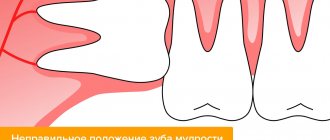
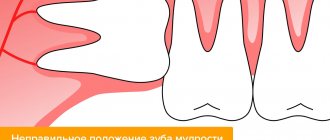
Temporary and permanent teeth have their own timing of eruption and specific locations on the alveolar process. Sometimes teeth erupt prematurely or remain in the bone, appearing much later (in this case, it bears the common name - wisdom tooth). Delayed teething is called “retention.” Sometimes teeth, including wisdom teeth, occupy an incorrect position, shift in the vestibular, palatal, lingual direction, and are rotated around their axis. This anomaly is called “dystopia”. Most often, the upper canines and lower wisdom teeth are affected by delay.
The presence of an impacted tooth (that is, the eruption of a wisdom tooth is delayed indefinitely) in the jaw in some cases does not cause any pathological phenomena in the patient. In this case, wisdom tooth removal is not urgent. But if an impacted tooth causes the formation of cysts, neuralgic pain, or an inflammatory process, then an atypical tooth extraction operation is used.
How are wisdom teeth different from other teeth?
- Wisdom teeth erupt between the ages of 18 and 25, and often later.
- Wisdom teeth do not have a distal neighbor that would prevent the tooth from moving distally.
- The wisdom tooth does not have a milk predecessor that would prepare the conditions for its eruption.
- Erupting at the age of 18-25 years, when the formation of the jaw bone tissue is completely completed, the tooth has to overcome a significant mechanical obstacle.
- The pterygomaxillary and external oblique lines thicken the cortical plates in the projection of the angle of the lower jaw and, thereby, create additional difficulties for the eruption of wisdom teeth
The difficult eruption of wisdom teeth is explained by the anatomical features of the structure of the lower jaw and the late timing of eruption. The lack of space in the dentition for the third molar - this is what the wisdom tooth is called in dental terminology - is associated with changes in the masticatory apparatus in the process of human evolution. The softer the food became, the less chewing stress was required on the teeth, which over time led to a decrease in the size of the jaws. Studies have shown that in modern humans, the width of the dental arch has decreased by 10-12 mm compared to distant ancestors.
If there is difficulty in the eruption of a wisdom tooth, it is necessary to consult a dentist and decide on its future fate. A general medical and dental history helps the dentist collect all medical information about the patient’s health, since the more the dentist knows not only about how the wisdom tooth is cut, but also about the patient’s health in general, the better he will be able to imagine the methods and methods of the upcoming treatment. The dentist must find out whether the patient suffers from any other disease and what medications he is taking.
After the dentist has collected an anamnesis and examined the patient, he begins an X-ray examination, with the help of which he assesses the condition of the wisdom tooth and gums, its roots, the bone located around the root and the degree of immersion of the wisdom tooth. After a thorough examination of the patient, the dentist decides whether wisdom tooth removal is necessary or not.
The operation of an impacted wisdom tooth begins with determining access to the tooth. Then a triangular-shaped mucoperiosteal flap is cut out, the bone tissue located above the tooth is removed, and the wisdom tooth is removed in parts or entirely. Then the flap is fixed with sutures, and the hole is tamponed with iodoform turunda.
The operation is performed under local anesthesia. In some cases, to improve psychological well-being, the doctor advises the patient to take medications to reduce anxiety during and after wisdom tooth removal.
Extraction methods
The standard method of removal for third molars is rarely used, only on the condition that eruption has proceeded normally, and the figure eight itself is in the correct position and has a normal root structure. Dentists at the Dentospas clinic recommend performing a more gentle and safe atraumatic removal of:
- after dissection of the gums or detachment of soft tissues, the tooth is divided into segments using a special tool;
- each of the segments along with the root is removed from the hole;
- the hole is processed, if necessary, stitches are applied.
Advantages:
- atraumatic removal is gentle on bone tissue. A small part of it can be removed if the molar is dystopic or impacted. Moreover, all manipulations are controlled, the doctor precisely regulates the volume of intervention, injury is minimal;
- if there are several roots, they have a non-standard location, are directed in different directions, and interfere with neighboring teeth, the atraumatic removal technique allows you to work separately with each of them. The root is removed safely, without damaging nearby tissues, regardless of its size, direction of growth, etc.;
- recovery after atraumatic removal is faster. It takes up to several days. The risk of complications is minimal.
At the Dentospas clinic, when removing wisdom teeth, precise diagnostics are used (to assess the position, number and condition of the roots, etc.). We perform third molar extraction using several methods. After the procedure, APRF technology can be used for faster healing.
Pericoronitis
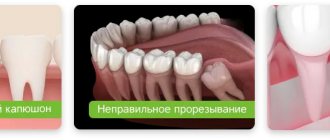
One of the common problems arising from incorrect tooth position is pericoronitis.
Pericoronitis is an inflammatory process of the tissues surrounding the wisdom tooth. The cause of pericoronitis is difficulty in the passage of the tooth through the gum. Even a small protrusion of a tooth above the gum can form a hole in it, which gradually expands, forming foci of infection. Plaque accumulates in this space between the gum and tooth and is difficult to clean.
Symptoms of pericoronitis include sensitivity and swelling of the gums surrounding the wisdom tooth. Sometimes there is severe pain, bad breath or a bad taste in the mouth.
If the dentist discovers that the cause of the development of pericoronaritis is an immersed wisdom tooth, then he suggests removing the wisdom tooth. The patient is prescribed a seven-day course of treatment. Antibiotics help reduce the infection, allowing the removal process and subsequent healing to go more smoothly. After a course of antibiotic treatment, the wisdom tooth is removed.
Removal of third molars
It is not always necessary to remove eights. If they have enough space in the jaw, they have normally located roots, grow vertically and erupt without complications, they can and should be preserved.
Indications for removal:
- complicated eruption, which is accompanied by swelling of the gums, severe or aching pain, inflammation, suppuration;
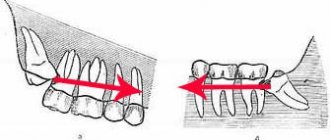
- incorrect location of dental roots, in which they interfere with the growth of neighboring teeth or gradually move or rotate them;
- incorrect position in the gum tissue - inclined or horizontal;
- absence of an antagonist tooth (for example, if the molars on the upper jaw have erupted correctly, but on the lower jaw they grow at an angle), violation of occlusion;
- small jaw size, in which there is no room left for the third molars, and they displace the entire dentition during eruption;
- inflammatory process in the root area, infectious, carious lesions, other dental diseases of third molars.
Periodontal diseases (gum diseases)
Misaligned wisdom teeth can lead to the development of periodontal disease. If the wisdom tooth is misaligned, the patient is unable to clean out plaque with a toothbrush and floss, which allows bacteria to develop and leads to periodontal disease. If such a disease is neglected, it can cause great harm to the gums and surrounding bone tissue. Periodontal disease does not develop in isolation around a single tooth, so to prevent it, the dentist recommends removing wisdom teeth that are incorrectly positioned.
Treatment
Depending on the picture and accompanying symptoms, the process of wisdom tooth removal is conventionally divided into simple and complex.
Easy removal
The operation begins with the administration of anesthesia.
During removal, specialists use forceps and elevators. No incisions are made for this type of intervention. The process of extracting a tooth from bone tissue lasts 2 to 10 minutes, depending on the location of the roots.
The resulting wound is treated with an antiseptic. If it is large, stitches are placed to reduce the risk of infection in the wound. A bandage with an anesthetic is applied to the area of manipulation, this is done to reduce bleeding.
Difficult removal
In the case of a complex operation to remove wisdom teeth, the necessary data is also collected and analyzed, and anesthesia is administered.
The operation is accompanied by dissection of the gums with a scalpel. To remove the tooth itself, it is cut into pieces using a drill. This is done to make it easier to remove. After removal, the resulting wound is treated with an antiseptic and then sutured.
Depending on the location of the tooth, the operation can take from 15 minutes to an hour and a half.
After the manipulations, regardless of their complexity, the doctor must consult the patient on wound treatment and, if necessary, prescribe medication.
Removal using ultrasound
In some cases, and with the appropriate equipment, a tooth can be removed using an ultrasonic scalpel. It allows for contactless intervention. Wounds with these manipulations heal faster, and the risk of complications is reduced.
Excision of a dental pocket with preservation of the tooth
There is a disease of the wisdom tooth in which its removal is called into question. This is an inflammation of the dental pocket, which is caused by bacteria that get under the gums. With this pathology, the doctor dissects the hood without affecting the tooth itself. The area of inflammation is treated with antiseptics.
The process of tissue healing and restoration, as a rule, proceeds quickly and the need for removal disappears. If the so-called pericoronitis has reached the stage at which ulcers form on the mucous membrane, the wisdom tooth is removed.
Postoperative complications for wisdom teeth
Dry sockets are one of the most common complications encountered during wisdom teeth removal. After a tooth is removed, a blood clot forms in the empty socket. Formation of a blood clot is an important part of the socket healing process. If for some reason a blood clot does not form, it results in a dry socket.
Dry sockets usually form after difficult extractions associated with significant trauma. Dry sockets appear as dry or sharp pain after wisdom tooth removal, 3-4 days later. There is a feeling that the pain on the wisdom tooth spreads from the extraction site towards the ear. Dry socket often causes an unpleasant taste or smell in the mouth.
To treat a dry socket, the dentist places a cotton swab with a medicine on the extraction site that reduces and soothes the pain. You should change your tampon every 24 hours until all symptoms disappear. This procedure may take several days.
Paresthesia is the most rare complication during the wisdom tooth extraction procedure. Paresthesia is a long-lasting numbness of the lip, tongue and chin. This happens because wisdom teeth may be located very close to the jaw nerves. And during the removal process, sometimes these nerves are touched or damaged. Usually the paresthesia lasts for several days, weeks or months: however, unfortunately, if the nerve is severely damaged, the paresthesia can become permanent.
Technique for removing a tooth from the lower jaw
- Using a dental smoother, the circular ligament surrounding the dental neck is peeled off. This stage is necessary to reduce damage to nearby soft tissues.
- Forceps delivery. Beak-shaped forceps are indicated for removing lower teeth.
- Move the forceps towards the root system.
- The tongs are clamped as tightly as possible.
- Loosening of the tooth. This stage, if the tooth is single-rooted, is done using the rotation method. Rotation – rotation along an axis. If the structural unit of the jaw is multi-rooted, then it is loosened using the method of luxation (loosening) - back and forth, left and right.
- Extraction from the hole.
- Inspect the hole for fragments and granulations; if there are any, remove them with a curettage spoon.
- A gauze pad is placed on the injured area.
- The patient is advised to discard the tampon after bleeding has stopped. This usually happens within 30 minutes. It is recommended not to eat for two hours. On this day, avoid too hot foods and physical activity.
Patients often ask the question: why can’t you eat exactly 2 hours? This is due to the action of the anesthetic. Removal of the lower units is always carried out under local anesthesia, as a result of which sensitivity is lost not only in the separate structure of the jaw, the entire half of the jaw bone is anesthetized, and along with it the soft tissues of the tongue and cheek. The anesthetic continues to act for 120 minutes, during which time, if a person begins to chew, he will bite his own tissues along with the food without feeling any pain, which will lead to serious injuries. Physical activity and hot foods and drinks can cause bleeding from the socket.
Age indications for wisdom tooth removal
There are no rules determining the optimal age for wisdom tooth removal. However, practice shows that the sooner you get rid of these teeth, the fewer complications you can expect from them. If there are very serious reasons for removing a wisdom tooth, it needs to be removed quickly. It is preferable to remove wisdom teeth when the roots of these teeth have not yet formed, and the bone surrounding the wisdom tooth is not yet very dense - this is late adolescence or early adolescence.
Diagnostics
Before removing a wisdom tooth, the surgeon needs to see a complete and accurate picture of its location. This is especially true in cases where the tooth has not erupted.
The specialist must prescribe an x-ray or orthopantomogram.
Before the operation:
- inspection;
- taking anamnesis;
- analysis of the received images.
Your feedback
I had my wisdom teeth removed at the RUTT clinic.
After six years of torment, during which he constantly made himself known at the most inopportune moments, she finally decided to break up with him. Removal was difficult (or so they said), with sawing and pulling out in parts. In terms of time, the doctor worked for at least 20-30 minutes. But it doesn’t feel like it hurts at all. Apart from picking at the jaw and pressing, I actually felt nothing. Unpleasant - yes, but not painful at all. Victoria |
10/31/2020 Leave a review Other reviews
Prevention after surgery
After the last molar is removed, the specialist gives instructions that must be strictly adhered to. This is done to prevent complications, speed up wound healing and restore the body. The doctor recommends:
- Do not eat food for several hours after surgery;
- On the first day, you can apply a cold compress to reduce swelling and inflammation;
- For the first two days, you should not rinse your mouth, so as not to remove the blood clot from the hole from which healing will occur;
- Hygienic care can be carried out as usual; teeth in the surgical area should be brushed very carefully;
- Take painkillers and other medications prescribed by your doctor;
- From the second day, the mouth can be rinsed with antiseptic solutions, decoctions of medicinal herbs, and mouth rinse;
- It is recommended to eat soft foods, avoid too hard, spicy, hot foods;
- Bad habits (smoking, drinking alcohol) should be eliminated;
- During the week you cannot visit the sauna, bathhouse, or gym.