Why you can’t install removable and bridge dentures against the background of advanced periodontitis
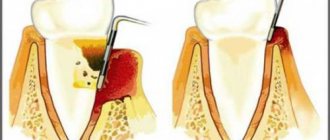
Loss of bone tissue and widening of the sockets during periodontitis create a very ambiguous situation: on the one hand, long-term conservative treatment in the later stages is rarely effective, on the other hand, prosthetics are also difficult, and the problem of missing teeth needs to be solved. However, not every treatment method is suitable.
Why are dental bridges not suitable?
Teeth with periodontitis are weakened and are on the verge of falling out; it is strictly forbidden to use them as support for a denture. The bridge will be movable along with the teeth on which it is attached. The risks are high, even if complex and long-term treatment was carried out before.
Why are removable dentures not suitable?
In fact, after a course of treatment for periodontitis (or closer to the middle of it after acute inflammation has resolved), removable dentures can be installed to solve the problem of partial absence of teeth. But only for a short time, because... When used long-term, they lead to many problems:
- do not stop bone atrophy, but only aggravate this process,
- put increased pressure on the gums and can provoke inflammation, which is extremely undesirable during the course of therapy,
- will require regular correction, since during treatment the damaged tissues are restored, which means the level of the bone with the gum will change - the dentures will no longer fit tightly, will shift, dangle,
- if teeth are partially missing, there is nothing to attach them to - as in the case of bridges, it is better not to use living teeth for support, especially if they are mobile,
- if the teeth are removed scatteredly, then removable dentures will not work at all; the minimum segment is 2-3 missing teeth in a row.
That is, removable dentures can provoke the development of periodontitis and negate all the results of a course of complex treatment. In addition, they are difficult to get used to - more than half of patients are not satisfied with them either in aesthetics or functionality.
Periodontitis: etiology, diagnosis, treatment
Periodontitis is an inflammatory process of the periodontium. The periodontium, in turn, is a complex of tissues (gingiva, periodontium, dental cement, periosteum and alveolar processes) that hold the tooth in the alveolus.
The main symptoms of the inflammatory process are:
- bleeding gums when brushing teeth;
- bad breath;
- teeth are covered with dark plaque;
- gums become swollen;
- the necks of the teeth were exposed;
- tooth mobility appeared.
There are local and general causes of periodontitis.
Local:
Dental plaque, dental plaque and tartar.
Bacterial plaque is a sticky, colorless film that constantly forms on teeth. If plaque is not removed, it will harden and form a rough, porous growth called tartar. Bacteria in tartar produce toxins (poisons) that irritate the gums, causing them to become red, tender, swollen, and bleeding.
As the disease progresses, toxins can lead to periodontal destruction and the formation of pockets that fill with plaque.
The bone that supports the teeth is subject to constant destruction. Consistently removing plaque through brushing, flossing, and professional care can minimize the risk of gum disease. However, if no treatment is given, the affected teeth may become loose and eventually fall out.
Composition and properties of saliva.
Particular importance in the role of metabolism and the formation of periodontal pathologies is given to saliva and its composition. After all, it is the source of enzymes that primarily break down food, a source of microelements, which means that, to a large extent, its properties can influence the formation of dental plaque and its composition.
Periodontal overload.
When the periodontium is overloaded (early tooth loss, malocclusion), a change in trophism occurs - tissue nutrition, which inevitably leads to their change.
Periodontal underload.
The lack of load on the periodontium during chewing provokes the onset of the atrophic process in its tissues.
Are common:
- Deficiency of vitamins C, B1, A, E. Vitamin C is especially distinguished. Since its deficiency significantly affects the condition of collagen fibers, which in turn are part of periodontal tissue.
- Endocrine disorders, especially dysfunction of the reproductive, parathyroid, and thyroid glands. There is also a tendency to periodontitis in people with diabetes.
- Gastrointestinal diseases , gastric and duodenal ulcers, promote the accumulation of histamine in the blood serum, the effect of which on blood vessels often leads to changes in the periodontium.
- Blood pathologies: anemia, leukemia, disorders of the coagulation and fibrinolytic systems, neutropenia, lead to dystrophic changes in the periodontium, hyperplasia of the gingival margin, resorption and osteoporosis of bone tissue.
- Psychosomatic factors Taking medicinal sedatives, neuroleptics, tranquilizers, leading to xerotomy; hyperkinesia (bruxism) of the masticatory muscles under stress often becomes a factor contributing to the development of periodontitis.
LOCAL TREATMENT
- Elimination of factors that injure the periodontium (gum);
- Drug anti-inflammatory therapy;
- Periodontal surgery;
- Orthodontic treatment (if necessary);
- Rational prosthetics and splinting.
GENERAL TREATMENT
- Treatment of concomitant diseases that worsen the condition of the gums.
- General strengthening measures that improve immunity, regeneration, metabolism.
- Balanced diet.
Is it possible to carry out implantation against the background of advanced periodontitis?
Implantation with preservation of living teeth in this form of the disease is extremely rare, but is not excluded. In general, this is assessed at the stage of primary diagnosis - the doctor will understand what results can be achieved with complex treatment, whether it makes sense to spend time and money on therapy, or whether it is better to immediately remove mobile teeth, replacing them with implants, thus stopping the inflammation process once and for all.
It is also important to understand the attitude of the patient himself - it is worth preserving your teeth if you are ready to fight for your natural teeth to the end, if you are ready for the fact that over the next year you will need to visit a periodontist at least once a month and undergo regular treatment, and after installing implants you will have to strengthen hygiene and similar courses will become commonplace for you.
Periodontitis is an infection. Do not follow the lead of those doctors who offer implantation without complex treatment. One-time cleaning, curettage or splinting is not enough; inflammation will progress, which means there is a high risk of it spreading to the tissue around the implant. Rejection in such a situation is guaranteed - you will lose money, time, nerves and will be forced to undergo implantation again, but 100% with the removal of living teeth and most likely with bone grafting, because its own is destroyed.
Thus, implantation for this form of periodontitis while preserving your teeth can be carried out subject to the following parameters:
- if there is something to save - if you only have 3-4 teeth left, there is no point in investing time and money,
- if, based on the diagnostic results, we understand that it will be possible to eliminate the disease during a period of stable remission and the risks of implantation will be minimized due to this,
- if you are ready for long-term treatment and follow all your doctor’s recommendations in the field of lifestyle changes, nutrition, and oral hygiene.
Why do we most often recommend removing teeth with periodontitis?
Our natural teeth are a hotbed of inflammatory processes. They have a porous structure, so it is on them that all microbes, which have a destructive effect on periodontal tissue, first settle. If implants with an active surface are placed next to such teeth, even the most resistant ones, which contain chemical elements that promote the healing of bone cells (such as SLActive® from Straumann and TiUnit® or TiUltra® from Nobel Biocare), they will still are unable to cope with a massive attack from all sides and bone tissue atrophy. That is, by preserving our natural teeth, we risk losing all the results of implantation.
So if there are only a few teeth left, they are destroyed and affected by diseases, then there is no point in preserving them - it is much easier to carry out removal with simultaneous replacement with implants, after which it will be enough to carry out regular oral hygiene (on your own and with a dental hygienist) and actually forget about dental problems forever. After all, if there are no teeth, there is no inflammation.
We categorically do not recommend implantation on one jaw if there are foci of generalized periodontitis of a severe and acute stage on the second - even though there is no direct contact, it is still dangerous. Our body is a single whole, let alone the oral cavity. Pathogenic microorganisms will circulate along with saliva, so inflammation of the tissues around installed implants is only a matter of time. It is impossible to talk about any lifelong service in such a situation.
Periodontal diseases and measures for their prevention
Periodontal diseases, as well as dental caries, have become very widespread. According to WHO, about 95% of the world's adult population and 80% of children have some form of periodontal disease.
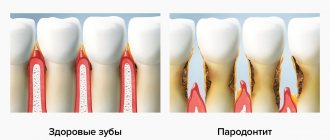
What is periodontium? The periodontium is a complex of tissues that surround the tooth and ensure its fixation in the jaw bones. This complex includes the gum, periodontal ligament connecting the tooth root to the bone socket, bone tissue of the alveolar processes and cementum of the tooth root. With various periodontal diseases, the pathological process may involve any part of the periodontal complex or the entire periodontium as a whole. The nature of the pathological process can also be different: dystrophic, inflammatory or tumor.
Among all periodontal diseases, 90-95% are inflammatory, such as gingivitis and periodontitis. Therefore, we will focus on them in more detail.
Gingivitis is an inflammatory process in the tissues of the gingival margin, in which only the superficial tissues of the gums are affected.
Periodontitis is an inflammatory process that involves all periodontal structures. It is characterized by the destruction of the periodontal junction and the progressive destruction of the alveolar processes of the jaw bones.
In fact, gingivitis and periodontitis are two interrelated forms of the disease, since the inflammatory process occurs first in the gum tissue, and gradually the underlying periodontal structures are involved: the periodontal ligament and alveolar bone.
Currently, the main local pathogenetic factors underlying inflammatory periodontal diseases have been established. This is the accumulation of dental plaque (microbial factor), disruption of the structure of the vestibule of the oral cavity, dental anomalies and supracontacts.
The inflammatory process in the gum tissue initially occurs due to massive microbial accumulations and the enzymes and toxins they secrete. While the inflammation is limited only to the gums, and the underlying tissues are not affected, we are dealing with gingivitis, which occurs with periods of exacerbation and remission, with varying degrees of activity in different patients.
| Figure 1. Chronic gingivitis. |
The difference in the nature of the course of gingivitis is determined by the state of the general protective mechanisms in patients. That is why, with the absolute recognition of the microbial factor as a causative factor, the “interest” of the entire organism in the development and course of this seemingly purely local process was never questioned.
What complaints do patients have with gingivitis?
Most often these are complaints of bleeding gums.
Bleeding gums during brushing are noted by almost all patients with gingivitis. There may also be complaints of pain and bleeding gums while eating. The general condition, with rare exceptions, is not disturbed.
When examining patients, as a rule, a large amount of soft dental plaque is determined, especially in the area of the necks of the teeth. The gingival margin is usually hyperemic, swollen, and the gums bleed easily upon probing.
Since with gingivitis only superficial tissues are inflamed, easily accessible for viewing and targeted therapeutic interventions, the treatment of this disease is very effective.
The main method of treatment and prevention of gingivitis is the removal of microbial accumulations, that is, hygienic measures.
Hygiene products - pastes and toothbrushes - are the main weapon against inflammatory periodontal diseases. Moreover, they act equally effectively against inflammation in the periodontium and against caries, since the microbial factor is the main factor in both cases.
However, despite the presence of such an effective and affordable preventive and therapeutic agent, the problem of inflammatory periodontal diseases remains very relevant. Already in childhood, in 30-80% of cases, the initial stage of the disease is diagnosed in the form of superficial inflammation - gingivitis, the course of which is characterized by alternating periods of intense inflammatory reaction and relatively favorable periodontal condition. With age, the intensity and prevalence of the inflammatory reaction in the periodontium increases: in adolescents with gingivitis, destructive changes in the periodontium are observed in 2-6% of cases. Later, the frequency of superficial inflammatory changes, manifested in the form of gingivitis, decreases, and the prevalence of deeper destructive phenomena in the periodontium of varying degrees of severity increases significantly.
| Figure 2. Chronic periodontitis. |
The problem of adequate hygienic oral care and instilling the necessary hygiene skills in children is extremely difficult. Today, the domestic market offers hygiene products (pastes and brushes) of fairly high quality. The question is different: in order to achieve the necessary cleaning of the teeth and gums, it is necessary to brush at least 20 times on one surface of the tooth, the total time of brushing the teeth - from the outside and inside - should be at least three minutes, otherwise the microbial plaque will persist. In addition, it is necessary to treat the interdental spaces with floss (dental floss). It is necessary to teach children this from a very early age in order to develop in them the need for such brushing of their teeth at least twice a day.
Until the child is consistently motivated for this type of care, it is difficult to expect tangible results in relation to the condition of the gums and teeth. It should be remembered that the quality of teeth cleaning largely depends on individual manual skills. Many children, no matter how hard they want, simply cannot brush their teeth well, even if they try very hard. The above directly applies to children with general developmental disorders.
What could be the way out of this situation? The doctor should regularly carry out appropriate treatment or prescribe drugs that effectively suppress the activity of microorganisms and slow down the formation of microbial accumulations. For these purposes, today the most effective drug is chlorhexidine bigluconate, which sharply inhibits the vital activity of all microbial accumulations that cause damage to periodontal tissue and hard tooth tissue. In addition, it actively suppresses herpes viruses and fungi, and has a weak analgesic effect. The disadvantage of this remedy is its persistent bitter taste, which limits the use of this drug, especially in children. The drug Corsodil, which recently appeared on our market, does not have this disadvantage. Because of this, it has become widespread in many countries around the world. Staining of the surfaces of the tongue and fillings - a property of chlorhexidine - is a temporary phenomenon that passes fairly quickly. But the effect of using chlorhexidine both as a therapeutic and as a prophylactic agent is very high and stable. Patients use the drug independently, the course of treatment is 5-7 days.
As soon as inflammation overcomes the main barrier - the periodontal junction - it rushes into the underlying tissue - the periodontium and alveolar bone. Being a logical continuation of gingivitis, this form takes on completely new features. Firstly, a periodontal pocket is formed, in which microbial accumulations are securely hidden and are not removed during tooth brushing. Secondly, in the depths of periodontal pockets, the most aggressive microbial species actively multiply - anaerobes, spirochetes, the damaging potential of which is extremely high. Thirdly, from the pockets the microorganisms themselves, and their enzymes and toxins, easily penetrate into the underlying structures, dissolving them. As a result, the stability of the teeth decreases, they become mobile, and the mechanical load on the teeth during chewing turns out to be traumatic. As a result of this injury, the destruction of the supporting apparatus of the tooth occurs especially quickly, which, in turn, further contributes to the spread of microbial accumulations. Periodontitis forms.
| Figure 3. Rapidly progressive periodontitis. |
The complaints that patients usually make are mobility of teeth, bleeding gums, bad breath, fan-shaped discrepancy of the upper front teeth, exposure of the necks of the teeth.
On examination, hyperemia of the gingival margin is noted, often with a cyanotic tint; the gum does not fit tightly to the neck of the teeth.
When probing, periodontal pockets of varying depths are determined, depending on the severity of the process. There are supra- and subgingival dental deposits. When the process is severe, purulent discharge from periodontal pockets and significant tooth mobility may occur. Radiologically, with periodontitis, a decrease in the height of the alveolar process is noted due to resorption of bone tissue of the interalveolar septa.
Treatment of periodontitis is aimed primarily at removing microbial accumulations, tartar and granulations from periodontal pockets. If the periodontal pockets are deep enough, their thorough treatment is only possible through surgery. And after the operation, the main task is to prevent active penetration of microbial masses deeper into the tissue. This is more difficult to achieve, but again the main method of prevention in this case is high-quality controlled oral hygiene, the prescription of effective antimicrobial rinses, among which Corsodil is today recognized as the most effective.
There are a number of forms of inflammatory periodontal diseases that are characterized by increased aggressiveness. Their main difference is in the presence of specific microorganisms and their combinations.
Prepubertal periodontitis. The process occurs in childhood and involves the teeth of the permanent and even primary dentition. The early development and aggressive course is due to the fact that such patients have defects in general defense - monocytes and polymorphonuclear leukocytes. In such cases, the tactics of specialists boil down to more thorough antimicrobial control. But the result can only be achieved through the efforts of general specialists - if it is possible to eliminate blood cell defects with the help of targeted medication.
Focal juvenile periodontitis. With this form of periodontitis, selective damage to the supporting apparatus of the first permanent teeth occurs. The disease is caused by the species Actinobacillus Actinomycetes comitans. In most cases, it occurs in children whose parents are carriers of the microorganism. The process occurs with minimal inflammatory reaction. Its rapid spread is due to the fact that this type of microorganism has the ability to suppress the chemotaxis of leukocytes, and antibodies do not have time to form under such conditions. Therefore, subsequent permanent teeth are rarely damaged, since specific antibodies later have time to form and exert their protective effect. Treatment includes active antibiotic therapy - for at least 3 weeks - in combination with local interventions. The duration and need for general antibiotic therapy are due to the fact that microorganisms not only inhabit the periodontal sulcus, and subsequently the periodontal pocket, but also penetrate deep into the tissues and bone structures, where they persist quite persistently.
Rapidly progressive periodontitis, as well as periodontitis resistant to therapeutic interventions , is caused by a specific microflora: Porphyromonas gingivalis (formerly bacterioids), Actinobacillus Actinomycetes comitans and Prevotella intermedia. Moreover, it is usually their combination that occurs. In this case, these microorganisms exhibit a sharply positive synergistic mutual influence, and the microbial composition not only causes a sharp destructive effect on tissues, but also suppresses the effect of protective cells. In addition, invasion of these microorganisms deep into tissues is characteristic.
| Figure 4. Periodontal disease. |
Medical tactics consist of careful mechanical treatment of periodontal pockets and intensive antimicrobial therapy. Local application of metronidazole or tetracycline orally is effective. It is advisable to perform patch surgeries no earlier than 3-4 weeks after the start of antimicrobial therapy, otherwise, if the viability of the listed microorganisms remains, surgical treatment will be ineffective. Corsodil has a good effect after surgical treatment. Considering the relative local unresponsiveness, the most reliable criterion for the effectiveness of treatment is microbiological analysis of the contents of periodontal pockets and tissue biopsies. It follows from this that in some cases it is advisable to treat such patients only in specialized institutions that have the necessary facilities. And of course, no treatment can be effective, especially when it comes to long-term prognosis, if there is no proper oral care.
One of the diseases that is based on the degenerative process is periodontal disease. Periodontal disease is an atrophic-dystrophic process in periodontal tissues. This disease has rather sparse symptoms. What brings patients to the doctor?
This is mainly a cosmetic defect, expressed in the fact that the roots of the teeth are exposed and their clinical crown is enlarged. Patients complain that “the gums sag and the teeth become long,” this especially bothers them in the frontal region. In some cases, patients are bothered by itching in the gums, as well as pain from the exposed necks of the teeth.
During examination, most often, uniformity of atrophic manifestations is observed in the area of all teeth and the involvement of dental tissues directly in the process - this is expressed in the presence of so-called wedge-shaped defects. This pathology is characterized by a slow course and relative asymptomaticity.
The cause of this pathology is unclear; it is considered either as a premature development of involutional processes, or as a manifestation of general disorders in the periodontium, that is, a syndrome or symptom of general disorders. However, a very specific and clearly defined clinic makes it possible to distinguish this form of the disease.
There is no adequate treatment for periodontal disease because the cause of the disease has not been established. The doctor provides only symptomatic treatment - eliminates increased tooth sensitivity, prescribes massage or automassage of the gums to correct trophic disorders, and also fills wedge-shaped defects. In an effort to meet the wishes of patients, some surgeons perform vestibuloplasty operations. However, this should not be done, since the effect of such interventions is very short-lived.
What is actually effective is the use of products that eliminate the pain sensitivity of the exposed cheeks of the teeth. To do this, use fluoride varnish, fluogel, and baking soda powder. Currently, Sensodyne paste has appeared on the market, which successfully relieves increased sensitivity of teeth, and the patient can use it independently. The doctor should warn patients with this disease that they should not use a hard brush or make horizontal movements so as not to increase the depth of the wedge-shaped defects.
Tumor and tumor-like lesions are also among the diseases that are difficult to predict, since they develop only in individuals with a predisposition to this process. And the impetus for the beginning of the development of the process can be hormonal changes, in particular the accumulation of somatotropic hormone during puberty or pregnancy, the presence of a chronic traumatic factor, and previous inflammation. However, all of these are just additional risk factors that provoke the development of such lesions in individuals predisposed to this process.
Treatment and prevention measures consist of eliminating trauma, inflammation and, if necessary, surgical removal of overgrown tissue (for gingival fibromatosis, hypertrophic gingivitis, epulis, interradicular granuloma). Currently, another rather serious factor has emerged that provokes the development of this kind of pathology: the use of anabolic steroids by young people when engaging in bodybuilding and professional strength sports. The doctor’s capabilities here are modest: clarification and advice.
What really leads to a positive result in such cases? Maximum thorough oral hygiene, the use of effective antiseptic and antibacterial rinses by the patients themselves after an active treatment course.