Showing concern for the rights of citizens and remembering that in previous times many citizens were treated not only without asking for their consent, but even actively against their will, the Russian legislator introduced into the field of civil relations such a concept - the patient’s voluntary informed consent to medical intervention . At the same time, of course, the legislator wanted what was best. But it turned out as always.
As a result, this undoubtedly democratic measure often began to be used by very unscrupulous citizens as a way to make money from the legal ignorance of medical workers. And legally trained medical workers began to be forced to invent documents monstrous in bulk and content, from which the patient, already trembling in anticipation of difficult treatment, learned about all sorts of even more unpleasant and often casuistic events that could theoretically happen to him, and was forced to give in your voluntary consent.
As a result, the patient developed a strong conviction that evil was being planned against him in this clinic, and the doctors themselves felt almost like executioners, dooming another victim to death. Of course, it has become very difficult to establish subtle emotional contact between the parties in such a situation. However, since legal requirements exist, dental clinics must comply with them.
Where did the patient's voluntary consent come from?
Fundamental rights in the field of protecting the life and health of citizens are guaranteed by the Constitution of Russia. Article 20 declares the right to life, and articles 22 and 23 confirm the rights of citizens to freedom, personal integrity, as well as privacy, personal and family secrets. These provisions are expanded by Article 21, which states, in particular, that no one can be subjected to medical, scientific or other experiments without voluntary consent.
In furtherance of the right to life, Article 41 of the Constitution provides citizens with the right to health care and medical care. Apparently, in development of these provisions, the legislator introduced two separate articles into another federal act (Fundamentals of the legislation of the Russian Federation on the protection of the health of citizens). Article 32 of the Fundamentals determines that a necessary precondition for medical intervention is the informed voluntary consent of the patient.
Consent must always be given, except in cases where the patient’s condition does not allow him to express his will, and medical intervention is urgent. Then the question of its implementation in the interests of the patient is decided by the consultation, and if it is impossible to assemble a consultation, the attending (duty) doctor directly, with subsequent notification of officials of the medical institution.
Consent to medical intervention in relation to persons under the age of fifteen years, or citizens recognized as legally incompetent, is given by their legal representatives after providing them with information about the health status of such persons, including information about the results of the examination, the presence of a disease, its diagnosis and prognosis, treatment methods, associated risks, possible medical intervention options and their possible consequences. In the absence of legal representatives, such a decision can also be made by a council, and if it is impossible to assemble it, by the attending (duty) doctor.
Article 33 of the Fundamentals simultaneously grants the right to the patient or his legal representative to refuse medical intervention or to demand its termination; however, it establishes that the possible consequences must be explained to the patient or his legal representative in a form understandable to them. Refusal of medical intervention indicating the possible consequences is recorded in the documentation of the medical institution and signed by the patient or his legal representative, as well as a medical professional
If the parents or other legal representatives of a person under the age of fifteen years, or the legal representatives of a person recognized as incompetent in accordance with the procedure established by law, refuse medical care necessary to save the lives of these persons, the medical institution has the right to go to court to protect the interests of these persons.
In addition, a citizen, on the basis of Article 31 of the Fundamentals, can either refuse to receive information about the state of his health (and in this case no one has the right to provide him with this information against his will), or, on the contrary, receive available information about the state of his health, including information about the results of the examination, the presence of the disease, its diagnosis, treatment methods, prognosis, risks, possible options for medical intervention, their consequences and the results of the treatment, as well as directly familiarize himself with the medical documentation reflecting the state of his health , and get advice on it from other medical specialists.
At the patient's request, he is provided with copies of medical documents reflecting his state of health, if they do not affect the interests of a third party. The combination of such contradictory requirements introduces even more confusion into the heads of doctors, which results in completely opposite actions - from drawing up gigantic permitting documents to the complete absence of them. Healthcare workers have no less difficulty defining the concept of “medical intervention.”
The fact is that, using this term itself and establishing requirements for the process of its implementation (obtaining the voluntary informed consent of the patient), neither the legislator nor the relevant federal departments (Ministry of Health, Ministry of Justice) gave an interpretation of what “medical intervention” constitutes. As a result, both representatives and recipients of medical services, as well as other, less desirable participants in their relationships (for example, courts), are forced to turn to international documentation and nomenclature.
In international practice, the definition of the concept of “medical intervention” is used, given in the “Declaration on the Policy of Patient Rights in Europe”, which stands for “any examination, treatment or other action with a preventive, therapeutic or rehabilitative purpose, performed by a doctor or other manufacturer of medical services." This definition is recognized as basic by the World Health Organization (WHO/WH0,1994).
The use of such an interpretation of this concept (and there are no others, as we said, in Russia) leads to the fact that medical intervention means any action performed by a doctor or other medical personnel of the clinic in relation to the patient. As a result, according to Russian legislation, it is required to obtain the patient’s consent for any type of treatment in any clinic, including a dental clinic. What can dentists do in this situation?
All that remains is to act in accordance with the law. Informed voluntary consent to medical intervention or refusal of medical intervention is drawn up in writing, signed by a citizen, one of the parents or another legal representative, a medical professional and contained in the patient’s medical documentation (clause 7 of Article 20 of the Federal Law of November 21, 2011 No. 323- Federal Law of November 21, 2011 “On the fundamentals of protecting the health of citizens in the Russian Federation”).
However, the significance of such consent for the clinic is zero. After all, the clinic strives to satisfy the patient’s right to voluntary informed consent not so much in order to inform the patient in detail, but in order to protect itself from possible claims and their legal consequences associated with violation of legal requirements.
At the same time, the vast majority of patients do not need such complete and detailed information. Some of them believe that by turning to the clinic for help, they have already demonstrated the necessary amount of trust in the doctor and understanding of the need for this or that treatment. Another part of patients simply does not want to receive additional information that may be unpleasant for them. Although, of course, there is a group of patients who are happy to receive any additional information about their health and prospects.
Another thing is that in recent years, situations have increasingly arisen when an unconscious or conscious infringement of a patient’s rights to voluntary informed consent becomes a reason for filing a lawsuit against the offending clinic. And in this case, the lack of written confirmation that the patient received all the necessary information makes all subsequent attempts by the clinic to prove its case completely untenable. In fact, all the voluminous and scattered requirements of the legislator can be reduced to a short text containing a block of specific, succinctly stated questions that imply unambiguous answers.
Patient informed consent model in dentistry
During the conversation prior to the start of treatment, the doctor should explain to the patient:
- that he really has this or that disease;
- name this disease, formulate a diagnosis in a form accessible to the patient, and indicate how such a disease could have ended if the patient had not sought medical help or refused treatment;
- briefly indicate the treatment methods that may be available, and explain in sufficient detail (and again, accessible!) what he is going to do to treat a given disease in a given patient in a specific clinic;
- without going into details, explain what possible complications of treatment this patient may have and why;
- indicate what treatment options for this disease exist for this patient and why the doctor is going to use the chosen option;
- explain what features will accompany the chosen treatment option and what is the expected result upon completion of all treatment measures.
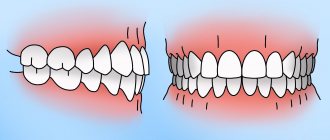
Information for patients planning bite correction (orthodontic treatment)
The patient is aware that:
- Before orthodontic treatment, it is necessary to undergo dental and gum treatment.
- It is necessary to follow ALL recommendations of the orthodontist regarding diet, oral hygiene and physical activity.
- It is necessary to visit your doctor and hygienist on time. The visit schedule established by the doctor can be clarified directly at the appointment or with the clinic administrators by phone.
- It is necessary to urgently visit the attending physician in such cases as the breakdown of the orthodontic apparatus, the breakdown of the arch, the detachment of the bracket, the occurrence of cracks, etc.
- The final stage of orthodontic treatment is wearing retention equipment.
The patient is recommended:
- Consultation with a psychologist (help with long-term treatment) and an osteopath (comprehensive diagnostics).
- Additional dental treatment
in some cases: teeth whitening, dental prosthetics or restoration, dental implantation. The preliminary scope of these procedures is discussed when discussing the treatment plan.
Protocol for voluntary informed consent
These explanations are included in an extremely brief form in the medical records used in this clinic (diagnosis in the formulation according to ICD-10, treatment method, treatment option, treatment plan). After that, a protocol of voluntary informed consent for medical intervention is drawn up and signed with the patient; it is first explained that treatment can begin only after the patient receives satisfactory answers to all questions.
To do this, it is proposed to include in the text of the protocol five questions in the formulations used by the basic legislation of the Russian Federation on the protection of the health of citizens. And the patient is invited to answer them “Yes” or “No” by personally entering the answers into the protocol form, while simultaneously indicating his identifying data - last name, initials, signature, place and date of signing the protocol.
At the same time, the protocol will avoid including unnecessary details and, at the same time, will fully meet the requirements of the legislator - the patient will receive answers to exactly those questions and in the wording required by the legislator, while the patient personally confirms the receipt of satisfactory answers to these questions. It should be noted that the head of the dental clinic must provide two forms of protocol - directly for the patient and for the patient’s legal representative if he is under 15 years of age.
FAQ:
- What is medical intervention? This is any examination, course or other action with a preventive, therapeutic or rehabilitation purpose, performed by a doctor or other provider of medical services.
- What right does a patient have before starting medical intervention? Allow medical intervention to begin only after receiving information from the doctor, giving voluntary informed consent.
- What laws require voluntary informed consent? Fundamentals of the legislation of the Russian Federation on protecting the health of citizens (Articles 31, 32, 33).
- What does the concept of voluntary informed consent include? This is the patient’s consent to begin medical intervention after receiving, in a form accessible to him, available information about the state of his health, including information about the results of the examination, the presence of the disease, treatment methods, the associated risk, its diagnosis and prognosis, possible options for medical intervention and their consequences .
- In what cases does a patient give voluntary informed consent? In all cases when seeking medical help.
- In what form is voluntary informed consent formalized? In a written form.
- What does the protocol for voluntary informed consent of a patient in dentistry include? The patient’s own written answers to the questions: - did the dentist explain to you the information about the presence of the disease? — did he indicate the diagnosis and prognosis of the disease? — did he explain the treatment methods and possible risks? — did he indicate possible options for medical intervention? — did he explain the options for the consequences and results of treatment? — surname, initials and signature of the patient, date and place of signing the protocol.
- With whom is the voluntary informed consent protocol concluded? With the patient or the patient's legal representative.
Information for patients planning dental prosthetics (orthopedic treatment)
The patient is aware that:
- Before dental prosthetics, it is necessary to undergo basic dental treatment : dental treatment, periodontal treatment, bite correction.
- After prosthetics, a period of adaptation begins, i.e. getting used to new denture structures, the duration of which depends on the correct emotional state of the patient and compliance with all medical recommendations.
- Dental implants are the best way to replace missing teeth.
- It is necessary to regularly visit the doctor for preventive purposes and for correction (if necessary) of the denture structure. This increases the service life of the prosthesis.