Infiltration anesthesia is a type of local anesthesia most common in dental practice. It is this type of pain relief that patients call “freezing.”
Local infiltration anesthesia acts exactly in the area where it was injected. After the injection, all nerve impulses are blocked in this place, the patient does not experience pain or discomfort during dental procedures. At the Left Bank Dental Clinic, infiltration dental anesthesia is used only when necessary and there are no contraindications.
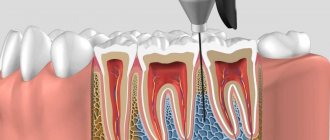
Operating principle of infiltration anesthesia
Infiltration anesthesia is one of the methods of pain relief.
It involves the introduction of an anesthetic into the skin or mucous membrane, as a result of which nerve impulses are blocked. This type of pain relief is known as “freezing.” The drug used by the doctor suppresses the nerve impulse that goes from the pulp to the brain. Therefore, the patient loses sensation in some parts of the face or mouth, such as the cheek, lip or tongue. Numbness occurs in the part of the face where the anesthetic is injected. The anesthetic is administered by injection. First, the drug enters a certain area under the skin, and then is distributed among the cells. The maximum duration of the anesthetic dose is one hour. Gradually the medication breaks down and sensitivity returns. If necessary, another dose of the drug may be administered. The anesthesia process is under the supervision of a specialist.
Distinctive features of infiltration anesthesia
Infiltration anesthesia differs from other methods of pain relief by its immediate action and the exact duration of the analgesic effect. The components of the drug are very quickly eliminated from the body and do not have a negative effect on it. Infiltration anesthesia is also characterized by a low concentration of medications used.
Indications for the use of infiltration anesthesia in dentistry
- Treatment of dental diseases (caries, pulpitis, periodontal inflammation).
- Surgical treatment of periodontal diseases (curettage, gum plastic surgery, elimination of defects and tissue regeneration).
- Dental prosthetics without pulp removal (installation of crowns, inlays, bridge structures).
- Treatment with surgical intervention (tooth extraction, implantation, tissue expansion, emptying of purulent cavities, opening of phlegmons, excision of cysts).
Contraindications
- An allergic reaction to a pain reliever.
- Mental disorders of the patient that prevent constructive communication with him.
- Excessive psychomotor agitation.
- Children under 10 years of age (relative contraindication).
- Asthma and other pathologies of the respiratory system.
- Using muscle relaxants to relax muscles.
- The presence of scars on the mucous membranes of the oral cavity, which prevent the uniform distribution of the drug.
- Inflammatory or purulent process in the area of anesthetic administration.
- The presence of malignant neoplasms or tumors suspected of cancer.
- Refusal of the patient to use this method of anesthesia.
Types of infiltration anesthesia
- Straight. The area of tissue where the anesthetic was directly injected loses sensitivity.
- Indirect. The drug disperses throughout the surrounding tissues and has an analgesic effect on a wider area.
Drugs used
For infiltration anesthesia, special drugs are used in low concentrations. These include:
- Lidocaine.
- Novocaine.
- Procaine.
- Ultracaine.
More effective, but also more toxic anesthetic drugs include:
- Bupivacaine.
- Tetracaine.
- Ropivacaine.
Adrenaline can be used to enhance the effect of the painkiller. It promotes vasoconstriction and prevents the anesthetic from entering the blood.
When infiltrating anesthesia, specialists adhere to the principle of using sufficiently large volumes of solutions with low concentrations. This makes pain relief safe for the patient. For anesthesia, a 0.25-0.5% solution is diluted with novocaine or lidocaine. This concentration allows you to administer up to 400 ml of the product.
Infiltration anesthesia according to A.V. Vishnevsky
Premedication, consisting of 2 ml of a 2% solution of promedol, 2 ml of a 1% solution of diphenhydramine and 0.5 ml of a 0.1% solution of atropine, is prescribed 30-40 minutes before surgery.
To perform local anesthesia correctly, certain conditions must be met.
The patient is placed on the operating table in the most comfortable position for the surgeon and the patient. For anesthesia, 2 syringes are needed: 5-10 ml with a hypodermic needle and 10-20 ml with a longer and thicker needle. A 0.25 or 0.5% solution of novocaine (preferably heated) or a solution of trimecaine is used as a local anesthetic. In this dilution, novocaine has minimal toxicity, and, therefore, it can be used in much larger quantities.
The effectiveness of local anesthesia depends on the quality of skin anesthesia. A solution of novocaine or trimecaine is injected intradermally with a 5 ml syringe along the entire length of the intended incision, thereby forming a skin nodule, which surgeons call “lemon peel”. The initial stage of intradermal administration of novocaine (the first injection) is painful, and the patient should be warned about this. Good skin infiltration provides a reliable and long-lasting analgesic effect. When a “lemon peel” forms, injections should be made as few as possible, passing a thin needle intradermally as far as possible along its entire length and applying a novocaine solution to it. Each subsequent injection is made into the edge of the “lemon peel” so that the patient does not experience additional pain from the injections.
After the end of skin anesthesia, it is necessary to change the syringe and continue injecting novocaine or trimecaine with a longer needle into the subcutaneous tissue. The subcutaneous fat layer does not contain very many pain receptors, and therefore very large quantities of local anesthetic should not be injected here, which will then flow into the wound after the incision, interfering with the surgeon’s work.
After completing the infiltration of subcutaneous fatty tissue, you should, changing the needle to a longer one, carefully inject a local anesthetic directly under the aponeurosis, also along the entire length of the intended incision. This achieves tight infiltration of the cellular space, which, firstly, leads to effective anesthesia and, secondly, separates the aponeurosis from the underlying tissues. The need to inject a local anesthetic under the aponeurosis at this stage of the operation is due to the fact that it takes some time (5-10 minutes) for the analgesic effect to develop.
Advantages of infiltration anesthesia
- This type of anesthesia is safe, as it allows the use of solutions in low concentrations.
- The effect of infiltration anesthesia is much faster than conduction anesthesia.
- The area where the anesthetic is administered loses sensation for a long period of time.
- It is possible to administer an additional dose of the drug if long-term treatment is necessary.
- The anesthetic drug is very easily eliminated from the body in a short time.
- Loss of sensation occurs not only in the nerve into which the anesthetic was injected, but also in neighboring nerves.
Pros and cons of infiltration anesthesia
| Pros: | Minuses: |
|
|
Technology of infiltration anesthesia behavior
- First, the area where the drug is administered is treated with an antiseptic.
- The doctor takes a comfortable position near the patient (on his right side).
- The doctor exposes the working area of the mouth by pulling back the cheek or lip. This action can be performed by hand or with a special tool.
- The specialist places the tip of the needle on the transitional fold, maintaining an inclination angle of 45° (relative to the alveolar ridge). The cut of the needle should be directed towards the jawbone.
- Next, the doctor carefully inserts the needle until it touches the bone tissue. The immersion depth can be 5-15 mm, depending on the jaw area.
- The anesthetic is smoothly injected from a syringe into the tissues of the oral cavity.
Reviews about our dental therapists
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
Possible complications and precautions
Despite the fact that infiltration anesthesia is widely used not only in dentistry, this method of pain relief sometimes causes complications:
- Hematoma, which may appear due to damage to a vessel by a needle.
- Rupture of dental ligaments or tooth deviation. This complication is a consequence of too rapid administration of the drug. To avoid such a pathology, it is necessary to observe the rate of administration of the anesthetic, which is 1 ml/15 seconds.
- Trauma to the nerve trunk, which provokes the development of traumatic neuritis.
- Periosteum injury. This complication is accompanied by pain and swelling.
- Development of infectious inflammation. The reason for this is usually the use of unsterile instruments.
- Injury to the muscle tissue located in the infratemporal fossa.
- Paralysis of facial nerve fibers. This condition goes away on its own within a few hours. With this complication, the lip may sag and eye reflexes may be absent.
- Poisoning of the body. The cause of intoxication is too large a volume of injected anesthetic solution or its injection into a blood vessel.
- Allergy. Manifests itself in the form of redness of the mucous membrane, swelling, and difficulty breathing.
In order to avoid complications of infiltration anesthesia, it is necessary to follow a number of rules:
- Conduct preliminary testing of the anesthetic to determine an allergic reaction.
- The dose of the administered anesthetic drug must correspond to the norm specified in the instructions. If the anesthetic does not have an effect, you need to replace it with another similar medication.
- Study contraindications to infiltration anesthesia and the drug used.
- When administering the anesthetic, do not make sudden movements so as not to injure the soft tissues.
- If you are afraid of the needle, you can use preliminary application anesthesia. Before making the injection, the doctor will treat the area of the mucous membrane with an anesthetic gel.
- In order to prevent the needle from entering a large vessel, the doctor pulls the syringe plunger towards himself. If blood appears in the syringe, this indicates an error. In such a situation, the specialist moves the needle to another place.
In order not to encounter the unpleasant consequences of infiltration anesthesia, you need to seriously approach the issue of choosing a clinic and specialist. After all, it is due to medical errors that most complications arise. In our clinic they are extremely rare. We are proud of the level of training of our specialists and invite you to undergo safe treatment in a comfortable environment.
The name of Alexander Vasilyevich Vishnevsky is rightfully inscribed in golden letters in the history of domestic surgery and is immortalized in the name of the oldest surgical institute in our country. This name is associated with the emergence and development of a large surgical school, originating from his conceptual method of local anesthesia - “tight creeping infiltrate”, therapeutic novocaine blockades and the doctrine he created about nerve trophism in surgery. And although the name of this once very relevant area of domestic medicine sounds archaic today, many of its provisions still have their way into the science and practice of surgery. Finally, based on this teaching A.V. Vishnevsky developed a harmonious and logical system of wound treatment, many of the provisions of which are still relevant today.
Unfortunately, modern surgeons often encounter this name only on the pages of surgical textbooks and have little idea of its place in domestic surgery.
The path to surgery
A.V. Vishnevsky was born on August 23 (September 4), 1874 in the Chir-Yurt tract in Dagestan, where his father served in the 82nd Infantry Regiment. Having graduated with honors from the Faculty of Medicine of Kazan University in 1899, in November 1903 Alexander defended his doctoral dissertation in physiology[], while simultaneously working as a surgeon in the city Alexander Hospital and as a dissector at the anatomical departments of the university. In 1904-1909 privat-docent A.V. Vishnevsky, continuing to operate, taught at the departments of normal and topographic anatomy, taught a course in operative surgery, and worked in a microbiological laboratory.
Having received such versatile basic knowledge, the young surgeon went to Germany (1904) and France (1908-1909), where he mastered urology and brain surgery, which were poorly developed in Russia in those years. Returning to his homeland in 1910, A.V. Vishnevsky again began surgical activities, this time in a neurological clinic, where he began to perform complex interventions on the brain. Thus, through anatomy, physiology and microbiology, his path to major surgery began.
"Russian" method of anesthesia
A.V. Vishnevsky made contributions to many areas of domestic surgery - the brain, abdominal and thoracic organs, urinary and biliary tracts, in the fight against shock and in the treatment of wounds, but his method of local anesthesia, which is called the Russian method of anesthesia throughout the world, became the most famous. Let us briefly recall its background.
In 1912 A.V. Vishnevsky headed the department of surgical pathology (general surgery) of Kazan University, and during the First World War he simultaneously worked as a surgeon in military hospitals in Kazan. In 1916, he was elected to the department of hospital surgery at the university, where A.V. Vishnevsky began to develop biliary tract surgery.
By the early 20s of the last century, several methods of blocking pain sensitivity were proposed, but all of them were either technically complex or ineffective, especially for diseases of the liver and biliary tract. As A.V. recalled Vishnevsky’s desire to help patients with obstructive jaundice, eliminating the widespread and deadly chloroform anesthesia for them, led him to the idea of creating a universal method that combined conduction and infiltration anesthesia. His method was based on the principle of self-propagation of a heated 0.25% solution of novocaine through the fascial sheaths to the nerve trunks, the excess of which (an important part of the method!) flowed out during the incision. The surgeon, operating alternately with a syringe and scalpel, did not have to wait for the onset of anesthesia, nor search for the nerve with a needle, given the variability of its location.
The first message about his method, which he called “tight creeping infiltrate,” A.V. Vishnevsky did this at the XVII Congress of Russian Surgeons in 1925, when he reported on 22 successful operations on the biliary tract under local anesthesia. In addition to complete anesthesia, the method allowed for hydraulic tissue preparation.
The data on the surgical activity of the hospital surgery clinic of Kazan University for 1928 are indicative: 96 appendectomies, 29 gastric resections, 3 intestinal resections, 16 operations on the biliary tract, 30 hernia repairs, 9 nephrectomies, 12 nephropexies, operations on the brain and spinal cord, lungs and esophagus . At the same time, most interventions by A.V. Vishnevsky performed the procedure under local anesthesia using his own method. And this at a time when almost all major surgeons of the USSR, headed by S.P. Fedorov[] were categorically against “the presence of the patient at the operation.” There was also a categorical ban on injecting local anesthetics into inflamed tissues and around tumors, as well as the danger of poisoning when injecting them (cocaine) in large doses.
To use A.V.’s method, repeatedly tested by him, in wide clinical practice. Vishnevsky proposed in the late 20s - early 30s, publishing in 1929 in the Kazan Medical Journal the article “My method of local anesthesia for operations in the abdominal cavity,” and in 1932 publishing the monograph “Local anesthesia using the method of creeping infiltrate "
In 1929, at the invitation of the dean of the medical faculty of the University of Iowa A.V. Vishnevsky visited the USA, where he gave a presentation on his method, called “Russian”. By the mid-30s, the clinic had experience of almost 10,000 operations under anesthesia with creeping infiltrate, including interventions on the lungs, esophagus, stomach, liver, bile ducts, intestines, kidneys, including such unique operations as today, such as combined nephropexy, cholecystectomy and appendectomy through one incision, two-stage extirpation of the rectum for cancer, resection of the entire colon for ulcerative colitis, resection of the esophagus for cancer from a posterior extrapleural approach, etc.
Many of these operations are performed under local anesthesia A.V. Vishnevsky produced the first in the world. And this at a time when he was criticized for using local anesthesia for a routine (for him) cholecystectomy!
It should be noted that venerable surgeons criticized, and their rural colleagues, who knew more than others the imperfections of mask anesthesia and were sometimes forced to limit their operational activity to outpatient surgery all their lives, were on his side. "Method of Prof. A.V. Vishnevsky allows you to calmly carry out any major operation... which creates the opportunity for surgeons to quickly master the technique of practical surgery and provide qualified assistance in the periphery,” wrote rural surgeon M.Kh. in 1934. Shalunov. “There is essentially no area where it would be impossible, using A.V.’s method. Vishnevsky, operating painlessly... The method brought major surgery out of the walls of clinics and large hospitals into small hospitals in the periphery,” echoed a colleague in 1937, former zemstvo surgeon Professor BC Levit.
Today we can evaluate in different ways the contribution made to Russian surgery by A.V. Vishnevsky and his followers developed and implemented a “creeping infiltration”. Thus, there is an opinion that the method has slowed down the development of endotracheal anesthesia and, as a consequence, thoracic surgery in our country, but this is not so. The first pneumonectomy for lung cancer A.V. Vishnevsky produced it back in 1937, i.e. 10 years earlier than this operation was performed by the country's leading surgeons (V.N. Shamov, A.N. Bakulev, P.A. Kupriyanov, L.K. Bogush, etc.). Why did he succeed? Yes, because, in addition to the anesthesia technique, which he brilliantly mastered, during lung operations A.V. Vishnevsky used the vagosympathetic blockade he developed, which other surgeons did not know.
“The successes of thoracic surgery in the USSR are largely due to the widespread use of local anesthesia,” wrote A.A. in 1949. Vishnevsky (senior). Son A.V. has his own opinion Vishnevsky was justified by his own experience, operating in the 50s under local anesthesia on the lungs and heart (using closed techniques). To critical remarks about the too broad indications for “creeping infiltration,” father and son responded that local anesthesia is indicated where there are contraindications to anesthesia, and its effectiveness depends not on the method as such, but on the surgeon’s ability to use it. After all, most likely, opponents of the method either used it not according to indications, or did not fully master its technique. But the term “krikain”, which they used in print and has survived to this day, did not add to the popularity of the method.
History has put everything in its place. The years of the Great Patriotic War contributed to the recognition of the method used in the clinic in the early 30s. “Based on the creation of A.V. Vishnevsky’s method of pain relief also changed the surgical technique itself, it became more beautiful, gentle, and anatomical,” recalled who worked in Kazan at the beginning of the war under the supervision of A.V. Vishnevsky V.V. Kovanov.
Let us also quote the words of one of the founders and pioneers of Russian anesthesiology, Professor T.M. Darbinyan: “Local anesthesia according to A.V. Vishnevsky played an extremely important role in the development of Soviet surgery. The reason for this lies in the fact that the principle underlying it, paradoxically, is identical to the principle of modern endotracheal anesthesia and consists of a combination of analgesia and the preservation of reflex self-regulation of vital functions. And today, paying tribute to anesthesia, we should not forget that there is no safer method of anesthesia than local anesthesia.”
It is difficult to add anything to these words.
The doctrine of nervous trophism in surgery and the wound treatment system developed by A.V. Vishnevsky
Application of A.V. Vishnevsky novocaine for therapeutic purposes began with the treatment of limb ulcers with spontaneous gangrene at the department of faculty surgery with the clinic of Kazan University, the head of which he was elected in 1926. Based on the neurogenic theory of dystrophies A.D. Speransky[], with whom he began to collaborate in the early 30s, A.V. Vishnevsky proposed a method of turning off the trophic innervation of tissues by blocking the reflex arc of the pathological focus, as a result of which lumbar, presacral, sheath, vagosympathetic blockades and a short novocaine block were introduced into the clinic.
Soon the idea of a complete interruption of nerve impulses during blockade, which was supported by most surgeons, was replaced by the original concept of A.V. Vishnevsky about the nervous regulation of trophic processes under these conditions, and to continue its scientific and clinical development in 1935, he was invited to Moscow, where, on the basis of the Moscow Regional Clinical Institute, he headed the surgical clinic of the All-Union Institute of Experimental Medicine (VIEM) named after. AM Gorky and the Department of Surgery of the Central Research University of Doctors.
In 1937, for an additional effect on the reparative regeneration of damaged tissues, A.V. Vishnevsky suggested another weak irritant - Peruvian balsam emulsified in oil. “If the method of local anesthesia according to A.V. Vishnevsky brought major surgery out of the walls of large clinics into small hospitals in the periphery, then his theory about weak irritation of the nervous system as a healing factor finally brought the doctrine of nervous trophism out of the walls of physiological laboratories into the wide world of practical medicine. This is one of the greatest examples of the unity of theory and practice,” wrote one of A.V.’s students. Vishnevsky professor A.N. Redhead.
The method of treating wounds with an oil-balsamic emulsion, called “Vishnevsky ointment,” was based on the principle of the identity of the biological essence of inflammation and wound healing. Applied after a thorough surgical treatment of the wound, performed under novocaine blockade or local anesthesia, and always for a long time, the emulsion-impregnated bandage had (according to the author) a weak neurotrophic (irritating and stimulating) effect on the wound. After cleansing, the wound was sutured, introducing the same emulsion between the sutures and eliminating the pain reaction with a regional novocaine blockade.
The “ointment” containing tar[], xeroform and castor oil had practically no contraindications and for many years was widely used to treat inflammatory diseases of various etiologies, localization and distribution, including specific ones, such as tuberculosis, especially during the Great Patriotic War.
In 1941-1944. based on the leadership of A.V. Vishnevsky of the VIEM surgical clinic worked at military hospital No. 5002, and the head of the clinic was awarded several awards: the People's Commissariat of Health Prize (for the development and implementation of a “creeping infiltrate”), the Stalin Prize (for the development and implementation of novocaine blockades and oil-balsamic dressing), the Order of the Red Labor Banner and Order of Lenin.
“Our school, having been developing issues of inflammation for many years, came up with ready-made proposals in the field of military field surgery. Many of them received full approval by the GVSU of the Red Army [],” wrote A.V. in 1944. Vishnevsky. It is estimated that every third person wounded during the war received treatment according to A.V. Vishnevsky - local anesthesia (for operations and wound treatment), novocaine block (as an anti-shock and therapeutic agent) or a balsamic dressing (for the treatment of wounds and fractures).
During these years, continuing to study the problem of wound healing, A.V. Vishnevsky was the first to introduce into purulent surgery the concept of active wound treatment, meaning by this the active intervention of the surgeon in the course of the wound process at any stage of its development, directing it in the direction necessary for wound healing. The concept of active treatment also included the primary suture of a traumatic wound and the so-called tampon-free treatment of a sutured wound, when a heated oil-balsamic emulsion was injected with a syringe between its edges (more precisely, between the sutures).
The concept of A.V. is interesting and modern. Vishnevsky about secondary treatment of purulent wounds and reconstructive operations in conditions of purulent infection, i.e. something that from the point of view of surgery of the middle of the last century seemed unacceptable and which is the norm of modern purulent surgery. The author was able to carry out these operations using his “system”, which many other surgeons did not possess.
Based on the dystrophic theory of inflammation, A.V. Vishnevsky came to the idea of the unity of local and general in the pathogenesis of sepsis and put forward a modern-sounding thesis about starting the treatment of sepsis with mandatory surgical sanitation of the primary focus. The same applies to his understanding of the pathogenesis of traumatic and surgical shock. Considering shock as “a complex degenerative process caused by overstimulation of the nervous system,” A.V. Vishnevsky predicted the effectiveness of vagosympathetic blockade not only as an antishock agent, but also as a basic condition in lung and heart surgery.
In 1946, assessing the contribution of A.V. Vishnevsky and his school in military field surgery, head of the GVSU of the Soviet Army E.I. Smirnov wrote: “The huge difference in the results of treatment of penetrating chest wounds during the Patriotic War compared to past wars is explained by the universal recognition and widest use of the vagosympathetic blockade according to Vishnevsky. Along with this, the school A.V. Vishnevsky had a great influence on the treatment of other traumatic injuries and their complications - bones, joints, abdomen...”
Recognition of the merits of A.V. Vishnevsky's achievements in domestic surgery were his election as an academician of the USSR Academy of Medical Sciences (1946), chairman of the Surgical Society of Moscow and the Moscow Region (1946), as well as the creation of a clinic on the basis of his clinic in the building of the former almshouse of P.M. Tretyakov at the Shchipka Institute of Surgery of the USSR Academy of Medical Sciences (1947) and his appointment as director of this institute (1947), which he led until his death.
School A.V. Vishnevsky
Among the students of A.V. Vishnevsky Kazan period of his life and work (1910-1935) S.M. became doctors of medicine and professors. Alekseev, S.I. Voronchikhin, I.V. Domrachev, S.M. Kurbangaleev, I.S. Malinovsky, N.V. Sokolov, S.A. Flerov and I.F. Kharitonov.
Working in Moscow (1935-1948), A.V. Vishnevsky trained professors A.G. Gilman, P.N. Maslova, E.K. Young, G.M. Novikova, B.K. Osipova, S.P. Protopopova, V.I. Pshenichnikova, G.A. Richter, N.F. Rupasova, A.N. Ryzhikh, A.A. Troitsky, V.V. Turbin, as well as his son A.A. Vishnevsky (senior), who became an academician.
Many of these scientists created their own schools, some stood at the origins of new directions in domestic surgery (A.A. Vishnevsky and B.K. Osipov - surgery of heart defects, A.N. Ryzhikh - coloproctology), and six of them (S M. Alekseev, A. A. Vishnevsky, I. V. Domrachev, S. P. Protopopov, A. N. Ryzhikh and N. V. Sokolov) were awarded the title of Honored Scientist of the RSFSR. It is noteworthy that all scientific and pedagogical teams, which at one time were led by A.V. Vishnevsky, was headed by his students: the Department of General Surgery in Kazan - Professor I.F. Kharitonov, faculty - S.M. Alekseev, hospital - N.V. Sokolov, Department of Surgery, CIU doctors - B.K. Osipov, and the son took over from his father’s hands the Institute of Surgery of the USSR Academy of Medical Sciences.
The logical sequence of ideas that led to the creation of his school was described by A.V. himself. Vishnevsky summed it up this way: “During our scientific and practical work, we developed two big problems: local anesthesia and wound treatment. Work on the 1st problem led us to the discovery of the principle of sheath-creeping anesthesia <…>. In turn, this led to the development of various types of novocaine blockade. Work on the 2nd problem led to the discovery of a special system for treating purulently infected wounds with oil antiseptics. The system of wound treatment led to the posing of the question of active wound drainage, which in turn raised the questions of secondary wound treatment, drainage of a closed purulent cavity, layered tamponade, etc. This led to the questions of osteosynthesis in an infected wound, the problem of an amputation stump, economical resection of joints, etc. "The generalization of this material has led us to a special understanding of the emergence and development of a number of diseases as neuro-dystrophic processes"[].
There is an opinion according to which the school of A.V. Vishnevsky should include all surgeons who have ever used local anesthesia, novocaine blockades or wound treatment according to Vishnevsky in practice.
One can argue with this, but let us remember the similar point of view of V.A. Oppel, who wrote about N.I. Pirogov: “His school is all Russian surgery.”
The Vishnevsky dynasty and his memory
Glorious deeds of A.V. Vishnevsky was continued by his son, one of the creators of domestic heart and vascular surgery, Hero of Socialist Labor, Lenin Prize laureate, Academician of the USSR Academy of Medical Sciences Alexander Aleksandrovich Vishnevsky (senior), who headed the Institute of Surgery of the USSR Academy of Medical Sciences from 1948 to 1975. Recently, the third representative of the glorious dynasty, a major thoracic and plastic surgeon, laureate of the USSR State Prize, Professor Alexander Aleksandrovich Vishnevsky (junior), who for a long time headed the thoracic department at this institute, passed away.
The family tradition is continued by his daughter, great-granddaughter A.V. Vishnevsky, thoracic surgeon and doctor of medical sciences Galina Aleksandrovna Vishnevskaya, working at the Russian Scientific Center for Surgery named after. B.V. Petrovsky.
If we remember that the medical career of A.V. Vishnevsky began in 1899, it turns out that the Vishnevsky surgical family has been benefiting their homeland for more than 100 years. Amazing consistency!
Today in the name of A.V. Vishnevsky named the Institute of Surgery of the Ministry of Health of the Russian Federation in Moscow and the multidisciplinary Krutinskaya Central District Hospital in the Omsk region, streets in Kazan (Republic of Tatarstan), Kizil-Yurt, Khasav-Yurt and several villages of Dagestan. Monuments in his honor were erected in Moscow, on the territory of the Institute of Surgery, and in Kazan, at the intersection of L. Tolstoy and A. Butlerov streets.
There is no doubt that the name and deeds of A.V. Vishnevsky is destined to live a long life. His methods have long become classic and are unlikely to ever disappear from the surgical arsenal, and the concept of active and complex treatment of wounds, based on the possibility of a surgeon’s intervention in the wound process at any stage of its development, is fully implemented by the followers of the outstanding surgeon, working as in the institute named after him, and in many surgical clinics in Russia.
[] Vishnevsky A.V. On the issue of peripheral innervation of the rectum: Abstract. dis. ...Dr. med. Sci. Kazan 1904.
[] In 1933, the first Soviet surgeon S.P. Fedorov (1869-1936) was awarded the Order of Lenin, which may indirectly indicate his leadership in domestic surgery.
[] Speransky Alexey Dmitrievich (1888-1961), student of I.P. Pavlova, academician of the USSR Academy of Sciences and Academy of Medical Sciences, creator of the doctrine of nervous trophism in medicine.
[] Initially, the ointment included Peruvian (Peruvian) balm from the bark of the cinchona tree, which was later replaced by cheaper and more accessible tar.
[] Main Military Sanitary Directorate of the Workers' and Peasants' Red Army.
[] The final chapter from the book by A.V. Vishnevsky "Local anesthesia... infiltration." Ed. 4th. Surgery 1949; 5:5-8.