07.05.2018
A large number of patients are faced with the need to have teeth removed. Injuries, untimely contact with a dentist, errors in previous dental treatment and much more are the main causes of tooth loss.
Unfortunately, patients often put off compensation for the resulting defect after tooth extraction. At the same time, without suspecting that this entails consequences that do not provide the possibility of further restoration of teeth through implantation.
To understand this slightly confusing formulation, we will first try to describe what processes occur in the dental system after tooth extraction.
How do “eights” erupt?
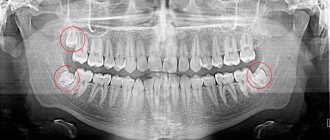
Wisdom teeth are the last teeth to erupt. Sometimes at 18–20 years old, but more often at a later age. In addition to the fact that these are the largest teeth, there are cases when they are located in the jaw bone not vertically, but at an angle. Therefore, problems most often arise with their eruption: the tooth does not grow upward, but to the side, pressing on the root of the nearest tooth, causing pain and inflammation. Often, to avoid such problems, wisdom teeth are removed without waiting for them to fully erupt.
Wisdom teeth often cause problems when they erupt
But if the tooth grows more or less without problems, the person does not see a dentist; there is no indication for tooth extraction. And then it turns out that due to the growth of molar No. 3, the front teeth have moved.
“Eights” are large teeth, and if there is not enough space in the dentition, they move neighboring teeth, and even the front ones.
Crowded teeth
Is it possible to remove a tooth and return everything as it was?
If you remove a tooth, nothing will change. Orthodontist patients know that after treatment a consolidation stage is needed, otherwise the roots of the teeth will begin to move to their old familiar place. It takes at least two years for the teeth to adjust and strengthen in their new position, and to do this they are held in place with the help of retainers and aligners.
During orthodontic treatment, the pressure from braces or aligners is much greater than that exerted by the growing wisdom tooth. Therefore, with an orthodontic system, teeth are moved within a few months, and the first results are visible within a few weeks.
Aligners correct the position of teeth in a few months
A growing molar erupts very slowly, over 2–3 years, and puts pressure on neighboring teeth, causing them to move. The process occurs almost imperceptibly, the teeth shift by fractions of a millimeter per month. During this time, they get used to the new (wrong) position. The ligamentous apparatus that supports the teeth is rebuilt to a new position, and the bone tissue around the roots is strengthened. And even if wisdom teeth are removed, it will not be orthodontically beneficial. Neither from a health point of view, nor from an aesthetic point of view.
How to stop the drift?
To prevent destruction, after the operation, restoration of the masticatory organs should be undertaken. To do this, the patient must contact an orthodontist. Braces are often required to correct an overbite. It happens that the hole becomes inflamed, causing the wound area to become infected and may fester. In such situations, cleaning and disinfection are performed. Therapeutic methods also include:
- Installation of removable corrective devices. They include a plastic plate. It is held in the mouth by hooks and wire loops. To straighten and return the units to the correct position, springs and arms are used. To further expand the jaw, an expansion screw is installed on the plate.
- Orthodontic devices that are not removable are represented by systems for correcting jaw closure. This effective technology allows you to correct the chewing organs of adults. The braces are fixed with special glue. A strong bracket is pulled to make the connection. It creates the right amount of force so that the units move in the right direction.
- In difficult situations, radical technologies are used. Treatment may involve face bows, which significantly change the configuration of the skull.
Nowadays, aligners and mouth guards are also used. They are suitable for patient patients. The correction period takes from 12 months to 2.5 years. The aligners are changed every 15 days. The advantage of aligners is the transparency of the material. They can be removed for hygiene purposes or for eating.
What to do?
Treatment with braces or aligners will help correct the position of your teeth. However, it is not necessary to remove grown wisdom teeth. Whether to save them or not is decided individually in each case and only after examination. If it is possible to expand a row of teeth so that there is enough space for all teeth, then there may be no indication for removal. It is always better to preserve healthy teeth, this also applies to third molars.
If the teeth were initially straight and the erupting wisdom tooth has distorted them, a slight disturbance in the position of the teeth usually occurs. Regardless of the patient’s age, it can be corrected in a few months.
Types of tooth displacement
While everything is quite clear about why teeth shift, many people are confused about the types of this problem. All bite defects are divided into 3 large groups.
- Violation of the position of the teeth: normally there are very narrow spaces between the teeth, and each tooth, except the last in the row, has 2 contact points with its neighbors. If there are enlarged spaces (tremas, diastemas) or teeth are crowded, then this is a defect that needs to be corrected - otherwise it will lead to problems with the gums and increased tooth wear,
- Violation of the development of dentition - they can be either narrowed or expanded.
- Abnormalities affecting the size or position of the jaws. These include:
a) cross bite - the jaws close in a cross direction horizontally, i.e. the teeth overlap;
b) mesial bite - the lower jaw protrudes forward;
c) distal bite - the upper jaw protrudes forward.
If any tooth has changed position as a result of injury or removal of an adjacent tooth, this is also a malocclusion that can be corrected by orthodontists.
Gaps between teeth: classification, causes
A variety of reasons can lead to the appearance of three:
- Often we are talking about hereditary predisposition. If at least one parent has trema or diastema, the risk that the child will encounter the same problem is 30%;
- Sometimes the appearance of gaps between teeth is a consequence of bad habits. Among those people who often chew pens and pencils, the percentage of those suffering from gaps between teeth is significantly higher than among those who are free from such habits;
- loss of teeth. The loss of a tooth entails many problems: this is atrophy of bone tissue, this is the process of moving apart the remaining teeth, which entails the appearance of teeth. The displacement of teeth leads to a deformation of the bite, to a change in the entire process of chewing food, and this can negatively affect the functioning of the gastrointestinal tract and human health in general. That is why dentists recommend not to delay and carry out full dental prosthetics.
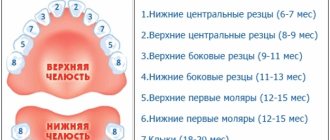
Depending on which teeth, milk or permanent, we are talking about, trema and diastema are divided into two groups: false and true. Trema are called false if they form between baby teeth, true - respectively, between permanent teeth. A false trema does not always degenerate into a true one, but this is a clear reason for parents to pay attention to the condition of their child’s oral cavity. Make an appointment with an orthodontist and follow his instructions - this will help you minimize the risk of gaps between your permanent teeth.
Problems with other teeth
Neighboring teeth gradually move to the place of the removed tooth. This leads to malocclusion. Also, in the first months after tooth loss, active bone resorption occurs. A depression forms in the gum above the empty socket. Because of this, the mucous membrane looks ugly.
The absence of even one tooth increases the load on other dental units. As a result, the enamel can wear off faster. This provokes the appearance of caries.
Misaligned teeth are more difficult to clean. Microbial plaque begins to form in hard-to-reach places. Gradually it turns into stone, provoking inflammatory processes and the progression of caries.
Dislocation of the lower jaw
If the mouth is opened wide during anesthesia and tooth extraction, dislocation of the lower jaw may occur. This complication is more common in patients with habitual dislocation. The occurrence of dislocation can be facilitated by relaxation of the masticatory muscles under the influence of conduction anesthesia.
Clinic and diagnosis of dislocation of the lower jaw
The clinic and diagnosis of mandibular dislocation is based on the patient’s complaints and clinical examination. The main complaint is pain in the preauricular area and the inability to close the teeth. Pain in patients with habitual dislocation may be moderate, as well as in patients who have undergone conduction anesthesia
Clinical manifestations: the patient cannot close his mouth; in case of unilateral dislocation, the jaw is shifted to the healthy side; in case of bilateral dislocation, it is shifted forward.
A symptom of elastic mobility is characteristic of a dislocation. The doctor, grasping the lower jaw on both sides with his index fingers and thumbs, attempts to establish it in a position of central occlusion. To some extent this is successful, but as soon as you stop holding the lower jaw, it returns to its original position.
Dislocation of the temporomandibular joint a - anterior b - posterior
Treatment of lower jaw dislocation
We complete the tooth extraction and then treat the dislocation of the lower jaw.
First way. The chair is lowered, its back is set vertically. The patient rests the back of his head against the headrest and fixes his hands on the armrests. The doctor stands in front of the patient, wraps the thumbs of the right and left hands with gauze napkins or a towel. He then grabs the lower jaw with both hands so that the thumbs rest on the chewing surface of the molars, and the rest cover the lower edge of the jaw. After this, the doctor presses firmly with his thumbs on the molars, moving the lower jaw down. Without ceasing to push the lower jaw down, the doctor moves it posteriorly. The sound of a click and the disappearance of the symptom of elastic fixation indicate that the dislocation has been eliminated. Having warned the patient about the possibility of recurrence of the dislocation when the mouth is opened wide, the doctor applies a chin-parietal bandage to the patient to limit the opening of the mouth. It is recommended to wear the bandage for 5-6 days.
Second way. The patient is seated in a chair in the same position. The doctor stands in front of the patient, inserts the index fingers of the right and left hands into the vestibule of the mouth and moves them along the anterior edge of the branch as high as possible, to the top of the coronoid process. Then the doctor sharply and firmly presses on the anterior edge of the coronoid process. The essence of the method is that, having felt pain in the area of the anterior edge of the coronoid process, the patient tries to avoid it by eliminating the pressure of the doctor’s fingers. He cannot move his head and entire body backwards, as they rest against the back and headrest of the chair. Therefore, subconsciously he tries to move the lower jaw down and back, i.e. carry out the movement of the lower jaw that is necessary to eliminate the dislocation. In this case, the doctor does not have to overcome the force of contraction of the masticatory muscles, as is done when using the first method to reduce a dislocation.
Main consequences after wisdom tooth removal
- Dry socket is a consequence that occurs due to the doctor using anesthetics and vasoconstrictor drugs at the same time. As a result, the arteries become spasmed, and a blood “sac” (clot), which is required for natural wound healing, does not form in the socket. .
- Pain in the socket area is a common condition that can last up to five days. If the pain does not go away, and after five days it becomes more active, you should urgently consult a doctor.
- alveolitis - inflammation that occurs due to the presence of infection in the oral cavity, tooth fragments;
- pointed edges of the alveoli are a consequence of unprofessional removal of the “eight”;
- osteomyelitis of the socket is a consequence of poor wound treatment in the first hours and days after surgery;
- exposure of the alveolar zone - an injury against which part of the bone is exposed;
- neuropathy of the alveolar nerve - when, during the elimination of the “8”, the nerves of the lower jaw were affected.
- The formation of abscesses and phlegmon is a common phenomenon that develops as a result of infection during surgery or wound treatment. An acute inflammatory process develops in the tissues, and a sac with purulent contents forms. The patient feels severe pain, the tissues in the surgical area become denser, the pain becomes throbbing and acute, the body temperature rises, the head feels dizzy, and the cheek puffs out.
Frequent complications after removal of a wisdom tooth in the upper jaw: alveolitis (inflammation of the socket), hematomas (when the doctor damages a vessel), bleeding (this area is abundantly supplied with blood), damage to the bottom of the sinus. jaws, swelling and inflammation of tissues.
Common complications after removal of a wisdom tooth in the lower jaw: gumboil, damage to adjacent nerve endings, bleeding, stomatitis, cysts, etc.
Signs of complications after wisdom tooth removal:
- the wisdom tooth socket becomes brown, sometimes acquiring a bluish tint;
- increased pain;
- swelling;
- increased body temperature;
- heavy bleeding;
- dry socket;
- weakness;
- weak appetite;
- pain when swallowing food and drinks;
- difficulties opening and closing the mouth, etc.
In case of all the complications listed above, you must definitely contact an experienced, trusted dentist. The doctor will conduct an examination, determine the problem and prescribe adequate treatment.
Fracture of the alveolar process of the jaw
A fracture of the alveolar process of the jaw can occur either due to the fault of the doctor (rough work, violation of the removal technique) or due to a pathological process (soldering of the tooth to the alveolar wall). Types of fracture of the alveolar part of the jaw: • fracture within the alveolus of the tooth being removed; • fracture within the periodontium of several teeth; • fracture of the alveolar process, extending beyond the dentition (fracture of the tubercle of the upper jaw).
Causes of fracture: • Compression of the bone during fixation of the forceps. • Too active dislocation, which leads to bending and breaking of the alveolar wall. • Pathological processes leading to a decrease in bone strength (cysts, tumors, osteomyelitis). • Osteoid type of articulation.
Diagnosis of a fracture of the alveolar process of the jaw
Diagnosis of a fracture of the alveolar process of the jaw is based on the nature of the complaints, medical history, examination and x-ray examination. Sometimes when a fracture occurs, you can hear a characteristic sound - a crack. When the alveolar process of the upper jaw is fractured along with the tubercle, quite severe bleeding from the venous plexus may occur.
Symptoms: • appearance of foamed blood in the wound; • passing a stream of air into the mouth during an increase in pressure in the nasal cavity (oronasal test); • the appearance of blood from the nasal passage on the affected side.
Treatment of a fracture of the alveolar process of the jaw
If the fragment of the alveolar process remains connected to the soft tissues, then it is fixed with a metal splint. Otherwise, the fragment is removed and the sharp edges are smoothed. After this, an osteotropic biological preparation can be injected into the alveolus, and the edges of the gums can be brought together with sutures.