Causes and risk factors
The mucous membrane of the child's oral cavity is often injured. The appearance of ulcers can be caused by temperature effects (hot food and drinks), biting the inner surface of the cheeks or lips; damage by sharp edges of the filling, braces or the tooth’s own tissues in case of chipped enamel. Normally, the immune response allows the pathological process to be quickly eliminated, the mucous membrane heals, and bacteria do not have time to cause severe inflammation and ulceration.
Weakened children's immunity cannot cope with this task, which leads to the development of aphthous stomatitis. A small number of opportunistic bacteria that populate the oral cavity begin to actively multiply. Often the disease occurs against the background or as a result of a severe infection: influenza, ARVI, acute tonsillitis, infectious mononucleosis, etc.
Main risk factors:
- food allergies, allergic reactions to hygiene products, such as toothpaste;
- deficiency of vitamins and microelements due to a strict diet or impaired digestion of food;
- hereditary predisposition;
- foci of infection in the oral cavity: caries, chronic periodontitis, periodontitis, gingivitis;
- frequent respiratory diseases;
- severe systemic diseases: pathologies of the endocrine system, blood vessels, metabolic disorders, etc.
Ask a Question
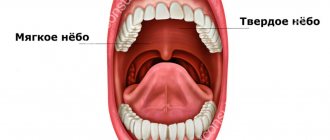
Other reasons for the appearance of red dots in the sky
In addition to stomatitis, there are many diseases that manifest themselves as small rashes on the oral mucosa:
- ARVI (acute respiratory viral infections). This is a rare case, but if the patient suffers from a runny nose and is forced to breathe through the mouth, then excessive dryness of the mucous membrane leads to the appearance of a small red rash.
- Herpetic sore throat. A characteristic symptom of this pathology are vesicles - formed bubbles with white contents. Over time, they burst and painful ulcers form in their place. Vesicles spread throughout the oral mucosa, so red dots on the palate may be the primary symptom of the disease. Additionally, the patient complains of severe sore throat, high body temperature, and enlarged regional lymph nodes.
- Diseases of the cardiovascular system. High blood pressure and fragility of blood vessels sometimes lead to the formation of small red rashes. And not only on the skin! The periodic appearance of the syndrome in question on the oral mucosa may be accompanied by headache, dizziness, shortness of breath, which means pressure instability. You should contact not only a dentist, but also a cardiologist regarding the problem.
- Allergic reaction. It is difficult to determine what exactly caused the appearance of red dots in the mouth. The fact is that the allergen first accumulates in the body and only after a few days can it manifest itself as symptoms. If you suspect an allergy, you need to examine the whole body: rashes will definitely be present on the elbows, behind the ears, and under the knees.
Adults and children sometimes develop a red rash in the mouth due to cancer with localization of the malignant process in the mouth, vitamin deficiency and tuberculosis. But such causes are recorded extremely rarely, although it is worth undergoing a full examination to exclude serious diseases that occur without typical symptoms.
Forms of the disease
According to the ICD, aphthous stomatitis is assigned code K12.0. There are two forms of the disease - acute and chronic. The second is characterized by frequent relapses and may be a consequence of inadequate or untimely treatment of acute inflammation.
An acute disease is characterized by severe symptoms. It begins quickly, severe pain occurs at the site of mucosal damage, and the child may refuse to eat. In some cases, body temperature rises, weakness and lethargy occur.
The chronic form is characterized by a sluggish course; the child’s general well-being does not suffer. The disease can recur up to several times a year.
A dental disease that causes a red rash in the mouth
Stomatitis is a disease that can cause the formation of red dots on the upper palate. This is an inflammatory process that occurs in the oral mucosa. It can be of fungal, viral or bacterial origin - it all depends on what specific pathogen has penetrated the mucous membrane.
Viral stomatitis
Caused by the herpes virus, small rashes appear not only on the palate, but also on the inside of the cheeks and lips, and tongue. The first two days of illness, the rash remains red and large, and then it transforms into blisters that are filled with serous fluid - clear or cloudy.
Viral stomatitis in each case is accompanied by elevated body temperature, weakness, lack of appetite and pain, a burning sensation in the mouth. This form of the disease is mainly diagnosed in adults and newborns.
Bacterial form of pathology
Most often, the oral mucosa is affected by staphylococcus and streptococcus. It is the latter that is considered the most dangerous, because it provokes various kinds of complications, including general blood poisoning. Bacterial stomatitis in almost every case ends with the development of tonsillitis, tracheitis or pharyngitis.
Red dots appear on the white palate, they never merge, but cause some discomfort to the patient: they itch, there is a burning sensation, the sensitivity of the mucous membrane to hot and cold, sour and salty increases. After a few days, the rash becomes barely noticeable, but the patient’s body temperature rises, and one of the above diseases rapidly develops.
Fungal stomatitis
Most often, the fungus affects the mucous membranes of those people who have weakened immune systems. In an adult, this can happen due to prolonged use of certain medications or a long course of the disease. Children often suffer from fungal stomatitis. “Thrush” develops due to constant licking of toys, pieces of furniture and imperfect immunity due to age.
There are not only red rashes in the mouth, but also a white coating. It is characteristic of this disease and helps to make an accurate diagnosis and prescribe effective treatment. Additional symptoms include pain and burning in the mouth, restlessness in a child, and a feeling of fatigue in an adult.
Symptoms of aphthous stomatitis
The onset of acute aphthous stomatitis in children may resemble ARVI: there is malaise, increased body temperature, and more profuse salivation may appear. The main symptom of the disease is the appearance of ulcers in the mouth: first, a red dot appears on the mucous membrane, which subsequently becomes an ulcer (aphtha) within 2-3 days. Accidental touching causes pain. The child refuses food and hygiene procedures.
Single erosions occur more often, but there are cases of multiple aphthae formed in groups. They usually measure up to several millimeters, but in severe cases the diameter of the ulcer reaches one centimeter. The disease is characterized by the appearance of a bright red rim around the aphthae; a grayish or yellow film-like coating forms on it.
There are also general symptoms that accompany aphthous stomatitis. These include:
- sleep disturbances (due to pain or discomfort);
- decreased appetite;
- pain while talking;
- increased fatigue, lethargy;
- whims, irritability.
Early treatment of aphthous stomatitis in children can prevent complications, shorten recovery time, and prevent further development of the disease.
Features of treatment
To diagnose a disease, only a visual examination is often sufficient, but in some cases laboratory diagnostics are required to determine the causative agent of the inflammatory process and the sensitivity of bacteria to antibiotics. Treatment should be carried out by a dentist, and the treatment regimen is developed individually, taking into account test results, the age and well-being of the child, the causes of the disease, the area of mucosal lesions and other conditions.
If the question of how to treat aphthous stomatitis in children is decided individually, then recommendations regarding eating behavior and hygiene are general for all cases. Such recommendations include the following:
- avoidance of too hot or cold drinks and foods;
- following a hypoallergenic diet;
- refusal of food that irritates the mucous membrane. This list includes fatty, salty and spicy foods, marinades, solid foods;
- adding pureed and soft foods to the menu. This includes cream soups, porridges, pre-boiled meat;
- drinking enough liquid;
- careful adherence to oral hygiene: using brushes with soft bristles, rinsing the mouth after each meal.
Local drug treatment consists of the use of such agents as:
- rinses or irrigation solutions (for children who do not yet know how to rinse their mouths) with an antiseptic effect;
- ointments and gels that stimulate the restoration of mucous membranes;
- drugs for pain relief and burning sensation.
It is important to test the product before use: apply a small amount to the crook of your elbow. If there is no redness, burning, or rash, we can say there is no allergy - the product can be used for treatment.
In some cases, systemic drug therapy is indicated. Your doctor may prescribe antihistamines to combat the allergic reaction and relieve swelling. In order to increase the resistance of the child's body, immunomodulators may be recommended. The decision on the need for antibacterial therapy is made in the case of an extremely severe course of the disease, a persistent increase in body temperature, and identification of a bacterial pathogen in a smear.
Elevated body temperature and pain are indications for symptomatic therapy. The doctor may recommend non-steroidal anti-inflammatory drugs in a dosage and form appropriate to the age of the young patient. Sometimes it is advisable to use suppositories if taking the medicine in the form of a tablet or syrup causes pain or anxiety.
Treatment of infants additionally includes disinfection of toys and teethers that the baby may put in his mouth. A nursing mother should pay attention to breast hygiene: thoroughly wash her breasts after feeding using warm water and special products.
Sometimes it is advisable to use folk remedies. Thus, rinsing the mouth with chamomile can soothe inflamed mucous membranes and speed up the healing process. However, it is important to remember that such prescriptions can only complement the main course of treatment. Don't forget to consult your doctor about the possibility of using them. Some herbs are strong allergens, so it is important to ensure that you are not hypersensitive to them.
Warming, the use of honey and alcohol tinctures are prohibited, as all this can lead to a worsening of the condition and lead to serious complications. It is better not to self-medicate, but to show the child to a qualified specialist.
Treatment of aphthous stomatitis in children usually takes no more than 7–12 days. It all depends on the state of the child’s immune system, the severity of inflammation, the number and depth of ulcers.
Manifestations of diseases of internal organs on the mucous membrane of the mouth, tongue and lips
Diseases of the mucous membrane (MU) of the mouth, tongue and lips are one of the important and complex areas of practical medicine. Patients often find themselves in difficult clinical situations when they receive untimely and inadequate care. The fact that the human body is a complex, hierarchical, dynamically self-governing formation, the stability of which is due to the simultaneous functioning of a number of organs and systems, began to escape the attention of the doctor.
The existing relationships between lesions of the mucous membrane of the mouth, lips, tongue and systemic pathology should alert both patients and dental and somatic doctors. In the medical literature, a large group of tongue diseases are presented that occur separately, without affecting other parts of the oral cavity: desquamative glossitis (“geographical” tongue), black (“hairy”) tongue, folded tongue, rhomboid glossitis [1].
Changes in the condition of the mucous membrane of the mouth and tongue can occur and be detected both before other clinical manifestations of systemic diseases, and simultaneously with them. In many systemic (somatic, general) diseases, the oral mucosa reacts with the appearance of various types of disorders: disorders of tissue trophism, bleeding, swelling, dyskeratosis . Some manifestations of pathology in the mucosa of the mouth and tongue clearly indicate one or another type of organ or systemic disorder and are of great diagnostic value. However, in most cases, despite the different etiology and pathogenesis, the manifestations of systemic diseases on the oral mucosa are not specific in nature and are characterized by similar, sometimes outwardly identical clinical signs, which creates difficulties in their recognition.
Often occurring lesions of the oral mucosa due to diseases of the gastrointestinal tract, cardiovascular system, endocrine pathology, deficiency of vitamins (especially group B), macro- and microelements can attract the attention of specialists in various fields. Since changes in the mucous membranes of the mouth and tongue can occur and be detected earlier than other clinical manifestations of systemic diseases or simultaneously with them, patients themselves often turn to a dentist. In turn, gastroenterologists, endocrinologists, cardiologists, and hematologists can involve a dentist for consultation and joint supervision of patients with lesions of the oral mucosa, lips and tongue.
In this regard, we consider it necessary to share our clinical observations. This message may be useful to specialists whose professional interests relate to the diagnosis of these diseases and the treatment of such patients. Our previous publications were devoted to these issues [2–10]. The latest report [11] provided data on cancer screening for diseases of the oral mucosa, tongue and lips.
During our many years of clinical practice, changes in the CO of the mouth, tongue and lips were observed in the pathology of various organs and systems of the body, and metabolic disorders. Lesions of the mucous membranes of the mouth, lips and tongue are most often found in diseases of the gastrointestinal tract. In this case, ulcerative, aphthous and necrotizing stomatitis develop. The best studied in this regard are language changes characterized by a number of features:
- coated tongue (Fig. 1), which is detected most often (with exacerbation of gastritis, gastroesophageal reflux disease, peptic ulcer, pancreatitis, enteritis and colitis, the amount of plaque increases);
- swelling of the tongue, diagnosed by tooth marks on its lateral surfaces, usually associated with enteritis and colitis;
- changes in the papillae of the tongue, manifested in the form of hyperplastic and atrophic glossitis;
- desquamation of the epithelium (sometimes in this case they talk about desquamative glossitis (Fig. 2), which some authors regard as an “independent disease of the tongue”);
- paresthesia and disorders of taste sensitivity, often accompanying not only diseases of the digestive system, but also developing as a result of an imbalance of vitamins and pathology of the autonomic nervous system.
Rice.
1. Coated tongue in a patient with chronic pancreatitis in the acute stage. Rice. 2. Desquamative glossitis in an 82-year-old patient suffering from peptic ulcer localized in the pylorus, who underwent radiation therapy for lung cancer and surgery for cancer of the rectosigmoid angle. Damage to the mucous membrane of the mouth, lips and tongue is observed with a deficiency of vitamins and microelements. The most common deficiencies in clinical practice are B vitamins and iron.
Pain, numbness, burning in the tongue, in the gums and lips are observed with hypovitaminosis B12, which is accompanied by neurological disorders and changes in hematopoiesis. Both with iron deficiency anemia and with latent iron deficiency, changes in the CO of the mouth, tongue and lips are caused by manifestations of tissue iron deficiency (sideropenia) . Patients (usually young girls and women) complain of perversion of taste sensitivity, paresthesia, burning of the tongue, pain and swelling in the tongue, sometimes difficulty swallowing dry and solid food, and choking. With severe sideropenia, the tongue, due to atrophy of the filiform and mushroom-shaped papillae, becomes smooth (“polished”, “varnished”), angular cheilitis develops, folds on the back of the tongue and trophic changes in the mouth are sometimes observed. It should be remembered that the appearance of symptoms of sideropenia often precedes a decrease in hemoglobin levels and can persist even after correction of anemia if iron therapy is insufficient.
Pain, numbness and burning in the tongue, in the gums, lips are observed with hypovitaminosis B12, which is accompanied by neurological disorders and changes in hematopoiesis (B12-deficiency anemia), so the mucus of the mouth is pale. Bright red areas of inflammation appear on the tongue, reacting to the intake of acidic foods and medications. These lesions are often localized along the edges and at the tip of the tongue, sometimes involving the entire tongue (“scalded” tongue) (the so-called Hunter-Meller glossitis). Often ulcerations and petechiae develop on the tongue. Such changes can spread to the gums, mucous membranes of the cheeks, soft palate, and less commonly to the mucous membranes of the pharynx and esophagus. Subsequently, the inflammatory phenomena subside, and the papillae of the tongue atrophy. The tongue becomes smooth and shiny (“varnished” tongue; Fig. 3).
Rice. 3. “Lacquered” tongue in a patient with B12-deficiency anemia.
With relapses of the disease, along with atrophic changes, hyperplasia of the papillae at the root of the tongue develops (hypertrophic papillitis). At the same time, leukokeratosis of the tongue and lip mucosa may be observed.
Vitamin B1 deficiency is accompanied by hyperplasia of the fungiform papillae of the tongue, paresthesia and allergic reactions of the oral mucosa. Hypovitaminosis B2 is manifested by a peculiar change in the skin, red border of the lips, mucous membrane in the corners of the mouth (angular stomatitis), oozing, maceration of the epithelium. A superficial form of desquamative glossitis is noted (triad: dermatitis, cheilitis, glossitis). With hypovitaminosis B6, symptoms of a disorder of the nervous system (polyneuritis) and the gastrointestinal tract, angular stomatitis, cheilitis, and glossitis are observed.
Lesions of the oral mucosa in diseases of the cardiovascular system are observed in more than half of patients with this pathology, in which the following are detected:
- swelling and cyanosis of the mouth and lips; in case of myocardial infarction, swelling of the tongue may be accompanied by the appearance of erosions, ulcers and “cracks”;
- vesical-vascular syndrome - the appearance (usually in older women suffering from arterial hypertension) of dense blisters (after opening, erosions form) with hemorrhagic contents on the mucous membrane of the soft palate, the lateral surfaces of the tongue, and the cheeks. It is necessary to differentiate this syndrome from pemphigus and erythema multiforme;
- ulcerative-necrotic lesions of the mouth with the formation of trophic ulcers in the absence of a pronounced inflammatory reaction in the surrounding tissues. We observed a patient with necrosis and sequestration of the body and branch of the mandible. These lesions must be differentiated from: traumatic ulcers, malignant tumors, Vincent's ulcerative necrotizing stomatitis, necrotic lesions of the mouth due to blood diseases.
The most common endocrine pathology in dentist practice is diabetes mellitus. There is a direct relationship between the severity of inflammatory changes in the oral mucosa and the course of the disease, its duration and the age of the patient. With a short duration of diabetes, the oral mucosa becomes hyperemic, swollen, and bleeds. With increasing duration of the disease, hyperkeratosis of filiform papillae and hyperplasia of fungiform papillae most often develop. The tongue is coated; hyperemic mushroom-shaped papillae in the form of reddish dots rise along the entire back of it.
The dentist is responsible for diagnosing the early manifestations of “general” diseases, conducting a thorough examination of the patient through the efforts of somatic doctors. Folding and an increase in the size of the tongue are often noted; a combination of tongue folding with hyperkeratosis of the filiform papillae or, conversely, with their desquamation (diffuse or focal) and dryness of the mucous membrane of the tongue is possible. There is a “geographical” language. Teeth imprints are identified on the lateral surface of the tongue. With decompensation of diabetes, decubital ulcers are possible and in almost all patients changes in the lips are detected: dry mouth and red border of the lips in combination with cracks, jams, crusts, bright hyperemia, especially pronounced in the Klein zone, angular cheilitis. In the diabetes compensation phase, dry mouth and angular cheilitis disappear.
Changes in the CO of the tongue are more stable, remaining in the phase of decompensation and compensation. Oral candidiasis often develops.
Basics of medical tactics for lesions of the mouth, lips and tongue:
- For rational treatment of diseases of the mouth, lips and tongue, a thorough examination of the patient and contact between the dentist and other specialists is required, first of all, with the therapist, as well as specialized specialists - gastroenterologist, endocrinologist, hematologist, cardiologist.
- An axiom for the dentist should be the elimination of all unfavorable irritating factors in the oral cavity in the patient, which can support and provoke the development of the pathological process. It is unacceptable to use the so-called cauterizing agents and long-term use of the same mouthwashes.
- Treatment of diseases of the oral mucosa must be carried out in compliance with the principles of bioethics; these diseases must be considered from the standpoint of the state of the whole organism, therefore, in most cases, one cannot limit oneself only to local effects on the lesions of the mucous membrane carried out by the dentist.
- Treatment should begin only after at least a preliminary diagnosis has been established and meet the following requirements:
- be comprehensive;
- provide a pathogenetic approach;
- do not violate the anatomical and physiological properties of oral mucosa;
- eliminate the pain factor;
- help optimize the epithelization of lesions;
- provide for the active involvement of the patient in performing medical procedures at home.
In some diseases, changes in the color and general appearance of the oral mucosa and surface of the tongue do not have independent diagnostic significance. However, in combination with other symptoms, the appearance of the lips, tongue, and oral mucosa can help clarify the diagnosis. The prognostic significance of changes in organs and tissues of the oral cavity is great. The dentist is responsible for recognizing and diagnosing early manifestations of “general” diseases and conducting a thorough examination of the patient through the efforts of somatic doctors. We are confident that timely and correct assessment of the described conditions in the practice of doctors of other specialties is very necessary and advisable.
Literature
- Danilevsky N. F., Leontyev V. K., Nesin A. F., Rakhniy Zh. I. Diseases of the oral mucosa. - M.: OJSC "Dentistry". — 271 p.
- Tsepov L. M., Mikheeva E. A., Nesterova M. M. Erosive and ulcerative lesions of the mucous membrane of the mouth, tongue and lips. Tactics of a dentist // Dental South. - 2009. - No. 8 (68). — P. 10-13.
- Tsepov L.M., Nikolaev A.I., Petrova E.V. et al. Symmetrical recurrent decubital ulcers of the mucous membrane of the lower lip in a patient with facial paraspasm // Dental South. - 2007. - No. 7 (56). — P. 28-29.
- Tsepov L. M., Tsepova E. L. Diagnostic value of changes in the lips, oral mucosa and tongue in various diseases and pathological conditions // Dental South. - 2010. - No. 6. - P. 14-16.
A complete list of references is in the editorial office.
Prevention
The development of the disease can be prevented with the help of general strengthening measures: it is important to adhere to a daily routine, provide nutrition taking into account the body’s needs for vitamins and minerals, and pay attention to the prevention of infectious diseases.
The development of stomatitis can be avoided using simple measures, such as:
- regular oral hygiene, which should begin from the moment the baby’s first tooth appears;
- use of toothpastes without sodium lauryl sulfate. This component increases the risk of developing the disease;
- routine examinations by a pediatric dentist;
- rinsing the mouth after every meal;
- limited consumption of sweets.
Pediatric dentists at STOMA clinics are ready to help a child of any age. By contacting us, you can be confident in the professionalism of our specialists. We have developed effective treatment regimens for aphthous stomatitis in children. Doctors will talk in detail about preventing relapses and give recommendations on maintaining oral health.