The need to examine these organs for the presence of tumors and metastases is primarily explained by their structure. The thing is that it is the lymph nodes that are the first to be affected when metastases occur in the body, and their identification plays a very important prognostic role. Thanks to the examination of lymph nodes, it is possible to judge the stage of the disease, select treatment tactics, and also assess the volume of necessary surgical intervention.
About lymph
The lymphatic system consists of lymph nodes and the vessels that feed them. It is multifunctional, but its main function is to protect the body from various pathogens.
For this purpose, immune cells exist in the lymph nodes - T-lymphocytes and B-lymphocytes.
The passage of blood through small capillaries creates a plasma filtration effect. Some of the blood enters the surrounding tissues, and some goes back into the bloodstream. Another one - into the vessels. The result is the formation of lymph. It is a clear, watery liquid containing immune cells.
Lymphatic vessels, uniting, enter the thoracic lymphatic ducts, right and left, the same, in turn, flow into the veins. This results in the return of fluid to the bloodstream.
Lymph nodes, as part of the body's immune system, are located in different parts of the body. Their task is to be filters, a kind of barriers for infectious carriers and pathogenic cells.
Classification of lymphadenitis –
There are several classification options for lymphadenitis. For example, according to the localization of inflammation, lymphadenitis can be submandibular, submental, retromandibular, parotid, cervical, etc. According to the route of infection, lymphadenitis is divided into – 1) “odontogenic”, i.e. in this case, the infection is associated with the teeth, 2) “non-odontogenic”, i.e. associated with a viral or bacterial infectious process of a non-dental nature (this may include sepsis or a specific infection such as tuberculosis, syphilis, actinomycosis, AIDS).
The most important classification takes into account the severity of the inflammatory process and divides lymphadenitis into acute and chronic. In turn, acute lymphadenitis can be serous and purulent. It must be said that acute serous lymphadenitis, in which there is still no focus of purulent inflammation in the tissue of the lymph node (and there is only serous infiltration), is the only form of lymphadenitis that can be treated conservatively without surgical intervention. But very often patients go to the doctor too late, when foci of necrosis form in the tissues of the lymph node and a cavity with pus forms.
As for the chronic forms of lymphadenitis, there are hyperplastic, purulent and aggravated chronic. In the chronic hyperplastic form, there is a slow, constant increase in the volume of the lymph node (due to the replacement of lymphoid tissue - connective tissue). However, in the case when, against the background of weakened immunity or high virulence of the infection, inflammation spreads beyond the border of the lymph node capsule, adenophlegmon can form. It should be noted that each of the acute and chronic forms is characterized by its own special symptoms.
Acute and chronic lymphadenitis: symptoms
Lymphadenitis is characterized by a certain seasonality of the disease - most often it occurs in the autumn-winter period and early spring. In the first case, the outbreak is explained primarily by the active state of the immune system during this period, and an overreaction to any infection. In the spring, on the contrary, it is associated with the weakness of the immune system and the inability of the lymph nodes to resist a large volume of pathogenic microorganisms. So, let's move on to the symptoms of different forms of lymphadenitis...
1) Acute serous lymphadenitis - it is characterized by an enlargement of the lymph node (sometimes quite significant), as well as the appearance of pain. The general condition is satisfactory, the temperature is usually not higher than 37.5, there are no changes in the blood and urine. Upon palpation, an enlarged painful node is felt, usually round in shape, the skin is not fused to it (i.e., the skin above the lymph node gathers in a fold), and its color is not changed. As the inflammation subsides, the lymph node shrinks, gradually becomes softer, and the pain disappears (24stoma.ru).
2) Acute purulent lymphadenitis - if a child does not have an appointment with a dental surgeon or pediatrician for 5-7 days, then serous inflammation usually turns into purulent inflammation. This is also facilitated by active home self-medication in the form of various compresses and warming up. The rapid transition of serous inflammation into purulent inflammation is facilitated by an incorrect diagnosis by pediatricians, who immediately prescribe heat compresses, thereby accelerating the transformation of serous inflammation into purulent inflammation (as a result of which such children quickly end up in the maxillofacial department).
In acute purulent lymphadenitis, complaints are usually made about an enlarged lymph node, in which throbbing pain appears, a significant increase in body temperature up to 38.0 ° C, loss of appetite (in children this causes a change in behavior, the child becomes capricious and restless). In the projection of the inflamed lymph node, tissue swelling appears, and upon palpation a painful round-shaped infiltrate is felt. The skin in the projection of the lymph node becomes red and gradually fuses with the lymph node (i.e., it will not gather into a fold). Over time, a focus of softening may appear in the center of the infiltrate, i.e. symptom of fluctuation.
If the inflammation is localized in the retropharyngeal or parotid lymph nodes, then swallowing is usually painful, and mouth opening is most often limited. As for adults, their symptoms can occur in the same way as described above, but can often be erased. In the latter case, the formation of a purulent abscess inside the lymph node occurs slowly (sometimes within 2-3 weeks), and is not accompanied by severe general and local symptoms. Lack of treatment for acute purulent lymphadenitis can lead to pus leaving the capsule of the lymph node, i.e. into the surrounding tissues, and the development of a serious complication - adenophlegmon.
3) Chronic hyperplastic lymphadenitis - this form of lymphadenitis occurs mainly only in adults, it develops slowly (sometimes over 1-2 months or even more). Patients usually complain of the presence of some kind of round formation in the soft tissues, and sometimes also of weakness and malaise. The general condition is usually satisfactory, and only in the evening the temperature can rise to 37-37.5 °C. Initially, a painless or slightly painful pea appears deep in the tissues of the face or neck, which gradually enlarges and thickens.
On palpation, a round-shaped lymph node is palpable, with clear contours, mobile and not fused to the underlying tissues. Sometimes a significant proliferation of granulation tissue occurs in the lymph node, which extends beyond the lymph node capsule and grows to the skin, thinning it. When thinned skin breaks through, a fistulous tract usually forms, from which granulations bulge. This form of lymphadenitis can periodically worsen, and then during the period of exacerbation the symptoms will correspond to acute purulent lymphadenitis.
4) Chronic purulent lymphadenitis - this chronic form of lymphadenitis occurs in both children and adults. Patients usually complain of a long-term “ball” (usually in the submental or submandibular area), which does not cause any particular inconvenience. From a survey, you can usually find out that the ball first appeared several weeks or months ago - most often after pain in a tooth on the side of the inflamed lymph node. Subsequently, the pain in the tooth disappeared, but the slightly enlarged lymph node remained.
Patients may also note that over the course of several months there have been one or more cases of exacerbation of chronic inflammation, which was manifested by a slight increase in temperature, an increase in the size of the lymph node and its soreness. In this case, upon palpation, a dense, painful, limitedly mobile, round-shaped formation not fused to the skin is felt, in the center of which a focus of softening (fluctuation) can be detected.
5) Adenophlegmon - occurs when the lymph node capsule melts, when the pus contained in it penetrates into the surrounding loose tissue. Those. diffuse purulent inflammation occurs. Patients usually complain of intense, spontaneously occurring pain in any area, as well as deterioration in health, chills, and an increase in body temperature to 38-38.5 °C. In rare cases, adenophlegmons develop slowly, the symptoms are erased, and the body temperature does not exceed 37.5-38 °C.
Patients always usually say that the disease began with the appearance of a painful ball (pea), gradually increasing in size. Over time, a diffuse infiltrate appeared in the tissues, the skin on which became red and gradually stopped folding. The release of pus from the lymph node into the surrounding tissue is accompanied by an increase in the area of the infiltrate, the skin gradually becomes purple, and a focus of softening may appear in the center of the infiltrate. Treatment of adenophlegmon is only surgical; an urgent autopsy is indicated, and the location of the external incisions will depend on the location of the inflammation.
Establishing diagnosis -
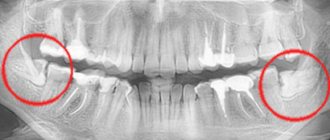
Diagnosis of odontogenic lymphadenitis is quite simple, because There is always a connection with toothache and gum inflammation. When examining the teeth in this case, you can find either a destroyed tooth, or a tooth under a filling or crown. Biting on such a tooth can be painful, or there was pain in it quite recently. There may be a fistula or lump on the gum in the projection of the causative tooth, and pressing on the gum can be painful. If the inflammation in the dental area is chronic and almost asymptomatic, then panoramic radiography will help us.
It can be more difficult to make a correct diagnosis with non-odontogenic lymphadenitis, which in this case must be distinguished from an abscess, phlegmon, sialadenitis, salivary stone disease, suppurating atheroma, as well as from specific lymphadenitis in syphilis, tuberculosis and actinomycosis. In acute forms of lymphadenitis, puncture plays a decisive role in making the correct diagnosis. Examination of punctate allows you to make a correct diagnosis and distinguish ordinary nonspecific infectious lymphadenitis from specific lesions (actinomycosis, tuberculosis, syphilis, as well as oncology).
In addition, chronic hyperplastic lymphadenitis must be distinguished from congenital cysts and fistulas of the face and neck, tumors, as well as from lymphogranulomatosis (puncture will also help us here). It is equally important to pay attention to other lymph nodes during the examination, because an increase in several groups of facial and cervical lymph nodes at once should alert you to certain blood diseases and HIV infection.
Localization of lymph nodes in the neck
Lymph nodes are located throughout the body. Now we are interested in the neck, where there are such groups of lymph nodes:
- Chin;
- Submandibular;
- Preglottic;
- Jugular;
- Parotid;
- BTE;
- Occipital;
- Posterior cervical;
- Supraclavicular.
Bone biopsy
A medical examination involves feeling them. An enlarged lymph node means certain pathological processes occurring in it. This can be an inflammatory, purulent process, the occurrence of infection, as well as oncology.
Indications
There are many indications for the procedure:
- Node over 1 cm;
- Soreness;
- Inflammatory process for no apparent reason;
- Suspicion of a malignant tumor;
- The lymph node does not change, although treatment has been carried out for a long time;
- Sarcoidosis or lymphogranulomatosis, etc.
This procedure provides an understanding of:
- What is the specificity of the course of the disease;
- What is the level of infection;
- If a patient with cancer has metastases.
How is the procedure done?
To examine the lymph nodes of the neck using an ultrasound, the patient will need to remove obstructive clothing and also remove jewelry. After this, you will need to lie down on the couch near the ultrasound machine, you can put a special cushion or a small pillow under your head - the doctor will tell you about this. Then a special gel is applied to the neck. The doctor examines the lymph nodes using an image that is displayed on the device’s screen. All data and pathologies are carefully recorded and will later be included in a report, with which you can go to your doctor.
Ultrasound of the lymph nodes of the child’s neck
A child may need an ultrasound of the lymph nodes of the neck in the same way as an adult. The examination itself does not cause any discomfort and can last about twenty minutes. During the examination of the lymph nodes, the baby's parents can be with him so that he does not worry. The only thing worth paying attention to is that the baby needs to be told not to move, since the results in this case may be inaccurate. Indications for ultrasound diagnostics are:
- persistent enlargement of nodes for two weeks after a cold or other illness;
- swollen lymph nodes without signs of any infectious disease of the ears, nose or throat;
- palpation under the skin of a dense enlarged node, which is tightly fused to the surrounding tissue;
- with a significant increase in the node compared to others.
It is worth knowing that the norm for an ultrasound of the neck lymph nodes for a child is one centimeter. In this case, the node can be clearly felt under the skin, this should not cause concern. If the lymph node enlarges to 1.5-2 centimeters, this is already a signal to visit a doctor.
Oncology and enlarged cervical lymph nodes
Some cancers (lymphomas) arise and develop in the lymph nodes. They are classified as:
- Hodgkin's lymphoma;
- Non-Hodgkin's lymphomas.
But more often metastases penetrate the lymph nodes.
This occurs due to the ability of cancerous tumors to metastasize. Benign tumors do not have this ability.
Breaking away from the lesion, the mutated cells migrate, enter the blood and lymphatic vessels and create secondary lesions. The lymph nodes adjacent to the primary lesion become the most vulnerable.
Complications of lymphadenitis –
As for complications, lymphadenitis can be complicated by adenophlegmon, and the latter can lead to the development of phlebitis, thrombophlebitis, and sepsis. The causes of complications are usually:
- a sharp weakening of the immune system due to viral and infectious diseases,
- if in the source of inflammation, in addition to the usual microflora (staphylococcus, streptococcus), there are also anaerobes (for example, clostridia and fusobacteria),
- errors in diagnosis,
- untimely start of treatment,
- improper treatment, including attempts at home self-medication.
Prevention of lymphadenitis is timely sanitation of the oral cavity, as well as foci of acute and chronic infection in the body. We hope that our article: How to treat neck lymphadenitis was useful to you!
Sources:
1. Higher medical education of the author of the article, 2. Based on personal experience in maxillofacial surgery and dental surgery, 3. National Library of Medicine (USA), 4. The National Center for Biotechnology Information (USA), 5. “Outpatient surgical dentistry" (Bezrukov V.), 6. "Pediatric surgical dentistry and maxillofacial surgery" (Topolnitsky O.).
Metastasis to cervical lymph nodes
Cervical lymph nodes are at greater risk of metastasis. It is there that metastases of squamous cell carcinoma of the upper respiratory tract, cancer of the thyroid gland, skin and salivary glands penetrate.
Sometimes the primary lesion is localized in another part of the body:
- Breast cancer – up to 4.5% of cases;
- Lung cancer – up to 32% of cases;
- Oncology of the esophagus – up to 30% of cases;
- Kidney cancer – up to 8% of cases;
- Testicular cancer – up to 4.5%.
Minor rates of metastasis were diagnosed in oncology of the cervix, uterine body, prostate, central nervous system, liver, bladder, and ovaries.
Lymph nodes of the neck
The current classification of the American Joint Committee on the Study of Malignant Tumors and the American Academy of Otorhinolaryngology and Head and Neck Surgery was modified by K. Robbins et al. in 2000 and approved by the AJCC-AAOHNS in 2001. It proposed dividing the 3 levels into sublevels. The classification of lymph nodes by level is known all over the world, is convenient to use, easy to remember and, most importantly, allows specialists to speak the same language. It has already become the basis for the classification of cervical dissections.
Using the classification of neck lymph nodes by level will help solve a number of problems that arise, in particular: 1) when determining the scope of surgical intervention and planning radiation therapy; 2) when a patient who was treated in one medical institution goes to another with an extract indicating that the patient underwent fascial-sheath excision of the tissue of the neck and the exact volume of intervention is not indicated. In the first situation, where, according to the ultrasound, there is a lesion in the cervical-supraclavicular zone without indicating the levels, it is difficult for us to assess the volume of the lesion. In the second situation, without a surgical protocol, it is impossible to know the exact extent of the previously performed operation.
Classification
I (IA and IB)
– below the body of the lower jaw (behind the branch of the lower jaw - this is already IIA);
IA - group of mental nodes
IB is a group of submandibular lymph nodes (located in front and behind the submandibular salivary gland). If the lymph nodes of this level or the gland itself are affected, it is removed.
II, III, IV – jugular
– along the neurovascular bundle (internal jugular vein) covered by m.sternoclaidomastoideus
II - upper jugular - from the level of the base of the skull to the level of the lower edge of the hyoid bone IIA - upper anterior jugular - anterior to the posterior edge of the internal jugular vein; IIB - superior jugular posterior - posterior to the posterior edge of the internal jugular vein.
III - middle jugular - from the level of the lower edge of the hyoid bone to the level of the lower edge of the cricoid cartilage of the larynx;
IV – lower jugular – from the level of the lower edge of the cricoid cartilage of the larynx to the clavicles (including Virchow’s);
V – posterior (lateral) triangle of the neck
corresponds to anatomical boundaries
VA – accessory – above the level of the lower edge of the cricoid cartilage, along the anterior surface of the trapezius muscle, VB – supraclavicular – below the level of the lower edge of the cricoid cartilage (excluding Virchow’s);
VI - anterior neck space - pre- and paratracheal lymph nodes, preglottic (Delphian) and parathyroid lymph nodes
, including lymph nodes along the recurrent laryngeal nerve)
Table
Groups of lymph nodes not included in the classification.
When describing all the groups of lymph nodes listed below, it is necessary to use traditional names.
1. Lymph nodes of the postauricular area.
2. Suboccipital lymph nodes.
3. Parotid lymph nodes (inside and extraparotid salivary gland).
4. Lateral and medial retropharyngeal lymph nodes (their defeat is important for cancer of the nasopharynx and oropharynx).
5. Facial lymph nodes.
6. Upper mediastinal lymph nodes (not related to the lymph nodes of the neck).
Examples of lymphadenopathy of different groups of lymph nodes in the neck.
The CT image below shows necrosis of group IA lymph nodes.
The CT image below shows group IB lymphadenopathy on the right.
The post-contrast CT image shown below shows a patient with tongue carcinoma and lymphadenopathy of group II lymph nodes.
The post-contrast CT image below shows enlargement and contrast enhancement of group III lymph nodes.
On the post-contrast image, the white arrow indicates an enlarged group IV lymph node. The patient had the right lobe of the thyroid gland and the right jugular vein removed, as indicated by the black arrow, due to papillary carcinoma.
On the post-contrast image, the white arrow indicates an enlarged group V lymph node.
On the post-contrast image, the white arrow indicates an enlarged group VI lymph node.
Source
- Cervical lymphadenopathy: what radiologists need to know Vincent Chong Department of Diagnostic Radiology, Singapore General Hospital, Singapore Corresponding address: Vincent Chong, Department of Diagnostic Radiology, Singapore General Hospital, Outram Road, Singapore 169608. Date accepted for publication 19 January 2004
- S. Subramanian1,2, V.L. Lyubaev1, V.Zh. Brzhezovsky1, A.A. Aidarbekova1 CLASSIFICATION OF LYMPH NODES OF THE NECK: THE NEED FOR TRANSITION TO MODERN CLASSIFICATION IN ONCOLOGICAL PRACTICE 1 Research Institute of Clinical Oncology, State Russian Cancer Research Center named after. N. N. Blokhina RAMS, Moscow 2 Department of Oncology, Moscow Medical Academy named after. I. M. Sechenova, Moscow
- CT diagnostics of malignant tumors of the oral cavity, pharynx, larynx. Kuraeva Lyudmila MDC-Dimitrov, Koritko Yuri MC Tomograd.
- Radiology Assistant
- Radiomed
How to detect metastases in lymph nodes
The problem is not simple, since if there are a small number of mutated cells in the lymph nodes, there are usually no symptoms. If there is any suspicion, the doctor must make an accurate diagnosis.
This is where lymph node biopsy comes to the rescue. It is carried out in different ways:
- Biopsy with needle insertion into a questionable node. Carry out under local anesthesia. The procedure takes up to 30 minutes.
- Open biopsy. This is a surgical procedure performed under anesthesia, local or general, with the removal of part or all of the lymph node.
- Sentinel lymph node biopsy. A radiopharmaceutical or fluorescent dye is injected into the tumor. Penetrating the lymph vessels, it reveals the problem node, the so-called sentinel node.
After the biopsy procedure, all materials are sent to the laboratory for study.
Consequences
In general, patients easily tolerate the procedure; there are no consequences or complications. But you still have to deal with symptoms that arise as consequences of the procedure. It can be:
- Feeling weak;
- Temperature increase;
- Painful sensations in the head and neck area;
- Dizziness;
- Nerve pinching or damage
Unpleasant consequences can be caused by insufficient qualifications of the doctor - damage to the vessel, penetration of bacteria.
If you experience the above symptoms, you should consult a doctor. At the Onco.Rehab oncology clinic, you can get the addresses of our reliable partners, where lymph node biopsies are performed in accordance with international standards.
Lymphadenitis: treatment
In the treatment of lymphadenitis, the main thing is to eliminate the cause of its occurrence.
Accordingly, in case of odontogenic lymphadenitis, depending on the condition of the tooth and the age of the child, it is necessary to treat or remove the causative tooth. If in adults it is desirable to preserve a tooth in all possible cases, then in children the situation is much more complicated. In children, inflammation at the root apex is treated only in permanent teeth; baby teeth must be removed. This is due to the wide root canals of baby teeth, the immaturity of the apexes of the roots of baby teeth, on which huge apical foramina gape. Such teeth cannot be properly filled, plus there is too great a risk of injury to the permanent tooth germ. Numerous attempts to treat such teeth end in almost 100% of cases with complications - the development of purulent periostitis, inflammation and loss of the permanent tooth germ, sometimes with sepsis and even death. And this is not to mention the fact that the long-term presence of a focus of purulent inflammation in a child affects the entire body, suppresses its immunity, contributing to the occurrence of frequent infectious diseases, allergic reactions, bronchial asthma and other pathologies. This is worth remembering when a not very competent doctor suggests not removing such a tooth, citing possible problems with the bite in the future.
Accordingly, if it is possible to save a permanent tooth in a child or an adult, the tooth is opened (removal of carious tissue, old filling or crown, revision of the root canals) to create an outflow of pus through the root canal. Next, general therapy is prescribed, and after the cessation of suppuration, the inflammatory focus at the apex of the tooth root is treated in the standard way, as for chronic periodontitis, i.e. with placing a special medicinal paste into the root canals. All these actions will prevent further transmission of infection from the source of inflammation - to the lymph nodes.
1) Treatment of serous lymphadenitis -
The treatment tactics for serous lymphadenitis will depend on what day after the onset of the disease the patient went to the doctor (the earlier, the greater the chance of success of conservative treatment). In this case, conservative treatment is first used - compresses with a 5% solution of dimexide, in which anti-inflammatory medications are dissolved. To do this, add 1 ml of hydrocortisone solution, 50% analgin solution and 1% diphenhydramine solution to 10 ml of a 5% dimexide solution.
Drug Dimexide (99% concentrate) –
Next, apply a classic compress to the area where the affected lymph node is located. A gauze cloth is generously moistened with the solution, and a plastic film is placed on top of it (to isolate the solution from air). Under no circumstances should you make a thermal compress by placing any material or towel over the film. Thermal procedures, if this is not 1-2 days of development of the disease, will only aggravate congestion in the lymph node and will contribute to the development of pathogenic microorganisms, i.e. the transition of serous inflammation to purulent (for the same reason, you should not do UHF, bandages with Vishnevsky ointment).
If a child or adult consults a doctor in the first 2-3 days from the onset of the disease, the most effective is the use of physiotherapy methods - phonophoresis of hydrocortisone, electrophoresis of dimexide with an antibiotic and diphenhydramine, laser therapy.
2) Treatment of purulent forms of lymphadenitis -
Surgery is used to treat acute purulent lymphadenitis, exacerbation of chronic purulent lymphadenitis, adenophlegmon. The operation is performed in a hospital setting under general anesthesia, and it is necessary to scrape the necrotic tissue of the lymph node from the wound. In case of chronic hyperplastic lymphadenitis, it is better to remove the lymph node followed by histological examination (moreover, if there is a fistulous tract with granulations growing to the surface of the skin, the lymph node is removed along with the fistulous tract).
After opening the abscess, physiotherapy is prescribed - enzyme electrophoresis, UHF, magnetic therapy, helium-neon irradiation, ultraviolet radiation. Depending on the severity of inflammation, intoxication and the state of immunity, various medications are used. First of all, these are detoxification and antihistamines, sometimes antibiotics. For inflammation of the lymph nodes, not just any antibiotics are used, but those that tend to accumulate in the lymph nodes, for example, the combination of ampicillin + sulbactam, cefazolin, claforan).
Removal of a lymph node for hyperplastic lymphadenitis –