01.12.2019
Neglect of oral health leads to various dental diseases with complications. One of them is the overgrowing of the destroyed tooth crown with flesh. Why gums grow in the cavity and how to get rid of this anomaly, we will consider later in the article.
When is a tooth root 100% subject to extraction?
Tooth root removal is performed if:
- the root is softened below the gum level,
- the root of the tooth is below the level of the surrounding bone tissue,
- the root of the tooth has cracks
:
- the root of the tooth is chipped
:
- the root of the tooth is severely damaged, for example as a result of canal treatment with resorcinol
:
- There are various inflammatory processes around the root and under the root of the tooth - cyst, cystogranuloma
:
- the root of the tooth is mobile,
- there is a deep dental pocket.
Home care and postoperative period
After treating gum recession, your doctor may prescribe antibiotics, rinses, topical gels, and other topical treatments to prevent complications and speed up the healing process. It is also important to prefer gentle, soft food at a comfortable temperature, and perform regular hygiene according to the recommendations of a specialist.
The dentist will recommend replacing your hard toothbrush with a soft one, and as healing progresses, you will likely need a toothbrush with medium-hard bristles. In addition, the doctor will definitely show the correct cleaning movements and tell you what pressure will be optimal. In many cases, such measures are sufficient to eliminate the causes of exposed tooth necks, as well as maintain treatment results.
How is tooth root removal done?
Are there any features or important points when removing a tooth root? Of course, any removal - be it tooth extraction, wisdom tooth removal, impacted tooth or tooth root should be carried out as atraumatically as possible, preserving the tissue structure
that surround a tooth or tooth root:
The goal of atraumatic root removal is to preserve bone
. Removal should be done painlessly.
The clinics of the German Implantology Center are supporters of atraumatic and painless removal. Our technologies have been proven over the years, and our patients feel very comfortable with them. It is no secret that many patients have fears about removal, and these fears sometimes postpone the surgical stage of treatment for a long time. In our clinics, we help patients overcome these fears. The patient may not be afraid of anything - both in the case of a single extraction and in case of multiple extractions of teeth
:
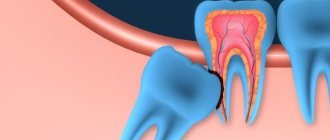
Ingrowth of gingival papillae
Pathology develops due to chipping/destruction of molars or incisors on one side. The tissue between the teeth is constantly injured, which contributes to its abnormal growth. The flesh increases in volume, filling the free space. At the beginning of the activation of abnormal processes, the patient experiences pain and discomfort. In the latent state, pain decreases. However, the papilla continues to grow and causes discomfort when it reaches a large size. When eating food or brushing teeth, the gums are constantly injured.
What is atraumatic tooth root removal?
What instruments does the surgeon use to achieve atraumaticity? For atraumatic removal, special instruments are used - thin, neat and elastic elevators that can minimally invasively penetrate and expand the periodontal tissue that connects the tooth root directly to the jaw. Using special instruments, the periodontal ligaments are cut so that the root can be removed as carefully as possible, in its “pure form.”
The vestibular plate that surrounds the bone is very thin. And we work with her carefully when removing teeth. It may also be necessary to saw the root of the tooth so that it can be removed in pieces. Sawing can be carried out with oscillating ultrasonic attachments - ultrasonic knives. Cutting the root of a tooth can be done quite effectively with a high-quality thin surgical dental bur, which has a certain length.
After cutting the root, the medial wall of the root is first removed, and then the vestibular wall of the root is removed. This allows for maximum preservation of surrounding tissue.
Then, after such removal, you can preserve the tooth socket or place an implant so that the bone is preserved as much as possible. Preservation of the tooth socket is carried out if there are no conditions for installing an implant at once, or if the patient undergoes delayed implantation.
If the roots of wisdom teeth are removed, the socket is not preserved; it is enough to remove them as atraumatically as possible. Let's talk about this in a little more detail.
Features of root removal of decayed wisdom teeth
Are there any difficulties when removing the roots of wisdom teeth? Removing the roots of wisdom teeth requires that the surgeon has sufficient experience. Often the roots of these third molars (wisdom teeth) are located close to the mandibular canal. Often the roots of molars are adjacent to the upper or lateral wall of the mandibular canal. The configuration of wisdom tooth roots is extremely diverse and sometimes extremely difficult to remove:
Therefore, when removing the roots of wisdom teeth, it is imperative that the patient undergo a CT scan. And the surgeon, as I said, needs to have some experience in surgical training in order to avoid the risks of removing the roots of such teeth and carry out the manipulation as efficiently as possible.
Like any root teeth, the roots of wisdom teeth are removed by cutting them along the roots. Wisdom teeth do not have problems because they are close to the angle of the lower jaw and there are strong cortical plates there. When I talked about thin vestibular walls, this comparison refers to the aesthetic zone of the smile, to the frontal group of teeth, including the premolars:
.
Prevention of receding gums
To prevent gum recession, your doctor may recommend the following measures:
- Timely, regular visits to the dentist: it is important not only to undergo an examination, but also to carry out professional hygiene twice a year. This will prevent the accumulation of plaque and the formation of hard deposits.
- Timely correction of bite, treatment of inflammatory gum diseases, replacement of fillings, careful selection of orthopedic structures.
- Individual selection of oral hygiene products, especially in the presence of periodontal tissue diseases.
- Using dental floss and irrigator. It will not only improve the quality of hygiene and help remove food particles from the interdental spaces, but will also serve as a kind of gum massager, stimulate blood circulation and maintain the health of the mucous membranes. It is important to consult a doctor about the advisability of use, however, modern irrigators provide mild modes of exposure.
- Avoiding mucosal injuries: avoiding uncomfortable orthopedic structures, using special wax when wearing braces.
- Quitting smoking: this bad habit impairs the blood supply to the tissues of the oral cavity and contributes to the formation of a large amount of plaque on the teeth.
You can learn more about treatment and prevention, as well as get quality help if you have gum recession, from the doctors at the STOMA clinics. Experienced periodontists are highly qualified and have a whole arsenal of modern treatment methods: we are ready to offer comprehensive assistance in diagnosis and treatment. You can make an appointment by phone or through a special form on the website.
What the patient needs to understand before root removal
You need to assess the health risks, you need to talk to the attending surgeon, find out about his experience. Quite often, tooth root removal is carried out, unfortunately, with the following negative consequences:
- gums are torn
- fractured bony vestibular plate
Sometimes when visiting such patients, you get the feeling that the tooth was not removed, but knocked out with something. There were cases when a patient’s extraction began in some clinic, and there, in the middle of the patient’s appointment, the doctor announced that he was unable to remove it, and the patients came to us in this form to remove the root of a tooth that was already in the extraction stage.
When removing the roots of wisdom teeth, you may face risks such as jaw fracture. One of the common risks of removing the roots of 3 molars is damage to the mandibular nerve
, leading to cuts and numbness in areas of the jaw. There is a risk of damaging the artery on the lingual side.
If, when a tooth is removed, a root or part of it is left behind, what should you do?
According to Russian treatment standards, the tooth root cannot be left during extraction. That is, if the patient was left with a root or part of it during removal, then this is considered a poorly performed surgical procedure.
In European countries there are doctors who agree that if there is no inflammation on the tooth and if the root part is not infected, and removal of the root leads to trauma, then only the cortical part of the root is removed, and the other part remains in the bone.
If the patient is left with a part of the root that is infected, then this is a problem. A cyst may develop and inflammation may develop. If the apical part was not infected, then everything heals and does not bring any trouble to the patient.
Tooth root without crown part
Can a tooth root without a crown cause inflammation in the gums or bone? Of course it can. There is a canal at the root of the tooth; if this canal is infected, then the problem will develop into a negative prognosis.
Inflammation, suppuration, periostitis, osteomyelitis - diseases can develop due to an infected tooth root. And the source of infection at the root must be removed; if it is impossible to remove the infection and preserve the root, then it must be removed.
Hypertrophic pulpitis
Overgrowth of gum tissue is a serious pathology that requires immediate attention to a dental clinic.
The gum comes out of the tooth often with advanced hypertrophic pulpitis, which occurs in two possible chronic forms:
- Excessive volume of soft tissue is formed due to the granulation process. The development of the process is preceded by the presence of a huge carious hole over a long period of time. Due to its presence, soft structures are constantly injured, transmitting irritation to the pulp.
- A dense polyp forms in the pulp area due to the growth and layering of flesh on top.
The disease is mostly asymptomatic. And only eating rough food provokes aching pain. The gums in the problem area may also bleed. But the main sign of hypertrophic pulpitis is the appearance of “wild meat” in the hole of the dental unit. Over time, it grows so much that it fills the entire cavity and goes beyond its limits. Pain and discomfort interfere with proper hygienic care. Aggressive microflora contributes to halitosis (bad breath).
Swelling of the mucous membrane due to traumatic or deep carious destruction of the crown
Gum receding occurs when the walls of the tooth are completely or almost completely destroyed. It becomes inflamed due to constant injury and accumulation of food particles. Plaque thickens over time, puts pressure on the gums, and populates it with pathogenic microflora. The proliferation of aggressive microorganisms contributes to the development of swelling and hyperemia. The gums increase in volume and it seems that meat is sticking out of the cavity of the dental unit. The patient experiences pain and severe burning when eating salty and sour foods. The jaw row reacts sharply not only to taste, but also to temperature stimuli. There is discomfort from hot/cold.
Is implantation possible after tooth root removal?
Yes, of course it is possible. And we at the clinics of the German Implantology Center widely use implantation after tooth root removal. Our conditions allow us to carry out implantation in such cases. And if we can achieve primary stability of the implant, then in 90% of cases
After removal, we immediately install the implant. We have rolled out the technology to perfection and gives excellent results.
Of course, with the exception of wisdom teeth, no implant is placed after their removal. But, by the way, wisdom teeth in this situation can be extremely useful, since they... can be transplanted to the place of the problem tooth being removed! Dental transplantation has been practiced in the clinics of the German Implantology Center since 2017, and our specialists have accumulated a wealth of clinical experience. Let's talk about this a little more.
An alternative to implantation is autotransplantation of wisdom teeth
Don't rush to remove your wisdom teeth. Firstly
, there must be clear indicators for their removal.
Secondly
, you don’t need to follow fashion, trends and delete eights just because “a girlfriend or friend deleted them and it’s cool.” There are a number of moments in life when wisdom teeth come to our aid.
It is not for nothing that nature has created a number of organs that duplicate each other in our body, for example, we have two lungs, two kidneys, which in case of problems with one lung/kidney come to our aid. Also with wisdom teeth: if a person (for some reason) has problems with the chewing group of teeth, for example, caries has destroyed the sixth or seventh tooth, then eights can come to the rescue. How so? After all, wisdom teeth are not involved in the chewing process. Yes, you are right here. But a wisdom tooth can serve as a donor, and it can be transplanted into place of a tooth with destroyed roots. Fantastic? No, advanced technologies in dentistry. This is called autotransplantation.
In the following video we show in detail the dental transplant surgery. The roots of two sixths of the patient's teeth had just been destroyed, and they were replaced by the patient's own wisdom teeth. And, by the way, this patient at the end of the video gives a detailed review after 1 year after the operation. Look, this is useful:
Features of treatment of gum recession
There are conservative and surgical methods, with the help of which it is possible to cope with the problem relatively quickly. The development of a treatment program is always individual and takes into account the severity, causes of prolapse, prevalence of pathology and other conditions.
The first step is always professional teeth cleaning. It is necessary to remove soft and hard dental plaque. Sometimes subgingival tartar is removed, which already makes it possible to reduce the depth of periodontal pockets, and in combination with other methods, cope with the problem completely or achieve a significant improvement.
Drug treatment can solve several problems at once:
- eliminate or prevent gum inflammation;
- strengthen gums;
- improve blood circulation;
- speed up recovery processes;
- activate the growth of mucosal cells and gum tissue.
For this, vitamin therapy, anti-inflammatory drugs and local antibiotics, self-absorbing membranes, etc. can be used. The doctor may prescribe medicinal baths, rinsing with certain solutions or application of drugs to the gums, including at home.
Preparations that activate recovery processes are also widely used: products based on hyaluronic acid, regenerating gels with growth factors. The launch of natural regeneration processes allows you to literally “grow” the gum in the place where it subsides.
Another conservative method is the use of the patient's own blood plasma enriched with platelets. This method is called plasma lifting, or APRF technology. Injections into the gums can be used, as well as special membranes that are placed under the gums, but as part of a surgical intervention. This allows you to quickly restore tissue and improve cell nutrition.
As for other surgical treatments for receding gums, the most common are:
- Flap surgery - gum recession is closed with a gum flap, which the doctor takes from the patient's own tissue located nearby. Intervention is performed when the gum defect is minor and there is a sufficient amount of surrounding tissue that can be used.
- Transplantation of a graft from the hard palate/tuberculum of the upper jaw. In this case, part of the gum or a flap of connective tissue is taken from the donor sites and planted in the defect area. Can be used for all types of recession.
- Combined method: the movement of gum tissue is combined with the collection of tissue from the hard palate. The combination of approaches makes it possible to obtain high aesthetic results and close deep recessions. However, if gum loss is more than 5 mm, multiple interventions may be required.
Closure of gum recession is performed on an outpatient basis under local anesthesia. The choice of type of operation is determined by the condition of periodontal tissues and diagnostic results. All surgical methods are often combined with curettage - cleaning the space under the gum and removing subgingival deposits, and are also supplemented with growth activators.