Finlepsin® (Finlepsin®)
Monotherapy for epilepsy begins with a low initial dose, gradually increasing it until the desired therapeutic effect is achieved.
When selecting the optimal dose, it is advisable to determine the concentration of carbamazepine in the blood plasma, especially during combination therapy. In some cases, the optimal dose may deviate significantly from the recommended initial and maintenance dose, for example, due to the induction of microsomal liver enzymes or due to interactions during combination therapy.
Finlepsin® should not be combined with sedative-hypnotics. If necessary, it can be combined with other substances used to treat alcohol withdrawal. During treatment, it is necessary to regularly monitor the content of carbamazepine in the blood plasma. Due to the development of side effects from the central and autonomic nervous system, patients are closely monitored in a hospital setting. When transferring a patient to carbamazepine, the dose of the previously prescribed antiepileptic drug should be gradually reduced until it is completely discontinued. Sudden cessation of carbamazepine may trigger epileptic seizures. If it is necessary to abruptly interrupt treatment, the patient should be transferred to another antiepileptic drug under the cover of the drug indicated in such cases (for example, diazepam administered intravenously or rectally, or phenytoin administered intravenously).
Several cases of vomiting, diarrhea and/or decreased nutrition, convulsions and/or respiratory depression have been described in newborns whose mothers took carbamazepine concomitantly with other anticonvulsants (these reactions may represent neonatal withdrawal syndrome). Before prescribing carbamazepine and during treatment, liver function testing is necessary, especially in patients with a history of liver disease, as well as in elderly patients. If existing liver dysfunction worsens or active liver disease develops, the drug should be discontinued immediately. Before starting treatment, it is necessary to conduct a study of the blood picture (including counting platelets, reticulocytes), iron level in the blood serum, general urine analysis, urea level in the blood, electroencephalogram, determination of the concentration of electrolytes in the blood serum (and periodically during treatment, because hyponatremia may develop). Subsequently, these indicators should be monitored weekly during the first month of treatment and then monthly.
In most cases, a transient or persistent decrease in the number of platelets and/or leukocytes is not a precursor to the onset of aplastic anemia or agranulocytosis. However, before starting treatment, and periodically during treatment, clinical blood tests should be performed, including platelet counts and possibly reticulocyte counts, and serum iron levels should be determined. Non-progressive asymptomatic leukopenia does not require discontinuation, however, treatment should be discontinued if progressive leukopenia or leukopenia accompanied by clinical symptoms of an infectious disease occurs. Carbamazepine should be discontinued immediately if hypersensitivity reactions or symptoms suggestive of Stevens-Johnson syndrome or Lyell's syndrome occur. Mild skin reactions (isolated macular or maculopapular exanthema) usually disappear within a few days or weeks, even with continued treatment or after reducing the dose of the drug (the patient should be under close medical supervision at this time).
The possibility of activation of latent psychoses should be taken into account, and in elderly patients, the possibility of developing disorientation or psychomotor agitation.
In some cases, treatment with antiepileptic drugs was accompanied by the occurrence of suicide attempts/suicidal intentions. This was also confirmed in a meta-analysis of randomized clinical trials using antiepileptic drugs. Since the mechanism of suicide attempts when using antiepileptic drugs is not known, their occurrence cannot be ruled out when treating patients with Finlepsin®. Patients and staff should be warned to monitor for suicidal thoughts/behavior and to seek immediate medical attention if symptoms occur.
Male fertility and/or spermatogenesis disorders are possible, but the relationship between these disorders and carbamazepine has not yet been established.
Intermenstrual bleeding may occur with simultaneous use of oral contraceptives. Carbamazepine may adversely affect the reliability of oral contraceptives, so women of reproductive age should use alternative methods of birth control during treatment.
Carbamazepine should only be used under medical supervision. Patients should be informed of early signs of toxicity, as well as skin and liver symptoms. The patient is informed of the need to immediately consult a doctor in case of adverse reactions such as fever, sore throat, rash, ulceration of the oral mucosa, causeless bruising, hemorrhages in the form of petechiae or purpura.
Before starting treatment, it is recommended to conduct an ophthalmological examination, including fundus examination and measurement of intraocular pressure. If the drug is prescribed to patients with increased intraocular pressure, constant monitoring of this indicator is required.
Patients with severe cardiovascular diseases, liver and kidney damage, as well as elderly people are prescribed lower doses of the drug. Although the relationship between the dose of carbamazepine, its concentration and clinical efficacy or tolerability is very small, regular determination of carbamazepine levels may be useful in the following situations: with a sharp increase in the frequency of attacks; to check whether the patient is taking the drug properly; during pregnancy; when treating children or adolescents; if there is a suspicion of impaired absorption of the drug; if toxic reactions are suspected if the patient is taking several medications.
During treatment with Finlepsin® it is recommended to refrain from drinking alcohol.
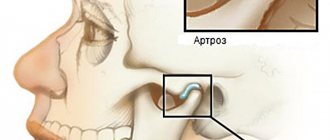
Causes of inflammation of the trigeminal nerve
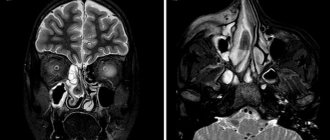
Doctors believe that the main cause of inflammation of the trigeminal nerve is compression of it either inside the skull or outside it. Inside the skull, the trigeminal nerve can be compressed as a result of the formation of tumors, in most cases resulting from some kind of head injury.
Also a fairly common cause of inflammation of the trigeminal nerve is internal venous or arterial displacement.
Other causes of trigeminal neuralgia include:
- the presence of a chronic inflammatory process, viral or bacterial infection in the body;
- herpes infection (herpes);
- a brain tumor;
- scarring in the brain stem;
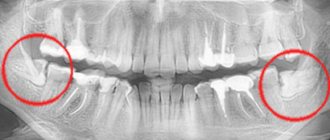
- failure of anesthesia during treatment or tooth extraction.
Most often, inflammation of the trigeminal nerve affects women at pre-retirement and retirement age (usually from fifty to seventy years). If trigeminal neuralgia is diagnosed in a young man or girl, then most likely its cause is a change in the arteries of a sclerotic nature or a strong dilatation of blood vessels.
Compound
| Long-acting tablets | 1 table |
| active substance: | |
| carbamazepine | 200 mg |
| 400 mg | |
| excipients: Eudragit® RS30D (ethyl acrylate, methyl methacrylate and trimethylammonioethyl methacrylate copolymer (1:2:0.1) - 11/22 mg; triacetin - 2.2/4.4 mg; talc - 15.6/31.2 mg; Eudragit® L30D-55 (methacrylic acid and ethyl acrylate copolymer) - 35/70 mg; MCC - 21.8/43.6 mg; crospovidone - 12.4/24.8 mg; colloidal silicon dioxide - 1.33/2, 66 mg; magnesium stearate - 0.67/1.34 mg |
Overdose
Symptoms: symptoms that occur during overdose usually reflect disorders of the central nervous system, cardiovascular and respiratory systems.
Central nervous system and sensory organs: depression of central nervous system functions, disorientation, drowsiness, agitation, hallucinations, coma, blurred vision, slurred speech, dysarthria, nystagmus, ataxia, dyskinesia, hyperreflexia (initially), hyporeflexia (later), convulsions, psychomotor disorders, myoclonus, hypothermia, mydriasis.
Cardiovascular system: tachycardia, decreased blood pressure, sometimes increased blood pressure, intraventricular conduction disturbances with widening of the QRS complex, fainting, cardiac arrest.
Respiratory system: respiratory depression, pulmonary edema.
Digestive system: nausea and vomiting, delayed evacuation of food from the stomach, decreased colon motility.
Urinary system: urinary retention, oliguria or anuria, fluid retention, hyponatremia.
Laboratory indicators: leukocytosis or leukopenia, hyponatremia, possible metabolic acidosis, hyperglycemia and glycosuria, increased muscle fraction of creatine phosphokinase.
Treatment: there is no specific antidote. Symptomatic supportive treatment in the intensive care unit, monitoring of heart function, body temperature, corneal reflexes, kidney and bladder function, and correction of electrolyte disorders are necessary. It is necessary to determine the concentration of carbamazepine in plasma to confirm poisoning with this drug and assess the degree of overdose, gastric lavage, and the administration of activated charcoal. Late evacuation of gastric contents can lead to delayed absorption on days 2 and 3 and the reappearance of symptoms of intoxication during the recovery period). Forced diuresis, hemodialysis and peritoneal dialysis are ineffective, however, dialysis is indicated for a combination of severe poisoning and renal failure. Children may require blood transfusions.
Treatment of inflammation of the trigeminal nerve
The first stage of treatment for inflammation of the trigeminal nerve is medication. It is aimed at reducing the strength and frequency of pain in the patient. Most often, doctors prescribe anticonvulsants to a patient suffering from trigeminal neuralgia. Sedatives are also used.
Physiotherapeutic procedures, as well as resorption therapy to relieve the inflammatory process, have a good therapeutic effect. Next, the doctor may recommend the use of laser treatment, in which the laser is directed cutaneously to the area where the processes of the trigeminal nerve exit the skull.
Our clinic is located in the same building as the multidisciplinary clinic “Diamed on Shchelkovskaya”, where special conditions for receiving physiotherapeutic procedures are organized for dental patients. The clinic’s physiotherapy room is equipped with modern equipment, including a laser physiotherapy device, with which you will feel relief after the first procedure. The pain will go away and you can return to normal eating. Make an appointment with a dentist by calling 8 or using the online appointment form. The doctor will make an accurate diagnosis and refer you for treatment.
If you are in severe pain, but for some reason you have not yet made an appointment with us, then it can be relieved with folk remedies. Take one tablespoon of yarrow, pour a glass of boiling water, let it brew for one hour and strain. The tincture should be taken one tablespoon before meals three to four times a day.
Why do teeth hurt when the trigeminal nerve is inflamed?
How is inflammation of the trigeminal nerve related to teeth? The connection here is the most direct. Firstly, severe pain during attacks “radiates” to the upper or lower jaw (depending on which nerve extension is inflamed), and sometimes to both jaws. This causes severe and unbearable toothache.
Secondly, those nerves that are found in the upper and lower teeth and gums are directly connected to the trigeminal nerve. The second branch of the trigeminal nerve innervates the upper teeth and gums, and the third, respectively, the lower jaw and gums.
The trigeminal nerve can also be damaged during a number of dental manipulations. Unsuccessful tooth extraction or improper filling, surgical intervention in the jaw structure that ended unsuccessfully, and injuries can cause trigeminal neuralgia.
It is very important to distinguish inflammation of the trigeminal nerve from other diseases of the oral cavity, in particular pulpitis - inflammation of the internal dental tissues. A characteristic sign of inflammation of the trigeminal nerve is that, despite severe pain, the sensitivity of the teeth does not increase when they come into contact with cold and hot foods, and hypothermia or heating does not provoke the onset of a new pain attack. Acute tooth sensitivity is a symptom of pulpitis.
When the trigeminal nerve is damaged in the jaw area, acute toothache, pain in the chin, ears and sometimes in the lower lip occurs. The pain may become increasingly intense, and often the patient continues to feel a dull ache after the attack.
Pharmacokinetics
Absorption is slow but complete (food intake does not significantly affect the speed and extent of absorption). After a single dose of the tablet, Cmax is reached after 32 hours. The average Cmax of unchanged active substance after a single dose of 400 mg of carbamazepine is about 2.5 μg/ml. Css of the drug in plasma are achieved in 1–2 weeks (the speed of achievement depends on the individual characteristics of metabolism: autoinduction of liver enzyme systems, heteroinduction by other simultaneously used drugs), as well as on the patient’s condition, the dose of the drug and the duration of treatment. There are significant individual differences in Css values in the therapeutic range: in most patients these values range from 4 to 12 μg/ml (17–50 μmol/l). Concentrations of carbamazepine-10,11-epoxide (a pharmacologically active metabolite) are approximately 30% of those of carbamazepine. Communication with plasma proteins in children is 55–59%, in adults – 70–80%. Apparent Vd - 0.8–1.9 l/kg. In the cerebrospinal fluid and saliva, concentrations are created that are proportional to the amount of active substance not bound to proteins (20–30%). Penetrates through the placental barrier. The concentration in breast milk is 25–60% of that in plasma. Metabolized in the liver, mainly along the epoxide pathway with the formation of the main metabolites - active carbamazepine-10,11-epoxide and an inactive conjugate with glucuronic acid. The main isoenzyme that ensures the biotransformation of carbamazepine into carbamazepine-10,11-epoxide is cytochrome P450 (CYPZA4). As a result of these metabolic reactions, a metabolite, 9-hydroxymethyl-10-carbamoylacridan, is also formed, which has weak pharmacological activity. Carbamazepine can induce its own metabolism. T1/2 after oral administration of a single dose is 60–100 hours (on average about 70 hours); with prolonged use, T1/2 decreases due to autoinduction of liver enzyme systems. After a single oral dose of carbamazepine, 72% of the dose taken is excreted in the urine and 28% in the feces; in this case, about 2% of the dose taken is excreted in the urine in the form of unchanged carbamazepine, about 1% - in the form of a 10,11-epoxide metabolite.
There is no data indicating that the pharmacokinetics of carbamazepine changes in elderly patients.
Prevention
There is no specific prevention against neuralgia. Doctors only recommend eliminating as much as possible exposure to the body of those risk factors that can lead to nerve inflammation. To avoid this, it is necessary to prevent hypothermia of the face, especially in the summer when using fans and air conditioners. It is important to harden yourself and worry less in order to reduce the impact of stress. It is also imperative to treat underlying diseases that are risk factors for neuralgia.