor. That is, during stress, the muscles of the maxillofacial and chewing apparatus become overstrained, which leads to tight clenching of the jaws - bruxism, especially at night. This leads to facial headaches and neck pain, excessive tooth wear and sensitivity.
Other possible causes of TMJ disorders include:
- joint injury,
- decreased bite height due to loss of teeth, especially chewing ones,
- excessive loads when playing athletic sports, malocclusion.
Most people do not notice the pathological changes occurring to them in the initial stages of this disease and consult a doctor when significant changes have already occurred. Therefore, it is very important to regularly visit the dentist in order to identify this problem at the initial stage, when treatment does not yet require surgical intervention. Treatment of TMJ diseases should be comprehensive with the involvement of specialists: dentists, neurologists, osteopaths, psychologists.
Pathogenesis
The study of the mechanisms of development of pathology allowed us to come to conclusions about their progression associated with a lack of physiological endurance of the joint.
The resulting injuries and the appearance of inflammation lead to improper distribution or excessive load on the tissue, which causes disruption of the synchronization of the joints, causing loss of functionality of the muscular system. The result of the development of such unpleasant processes is a disruption of the nutrition of cartilage tissue, as well as a gradual loss of their elasticity, which inevitably leads to destruction.
Simultaneously with all of the above, serious transformations of bone tissue develop, which provokes the formation of growths that modify the elements of the joint: the head of the lower jaw changes shape, and signs of osteoporosis are visible.
As a result of the uncontrolled course of pathological processes, severe deformation and serious disruption of the tissue structure occur.