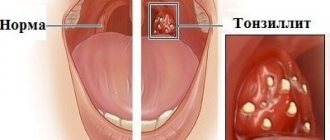
Sore throat (acute tonsillitis) is a disease that affects the palatine tonsils. There are many varieties of the disease. In the vast majority of cases, its causative agent is staphylococcus and streptococcus bacteria. But in otorhinolaryngology, there is another type of disease, the cause of which is not a bacterium, but a virus. Viral sore throat in children is most often caused by the herpes virus. Children of preschool and primary school age are at risk. For infants, this disease is difficult and extremely dangerous. As with bacterial tonsillitis, the viral form of the disease causes inflammation of the palatine tonsils (glands), but the symptoms and treatment of viral tonsillitis are somewhat different from the usual manifestations of tonsillitis. So how does the disease manifest itself? Let's figure it out.
Causes and routes of infection
The very name of the disease already makes it clear that the source of infection is a variety of viruses. These can be herpes viruses, influenza, Coxsackie viruses, ECHO viruses, adenoviruses, enteroviruses and others. Therefore, the disease is conventionally divided into adenoviral, influenza and herpetic.
The disease is highly contagious: you can become infected during a conversation, by sneezing, through dishes, toys, and food. Viruses that enter the body reach the surface of the tonsils and settle there. From the moment of infection, the patient remains a source of infection for another 30 days. Many factors increase the likelihood of developing the disease:
- cold season;
- improper and unbalanced diet;
- lack of personal hygiene;
- hypothermia (for example, caught in the rain, eaten cold ice cream);
- smoking in front of a child;
- bad ecology;
- climate change;
- weak immunity;
- the presence of a chronic source of infection in the body (for example, chronic tonsillitis);
- carious teeth;
- allergic reactions;
- tuberculosis, diabetes and other diseases;
- stressful situations.
Sore throats caused by influenza viruses or adenoviruses usually occur during the cold season, especially during outbreaks of epidemics, when the body's defenses weaken. Herpetic sore throats are more common in the summer. In order to understand in time that we are dealing with viral tonsillitis, it is necessary to be able to distinguish the main symptoms of the disease in a child.
How to treat a sore throat in a child?
An infection of a child's tonsils is called tonsillitis. The tonsils are glands in the back of the throat. Tonsils are part of the immune system and help fight germs in the mouth. Tonsils often become infected with viruses or bacteria. Bacterial tonsillitis is sometimes called tonsillitis (including streptococcal tonsillitis). Tonsillitis is common in children of all ages and often occurs with colds, runny nose and cough. Even if tonsillitis is caused by bacteria (tonsillitis), it is usually an infection that the child can recover from without antibiotics. Antibiotics do not improve tonsillitis symptoms, and most children have a sore throat that persists for three to four days, even if they are treated with antibiotics. Waiting to see if children get better without antibiotics is helpful because it increases immunity to infection and reduces the chance that your child will get tonsillitis again from this type of infection. If your child has recurring infections, it may be helpful to change the toothbrush after each infection to prevent the tonsils from becoming infected again.
Antibiotics are used for infection of the tonsils with Beta-hemolytic streptococcus group A (GABHS). However, the use of antibiotics in this case is aimed at preventing severe complications, such as rheumatic damage to the heart or joints.
Signs and symptoms of tonsillitis (tonsillitis)
If your child develops tonsillitis, it may present with the following symptoms:
- A sore throat
- Difficulty swallowing
- Painful lymph nodes (glands under the jaw)
- Ear pain (middle ear infection must be ruled out)
- Fever
- Bad breath
- Loss of appetite
- Lethargy and general malaise.
- Older children may also complain of headaches or stomach pain.
When to see a doctor?
If you think your child has developed tonsillitis for the first time, take him to a pediatrician, general practitioner, or ENT doctor. If your child has had tonsillitis before and it usually improves with home care, you don't always need to see a doctor.
Because tonsillitis is often caused by a virus, your doctor may not prescribe antibiotics because they will not help your child.
But some children may need antibiotics, including:
- those who have previously suffered from rheumatic heart disease,
- children with severe tonsillitis, especially if there is a rash (called scarlet fever)
- children who have complications, such as an abscess behind the tonsil or in the lymph nodes of the neck.
If swallowing is difficult, some children are given prednisolone (an anti-inflammatory corticosteroid drug) with or instead of antibiotics. Prednisolone reduces swelling of the tonsils.
If your child feels very unwell, is drooling and has difficulty breathing, call an ambulance immediately. This could mean dangerous inflammation of the epiglottis.
Caring for a child with a sore throat at home
Most children with tonsillitis can be treated at home after visiting a doctor (if necessary).
You can care for your child in the following ways:
- Make sure he gets plenty of rest.
- Give him a pain reliever, such as paracetamol or ibuprofen.
- Give your child more fluids to drink. This will prevent dehydration and make your throat less dry and sore. Ice cream is a good option as it provides extra fluid while also soothing inflammation and reducing sore throats.
- There are no restrictions on what a child can eat or drink. However, children may prefer softer foods if they have a sore throat.
- The child should stay at home until his fever has passed and he can swallow again without pain or difficulty. This usually takes three to four days.
If your child is prescribed antibiotics, give them to your child as directed and make sure the full course of antibiotics is completed.
You should call your doctor if your child has tonsillitis or sore throat and:
- Difficulty breathing with increased snoring during sleep
- Difficulty swallowing and signs of dehydration
- The child has difficulty opening his mouth
- You are worried for any other reason.
How to prevent tonsillitis from spreading to other children in the family?
Maintaining good hygiene reduces the chance of transmitting infection to others. Good hygiene includes: regularly washing your hands thoroughly, not sharing cups or cutlery, not allowing toothbrushes to touch, encouraging children to cough or sneeze into their elbow and using disposable tissues instead of handkerchiefs. Teach your child to throw tissues in the trash as soon as they are used and to wash their hands afterwards.
Key Points to Remember
Tonsillitis is an infection of the tonsils that can be caused by viruses or bacteria.
Bacterial tonsillitis is called tonsillitis.
The most dangerous form of sore throat is GABHS sore throat. It requires the use of antibiotics.
Most children recover with rest at home, pain relief, and plenty of fluids.
Many children do not need antibiotic treatment. Antibiotics do not treat viruses.
If antibiotics are prescribed, be sure to complete the course of antibiotics.
Symptoms
The development of symptoms of the disease occurs from two to fourteen days. The main difference between the viral form and the disease caused by bacteria is that there is no characteristic purulent plaque on the tonsils. The first signs that appear in the patient are in many ways similar to the development of catarrhal tonsillitis:
- high body temperature (up to 40°C);
- headache;
- lethargy;
- “aches” the joints;
- sharp pain in the throat;
- enlarged lymph nodes in the submandibular region.
After just a couple of days, symptoms characteristic of ARVI are added: cough, runny nose, sore throat, nausea, diarrhea, the appearance of small papules (rounded protrusions) on the tonsils.
Each type of viral sore throat has its own characteristics. So, with the adenoviral form, conjunctivitis and abdominal pain can occur. The disease usually goes away within two weeks.
The influenza form begins acutely with a sharp rise in temperature and is accompanied by a dry cough, severe headache, sore throat and runny nose. The illness usually goes away in seven to ten days.
In the herpetic form, blisters with gray liquid form on the tonsils. After three to four days they begin to burst.
Before the age of 6 months, the disease is extremely rare in infants, since the antibodies obtained with mother's milk protect against infections. After the child reaches three years of age, the number of these antibodies decreases, and infection with viruses occurs more and more often. As soon as the baby’s own antibodies increase, he becomes less susceptible to viruses, and outbreaks of the disease occur much less frequently. After three years, the frequent incidence of viral tonsillitis is associated with hypothermia in the cold season, a weak immune system and constant infection in preschool, school children's institutions and sports sections.
The peak of the disease occurs in the first five days, then the body temperature subsides. It is during this period that the patient is most contagious. As soon as the temperature returns to normal, it means that the virus has been controlled and there is no danger of infection for others. Cough and nasal discharge may be present until recovery, but their presence is not an indicator of contagiousness.
Treatment of tonsillitis in children
Treatment of tonsillitis in children should be under constant medical supervision. It is better not to self-medicate, as this can lead to complications. During illness, the child needs to stay in bed and drink plenty of fluids. It is mandatory to prescribe a gentle diet, as well as compliance with the rules of oral hygiene. To relieve pain, rinsing with herbal infusions is often done. Treatment often includes sprays with an anti-inflammatory and analgesic component or rinses. Local therapy also includes lozenges such as Faringosept , which have antimicrobial properties. If we talk about the treatment of chronic tonsillitis in a child, it is important to remember that treatment should be carried out both during the “quiet” period and during an exacerbation. If acute tonsillitis occurs, treatment in children usually goes like this: ● Rinsing with herbal infusions helps reduce pain. But the problem cannot be eliminated in this way, since only the symptoms are alleviated; ● To improve the condition of the tonsils, use anti-inflammatory sprays or lozenges; ●Sometimes the doctor advises cleaning the tonsils - washing them of purulent plugs. This procedure is prescribed to a patient with frequent exacerbations of chronic tonsillitis, experiencing constant pain in the throat and lymph nodes in the neck. Often, rinsing the lacunae of the tonsils is the only way to save the tonsils and avoid tonsillectomy (surgery to remove the tonsils). The procedure must be carried out outside the period of acute inflammation (angina).
To prevent frequent exacerbation of tonsillitis in a child, it is necessary to regularly strengthen the immune system. In the autumn and spring seasons, for prevention, take vitamin C and gargle with infusions of calendula, chamomile or sage. In addition, it is important for the child to spend a lot of time in the fresh air, ventilate and humidify the air in the room.
Possible complications
As a rule, the viral form of tonsillitis, if a sore throat is treated correctly and in a timely manner, does not pose a danger and goes away without complications.
ARVI can be complicated by the addition of a bacterial infection of the nasal cavity: a characteristic sign is green discharge from the nose. The prognosis for this development is favorable, just the duration of treatment will increase by several days.
Influenza viruses cause complications more often than other viruses. This can be pneumonia, lung abscess, hepatitis, diseases of the heart muscle, neuritis. Adenoviruses can cause sinusitis and pneumonia.
A common consequence of viral tonsillitis is infection of the oral cavity and pharynx by fungus. Bacterial tonsillitis often develops. Exacerbations of chronic diseases are possible.
Drugs for the treatment of tonsillitis in children
Treatment of tonsillitis in children includes drugs such as 2: ● Antiseptics. In this case, the drug Faringosept . It helps to effectively fight tonsillitis pathogens3. It can be recommended for children from 3 years old; ●Antibiotics - most often these are penicillins and cephalosporins. Antibiotics are prescribed by a doctor in the presence of a bacterial infection, because if taken incorrectly, complications can arise; ● Pain reliever. In this case, Faringosept lozenges are also suitable. They will help relieve sore throat 3; ● Antipyretics, because tonsillitis is often accompanied by high fever; ● Medicines to boost immunity and vitamins.
If you discover symptoms of tonsillitis in a child, it is better not to self-medicate, but to immediately go to the doctor.
What is chronic tonsillitis
The human oropharynx has special structures called tonsils; they protect the body from pathogenic microorganisms. In childhood, these structures are subject to enormous stress, because every day the child comes into contact with new microbes that are not yet familiar to him.
When bacteria “settle” on the surface of the tonsils on the back wall of the pharynx, and the immune system cannot cope with them, inflammation develops - tonsillitis. If this inflammation persists for a long time, acute tonsillitis (tonsillitis) turns into a chronic inflammatory process.
Tonsils in chronic tonsillitis do not perform their functions, but on the contrary, they become a source of infection. This leads to infectious and autoimmune complications.
Complications due to improper self-medication and lack of treatment for tonsillitis
There are a simple form of tonsillitis - accompanied only by local symptoms, and a toxic-allergic (complicated) - manifestations of intoxication and dysfunction of all organs and systems come to the fore.
Toxic-allergic manifestations are characteristic of chronic tonsillitis of streptococcal origin. With this form, antibodies to streptococci are formed in the blood, which are also capable of attacking the body’s own tissues. The most vulnerable to such autoimmune aggression are the kidneys, heart and joints. Therefore, chronic tonsillitis leads to the following complications:
- glomerulonephritis and subsequently renal failure;
- endocarditis, myocarditis, pericarditis;
- rheumatism, rheumatoid arthritis, systemic lupus erythematosus.
Therefore, any tonsillitis should be examined and adequately treated. It is necessary to monitor the child’s condition for 3-4 weeks after recovery. If alarming symptoms appear in the heart (chest pain, rapid heartbeat, high temperature), joints (pain with movement, stiffness), kidneys (swelling, lower back pain), seek medical help.
Causes of chronic tonsillitis
Tonsillitis
- infection. Among the pathogens that can cause tonsillitis are:
- bacteria (streptococci, staphylococci, diphtheria bacillus, etc.);
- ARVI (influenza viruses, parainfluenza, adenoviruses);
- herpes viruses (cytomegalovirus, Epstein-Barr virus);
- measles virus;
- yeast fungi (candida).
Provoking factors include hypothermia, consumption of cold foods, contact with sick people, stress, and poor nutrition. Candidal tonsillitis may indicate immunodeficiency.
Recommendations for the prevention of tonsillitis
To prevent the development of chronic tonsillitis, you must adhere to the following recommendations:
- avoid hypothermia of the child;
- protect him from communicating with sick people;
- monitor the child’s nutritional status;
- promptly show the child to a pediatrician or pediatric ENT doctor when the first symptoms of a sore throat appear;
- Visit the dentist with him in a timely manner to remove carious teeth, which are a source of bacterial growth in the mouth.