Why are breastfeeding women afraid to have their teeth treated?
Any step of a nursing mother can affect the health of the child, so before performing the simplest usual actions, she evaluates whether this will harm the baby. When visiting a dentist, three things may cause concern:
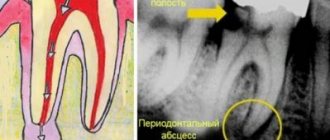
- To make a diagnosis, you may need an x-ray of the diseased tooth;
- During treatment, filling materials and anesthesia medications are used;
- After the procedure, a course of antibiotics may be prescribed.
A young mother may fear that x-rays and medications will make breast milk unsuitable for feeding, and just in case, she may completely refuse dental treatment and postpone going to the doctor until the time when the baby is weaned.
Fluorography and radiography
Fluorography and radiography are methods of radiographic examination. Fluorography is often used for mass, routine screening of tuberculosis.
Nowadays digital fluorography is mainly used . Film fluorography is an outdated research method. Digital fluorography has a lower radiation exposure to a person, but at the same time its resolution (that is, the ability to transmit a real image) is lower in comparison with x-rays of the lungs in direct projection.
X-rays contain more information and pathological changes are more clearly visible.
The radiation exposure is low for both methods (digital devices have lower radiation exposure).
Is it possible to treat teeth during breastfeeding?
If we compare the potential threat from medications used in dental treatment and from pathogenic bacteria in the carious cavity of the tooth, then the latter are much more dangerous for the child. Remember how many times a day a mother kisses her baby, not to mention the fact that she can taste food or drink from baby dishes to make sure they are at normal temperature? The infection will get to the child one way or another. Therefore, treating the teeth of a nursing mother is not only possible, but also absolutely necessary. You just need to warn your doctor about your situation.
If you go to the dentist at the first signs of caries, you can get by with minimal manipulations that do not require x-rays, anesthesia, or antibiotics. In this case, you don’t have to worry at all that dental treatment will somehow affect breast milk, and feed the baby immediately upon returning from the doctor.
X-rays during breastfeeding are also not contraindicated: short-term exposure to X-rays when photographing a diseased tooth will not make milk radioactive and will not harm the baby through breast milk. Moreover, filling materials will not penetrate into the blood and cannot pass into breast milk. And if there is a need for antibiotics, you can choose a medicine that is compatible with breastfeeding.
How to prepare for research
If the procedure is so necessary, then it is better to prepare your body in advance and protect your health using the following actions:
- X-rays should be performed only when necessary, if there are no other ways to identify the cause of the disease or if the risk to the mother’s health is much higher than limiting the baby to breastfeeding for a couple of days. You can feed the baby immediately before the procedure, and then use the expressed reserves. After this time, the mother will be able to continue breastfeeding, and in order to maintain lactation, she needs to express milk after the x-ray and pour it out.
- It is important to make sure that the equipment used for the study is in good working order and whether its service life corresponds to that stated in the documentation.
- When carrying out the procedure, do not neglect a special apron to protect the organs.
- If iodine-containing substances are used, the next feeding of the newborn should be no earlier than 24 hours later.
Anesthesia for dental treatment during breastfeeding. How not to harm a child?
As for anesthesia, there is also no need to endure pain during the procedure.
If the doctor is warned that you are breastfeeding, he will select a drug compatible with breastfeeding. Breastfeeding women should not use painkillers containing adrenaline. Old-generation anesthetics - novocaine, lidocaine, which are practically not used in modern dental practice, can penetrate into breast milk in small quantities.
It is important!
Modern drugs, for example, ultracaine, articaine, are not contraindicated during breastfeeding if used in recommended doses.
Before treatment, check with your doctor what kind of drug he is going to give you, and whether the drug is compatible with breastfeeding.
This article was written to debunk the myth of “dirty/harmful/radioactive” milk after any x-ray examination of a nursing mother.
The article was written by a surgeon, Olga Lipina, with the help and support of her husband (a chemical engineer, a lieutenant in the reserve forces of the chemical, radiation and biological defense forces).
In fact, almost all the information presented here is from a school physics course.
Let's start with an educational program.
X-ray radiation
- electromagnetic waves, the energy of photons of which lies on the scale of electromagnetic waves between ultraviolet radiation and gamma radiation, which corresponds to wavelengths from 10−2 to 103 Å (from 10−12 to 10−7 m).
Biological effects of X-ray radiation
X-ray radiation is ionizing. It affects the tissues of living organisms, the damage is directly proportional to the absorbed dose of radiation. The high penetrating power and energy of X-rays make them quite dangerous for the human body.
As X-rays pass through the human body, they interact with its molecules and ionize them. Simply put, X-rays are capable of “breaking down” complex molecules and atoms of the human body into charged particles and active molecules.
Effects caused by X-rays and other ionizing radiation (such as gamma radiation emitted by radioactive materials) include:
- temporary changes in blood composition after relatively small excess
radiation; - irreversible changes in blood composition (hemolytic anemia) after prolonged excessive
radiation; - increased incidence of cancer (including leukemia);
- faster aging and earlier death;
- the occurrence of cataracts.
As with other types of ionizing radiation, only X-ray radiation of a certain intensity that affects the human body for a sufficiently long period of time is considered dangerous.
The vast majority of medical examinations that use X-ray radiation use low-energy X-rays and irradiate the human body for very short periods of time, and therefore, even when repeated many times, they are considered practically harmless to humans.
The doses of X-ray radiation that are used in a regular X-ray of the chest or bones of the extremities may not cause any immediate side effects and only very slightly (no more than 0.001%) increase the risk of developing cancer in the future.
In the case of X-ray radiation, the radiation carrier is electromagnetic waves, which disappear immediately after the X-ray machine is turned off and are not able to accumulate in the human body, as happens in the case of various radioactive chemicals (for example, radioactive iodine). Due to the fact that the effect of X-ray radiation on the human body ends immediately after completion of the examination, and the rays themselves do not accumulate in the human body and do not lead to the formation of radioactive substances, there are no procedures or therapeutic measures to “remove radiation from the body” after an X-ray no need to carry out.
In the case where the patient was exposed to an examination using radionuclides, you should check with the doctor exactly what substance was used, what is its half-life and how it is eliminated from the body. Based on this information, the doctor will recommend an action plan to remove the radioactive substance from the body. [4]
Immediately after turning off the X-ray machine, both primary and secondary radiation disappear; there is also no residual radiation, which is not always known even to those who are directly involved with it through their work.[5]
About radiation in general
There are 3 types of radiation:
Different types of radiation are accompanied by the release of different amounts of energy and have different penetrating abilities, so they have different effects on the tissues of a living organism (Fig. 2.2).
- Alpha radiation, which is a stream of heavy particles consisting of neutrons and protons, is blocked by, for example, a sheet of paper and is practically unable to penetrate the outer layer of skin formed by dead cells. Therefore, it does not pose a danger until radioactive substances emitting α-particles enter the body through an open wound, with food or with inhaled air; then they become extremely dangerous.
- Beta radiation has greater penetrating ability: it passes into the body tissue to a depth of one to two centimeters.
- The penetrating power of gamma radiation, which travels at the speed of light, is very high: only a thick lead or concrete slab can stop it.
The damage caused in a living organism by radiation will be greater, the more energy it transfers to tissues; The amount of such energy transferred to the body is called the dose.
Radiation exposure doses.
Absorbed dose is the energy of ionizing radiation absorbed by the irradiated body (body tissues), calculated per unit mass.
Equivalent dose is the absorbed dose multiplied by a coefficient that reflects the ability of a given type of radiation to damage body tissue.
Effective equivalent dose is the equivalent dose multiplied by a factor that takes into account the different sensitivity of different tissues to radiation.
The latter indicator takes into account that some parts of the body (organs, tissues) are more sensitive to radiation than others: for example, with the same equivalent dose of radiation, cancer in the lungs is more likely than in the thyroid gland, and irradiation of the gonads is especially dangerous due to the risk genetic damage.
The effective equivalent dose is calculated when conducting any x-ray examination.
Calculation of radiation dose and assessment of the risk of x-ray exposure
Below is a comparison of the effective dose of radiation received during the most commonly used diagnostic procedures using X-rays with the natural radiation to which we are routinely exposed throughout our lives. It should be noted that the doses indicated in the table are approximate and may vary depending on the devices used and examination methods.
| Procedure | Effective radiation dose | Comparable to natural exposure received over a specified period of time |
| Chest X-ray | 0.1 mSv | 10 days |
| Fluorography of the chest | 0.3 mSv | 30 days |
| Computed tomography of the abdominal cavity and pelvis | 10 mSv | 3 years |
| Whole body computed tomography | 10 mSv | 3 years |
| Intravenous pyelography | 3 mSv | 1 year |
| X-ray – upper stomach and small intestine | 8 mSv | 3 years |
| X-ray of the large intestine | 6 mSv | 2 years |
| X-ray of the spine | 1.5 mSv | 6 months |
| X-ray of the bones of the arms or legs | 0.001 mSv | Less than 1 day |
| Computed tomography - head | 2 mSv | 8 months |
| Computed tomography of the spine | 6 mSv | 2 years |
| Myelography | 4 mSv | 16 months |
| Computed tomography of the chest | 7 mSv | 2 years |
| Vaccine cystourethrography | 5-10 years: 1.6 mSv Infant: 0.8 mSv | 6 months 3 months |
| Computed tomography of the skull and paranasal sinuses | 0.6 mSv | 2 months |
| Bone densitometry (determination of bone density) | 0.001 mSv | Less than 1 day |
| Galactography | 0.7 mSv | 3 months |
| Hysterosalpingography | 1 mSv | 4 months |
| Mammography | 0.7 mSv | 3 months |
*1 rem = 10 mSv
[Note – there is a radiologist’s opinion that these doses are overestimated and with modern equipment the radiation exposure rates are much lower. I’ll contact a radiologist I know this week and update him if I learn anything new.]
Taking into account the latest data on the risk of radiation exposure to human health, a quantitative risk assessment is carried out only in the case of receiving a radiation dose above 5 rem (50 mSv) within one year (for adults and children), or in case of receiving a radiation dose above 10 rem over the course of throughout life, in addition to natural exposure.
There is accurate medical evidence regarding the risks associated with high doses of radiation. If the total radiation dose is below 10 rem (including natural and occupational exposure), the risk of harm to health is either too low to be accurately assessed or does not exist at all.
Epidemiological studies among people exposed to relatively high doses of radiation (for example, people who survived the explosion of the atomic bomb in Japan in 1945) have shown no adverse health effects in people exposed to low doses of radiation (less than 10 rem) over many years. years.
More doses for comparison:
- 0.005 mSv = 5 μSv (0.5 mrem) – watching television for three hours every day for a year;
- 10 μSv (0.01 mSv or 1 mrem) – air travel over a distance of 2400 km;
- 1 mSv (100 mrem) – background radiation per year;
- 5 mSv (500 mrem) – permissible exposure of personnel under normal conditions;
- 0.03 Sv (3 rem) – radiation exposure during dental radiography (local);
- 0.05 Sv (5 rem) – permissible exposure of nuclear power plant personnel under normal conditions per year;
- 0.1 Sv (10 rem) – permissible emergency exposure of the population (one-time);
- 0.25 Sv (25 rem) – permissible exposure of personnel (one-time);
- 0.3 Sv (30 rem) – radiation exposure during fluoroscopy of the stomach (local);
- 0.75 Sv (75 rem) – short-term minor change in blood composition;
- 1 Sv (100 rem) – the lowest level of development of mild radiation sickness;
- 4.5 Sv (450 rem) – severe radiation sickness (50% of those exposed die);
- 6 – 7 Sv (600 – 700 rem) or more – a single dose received is considered absolutely lethal. (However, in medical practice there are cases of recovery of patients who received radiation exposure of 6 - 7 Sv (600 - 700 rem)).
The most likely effects at various values of radiation doses and dose rates, related to the whole body:
- 10,000 mSv (10 Sv) - Short-term exposure would cause immediate illness and subsequent death within weeks.
- Between 2000 and 10,000 mSv (2 - 10 Sv) - Short-term exposure would cause acute radiation sickness, likely fatal.
- 1000 mSv (1 Sv) - Short-term exposure would probably cause temporary illness but not death. Because radiation dose accumulates over time, exposure to 1000 mSv would likely result in a risk of cancer many years later.
- 50 mSv/year - The lowest dose rate at which cancer may occur. Radiation doses higher than this increase the risk of cancer.
- 20 mSv/year - Averaged over more than 5 years - the limit for personnel in the nuclear and mining industries.
- 10 mSv/year - The maximum dose rate level received by uranium miners.
- 3 – 5 mSv/year - Typical dose rate received by uranium miners.
- 3 mSv/year - Normal background radiation from natural sources of ionizing radiation, including a dose rate of almost 2 mSv/year from radon in the air. These radiation levels are close to the minimum doses received by all people on the planet.
- 0.3 – 0.6 mSv/year - Typical dose rate range from artificial radiation sources, mainly medical.
- 0.05 mSv/year - The level of background radiation required by safety standards near nuclear power plants. The actual dose near nuclear facilities is much less.
Hygienic standardization of ionizing radiation
Rationing is carried out in accordance with sanitary rules and regulations SanPin 2.6.1.2523-09 “Radiation Safety Standards (NRB-99/2009)”. Dose limits for the equivalent dose are established for the following categories of persons:
- personnel - persons working with man-made radiation sources (group A) or who, due to working conditions, are in the sphere of their influence (group B);
- the entire population, including personnel, outside the scope and conditions of their production activities.
The main dose limits and permissible exposure levels for group B personnel are equal to a quarter of the values for group A personnel.
The effective dose for personnel should not exceed 1000 mSv over a period of working activity (50 years), and for the general population over a lifetime - 70 mSv. Planned increased exposure is allowed only for men over 30 years of age with their voluntary written consent after being informed about the possible radiation doses and health risks.
Some points of the document:
7.9. The established standard for annual preventive radiation exposure during preventive medical X-ray examinations and scientific research of practically healthy individuals is 1 mSv. Preventive examinations using fluoroscopy are not permitted. Conducting scientific research with radiation sources on humans is carried out by decision of the federal health authority. In this case, mandatory written consent of the subject and provision of information about the possible consequences of radiation are required.
7.10. Radiation dose limits for patients for diagnostic purposes are not established. To optimize patient protection measures, it is necessary to comply with the requirements of clause 2.2 of these Rules.
When the accumulated dose of medical diagnostic radiation to a patient reaches 500 mSv, measures must be taken to further limit his radiation exposure if radiation procedures are not dictated by vital indications. When individuals from the population receive an effective radiation dose of more than 200 mSv per year, or an accumulated dose of more than 500 mSv from one of the main sources of radiation, or 1000 mSv from all sources of radiation, a special medical examination is required, organized by health authorities.
7.12. During an X-ray examination, screening of the pelvic area, thyroid gland, eyes and other parts of the body is mandatory, especially in people of reproductive age. In young children, full body shielding should be provided outside of the area being tested.
7.15. When referring women of childbearing age for an x-ray examination, the attending physician and radiologist clarify the time of the last menstruation in order to select the time for the x-ray procedure. X-ray examinations of the gastrointestinal tract, urography, x-rays of the hip joint and other studies related to radiation exposure to the gonads are recommended to be carried out during the first decade of the menstrual cycle.
[Note – in Section 7 – “Requirements for ensuring radiation safety of patients and the public” there is a mention of two groups of patients who need to reduce their exposure to the greatest possible extent – pregnant women and children. There is not a word about breastfeeding women, which indicates that there are no contraindications for X-ray examinations.]
X-ray examinations during breastfeeding.
Any procedures using x-rays (regular x-rays, fluorography, computed tomography) are safe for nursing mothers.
X-rays do not affect the composition of breast milk.
If an X-ray examination is necessary for a nursing mother, there is no need to interrupt breastfeeding or express milk.
In the case of nursing mothers, only X-ray examinations that involve the introduction of radioactive substances into the body (for example, radioactive iodine) pose a certain danger. Before such examinations, nursing mothers should inform doctors about lactation, as some medications used during the examination may pass into the milk. To avoid exposure of the baby to radioactive substances, doctors will likely recommend that the mother stop feeding for a short period of time, depending on the type and amount of radioactive substance (radionuclide) used.
Summary:
The carrier of energy when exposed to X-ray radiation is electromagnetic waves. Yes, they may (or may not) cause some damage at the cellular and subcellular level. The doses received in diagnostic studies are extremely small to cause any significant damage.
These electromagnetic waves act only when the X-ray machine is operating and do not accumulate in the body or anywhere else. Just so you know, some medical products for single use (polymer syringes, blood transfusion systems, Petri dishes, pipettes) are sterilized by radiation (gamma rays in special installations), so they are fragile and cannot withstand sterilization at high temperatures.
Accordingly, the composition of blood and milk does not change in any way. There is no need to pump (not once, not twice, not three, not fifteen). There is no need to wait for time (not an hour, not a day, not three).
BUT. If you eat a turnip that grew near a source of radiation (or are undergoing treatment or examination using radioisotopes), then you should not only feed, but also be near the child - in these cases, alpha particles enter the body, which are extremely dangerous. When treated or examined with radioisotopes, patients are hospitalized in special departments with shielded rooms.
One more note - radiocontrast substances are not the same as radioisotopes .
Parts of the body and cavities of individual organs that are transparent to X-ray radiation become visible if they are filled with a contrast agent that is harmless to the body, but allows one to visualize the shape of internal organs and check their functioning. The patient either takes contrast agents orally (such as barium salts when examining the gastrointestinal tract) or they are administered intravenously (such as iodine-containing solutions when examining the kidneys and urinary tract) [5].
If you look at several contrast agents for e-lactation, all of them have a risk of 0 (you can look at the groups Iodide Radiopaque Agent and MRI Radiopaque Agent).
That is, lactating women can undergo irrigography, contrast angiography can be done, barium sulfate can be taken to contrast the stomach, etc.
It is possible and necessary to require that non-irradiated areas be protected with an apron or plates. This needs to be done regardless of whether you are feeding or not.
Bibliography:
- Wikipedia (articles “X-rays” and “Ionizing radiation”) https://ru.wikipedia.org/wiki/X-rays
- https://ru.wikipedia.org/wiki/Ionizing_radiation
- SanPin 2.6.1.2523-09 “Radiation Safety Standards (NRB-99/2009)” https://gost.oktyab.ru/Data1/56/56325/index.htm
- Resolution No. 8 of February 18, 2003 on the implementation of SANPIN 2.6.1.1192-03 https://www.zhuravlev.info/files/postan8.doc
- X-ray examination: types of examinations, radiation doses, safety and risks of x-ray examination. https://www.polismed.ru/lab-roentg-post001.html
- Collier's Encyclopedia. X-RAY RADIATION. https://dic.academic.ru/dic.nsf/enc_colier/5698/X-RAY
- RADIATION. Doses, effects, risks. Translation from English by Yu.A. Bannikov. (This booklet is largely based on the findings of the United Nations Scientific Committee on the Effects of Atomic Radiation, a subsidiary body of the United Nations General Assembly, and is edited by Geoffrey Lean. The publication does not necessarily reflect the views of the Committee, of the United Nations Environment Programm, or of the editor © UNEP 1985United Nations Environment program) https://www.russianatom.ru/mediafiles/u/files/MultiMedia/Radiaciya_Dozy_effekty_risk.doc
More materials (if you are ready to help with translation, write to This email address is being protected from spambots. You need JavaScript enabled to view it.:
- Diagnostic X-ray procedures while breastfeeding (in English)
- Booklet on working with radiation for pregnant and lactating women (in English)
- Contrast agents and MRI
- Guide to Contrast Media from the American College of Radiology
- ABM Clinical Protocol #30: Radiology and nuclear medicine studies in breastfeeding women.
Comments:
- In contact with
Futuresbroker
Do I need to express milk after anesthesia?
If the medicine used for pain relief is compatible with breastfeeding, then there is no need to express. If the dose of the drug has been increased or the instructions prescribe using it with caution during breastfeeding, then it is better to express the milk after anesthesia. Your doctor can give you advice on this matter, taking into account the type of anesthesia you were given.
So
- Breastfeeding women are afraid to have their teeth treated because, in their opinion, drugs or x-rays may penetrate into the milk. radiation from x-rays.
- In fact, nursing mothers’ teeth must be treated, since infection from diseased teeth will harm the child more than modern medications compatible with breastfeeding.
- In order not to harm the baby when using anesthesia, you need to tell the doctor that you are breastfeeding, and he will select anesthetics that are not contraindicated during breastfeeding.
- After anesthesia, you need to express only if the dose of the drug was increased, if medications containing adrenaline or outdated painkillers were used.
(0 ratings; article rating 0)
Share Share Share
What can a doctor see on an x-ray?
He can see:
- total number of teeth;
- anatomical features of the structure of the maxillofacial region;
- level, bone height;
- possibility of installing implants.
X-rays are also done for the purpose of establishing a diagnosis, when the doctor cannot make one based solely on the patient’s complaints.
X-rays are also done to monitor the doctor’s work. It shows how:
- canals are sealed;
- tooth removed;
- an implant was installed.
When is it necessary to do a plain radiography of the spine?
X-ray of the spine: coccyx, cervical, thoracic, lumbosacral regions is used:
- For pain, impaired mobility, and a feeling of stiffness in the back.
- For inflammatory diseases such as arthritis or arthrosis.
- For curvature of the spine: scoliosis, kyphosis, lordosis.
- For back injuries, vertebral displacements.
- For osteochondrosis and osteoporosis.
- Suspected tuberculosis, metastatic lesions and spinal tumors.
How to Minimize Exposure to Harmful Rays
Medical practice involves taking x-rays at different stages of life, including during guarding. To reduce the negative impact of radiation, the most effective method is to wean the baby from the breast during the procedure and for several days after it. If this is not possible, then doctors advise drinking a glass of wine (red) immediately after the procedure, and for the week following that day include the following foods in your diet:
- cottage cheese, sour cream;
- seafood delicacies;
- Walnut;
- raw carrots;
- pork, but not too fatty.
For a nursing woman, the consumption of wine will have to be excluded, but the remaining ingredients can be included in the menu without fear.
Recommendations for the recovery period
In order to avoid complications after surgery, you need to follow all the doctor's advice. After the procedure, the doctor applies a cotton swab to stop the bleeding. It should be held for no more than 10 minutes, otherwise the blood clot will dry out and come off along with the cotton wool. With high blood pressure, bleeding continues for a longer time, so the tampon can be kept in place for 15 - 20 minutes.
In the first days you cannot:
- overheat the body, apply warming compresses;
- engage in heavy physical labor and sports;
- lick a blood clot;
- eat hot, spicy, rough food;
- drink through a straw;
- smoke;
- touch the socket with a toothbrush and other objects.
You are allowed to eat after 3-4 hours. The issue of feeding a child should be discussed with a doctor. Local anesthetics practically do not enter the blood, and components penetrate into mother's milk in minimal quantities. If the doctor has not prescribed other medications, then you can feed the baby within a few hours.
After the anesthetic wears off, pain appears. Possible increase in body temperature. To relieve acute symptoms, you can take Paracetamol, Ibuprofen, Naproxen. You can reduce pain and swelling by using cold compresses.
Rinsing your mouth and brushing your teeth is allowed on the second day. For rinsing, pharmaceutical preparations are used: Romazulan, Chlorhexidine, Miramestin. They will prevent the development of infection and inflammation. You can rinse your mouth with an aqueous solution of baking soda and salt. To improve the healing of damaged tissue, decoctions of oak bark, chamomile, and calendula are used.
Preparing for removal
If the tooth begins to ache, the gums are swollen, and the breath smells bad, then this may indicate severe inflammation in the dental system. At the appointment, the dentist collects an anamnesis, conducts a visual examination and sends the woman for an x-ray. It is important for a nursing mother to avoid psycho-emotional stress, so she is allowed to take sedatives in advance.
The best option for maintaining mental stability and eliminating fear is oxygen sedation with nitrous oxide (NAS). It is done in the doctor's office before the procedure. The patient inhales the gas and falls asleep. Additionally, a local anesthetic is injected into the gum.
X-ray and breastfeeding
X-rays and breastfeeding (BF) are not mutually exclusive events. It is not necessary to wean your baby to take an x-ray. Irradiation does not cause changes in the composition of mother's milk. Immediately after the x-ray examination, you can start feeding again.
If there is evidence for a nursing mother, an x-ray can be taken. The composition of breast milk remains unchanged even when X-rays are performed with contrast. The contrast agent formula contains mainly iodine molecules, which are excreted from the body naturally unchanged.
If a woman had an X-ray of her lungs during breastfeeding, then doctors may recommend not feeding the child for 2-3 hours after the examination.
Injuries, bruises, fractures are indications for a chest scan. The image allows you to determine the location of the damage and its complexity. Such an examination may be needed at any stage of feeding.
During pregnancy and lactation, a woman faces calcium deficiency, which manifests itself, for example, in intense toothache and other similar problems. To decide on a dental treatment algorithm, experts advise taking an X-ray of the tooth during breastfeeding.
X-ray examination of infants
When an X-ray examination is performed on a baby, it is worth remembering that this can be harmful to the health of the baby.
Although the chance of harm is low, it is still present, so doctors very rarely prescribe this procedure.
Typically, an x-ray is necessary to confirm or refute suspicions of the presence of pathology. It is generally recommended to do this procedure if the child receives an injury during childbirth. For example, damage to the nasal bones during childbirth requires x-ray diagnosis, although doctors believe that it is extremely undesirable to irradiate a child’s head.
During the procedure, all areas of the baby’s body, with the exception of the area requiring diagnosis, are covered from radiation with aprons.
Infants should not have x-rays if:
- for examination of the thyroid gland;
- for diagnosing pathologies of the pelvic organs in girls;
- for examination of the testicles in boys.
X-rays for infants are contraindicated:
- in the presence of increased sensitivity to ionized radiation;
- with close proximity of organs;
- with uneven development of organs;
- with other individual characteristics.
Ultrasound instead of X-ray
Ultrasound is recognized as a safer diagnostic method than x-rays. Typically ultrasound is used:
- for the diagnosis of congenital dislocations and subluxations of the hip;
- to detect hip dysplasia;
- to assess the condition of joint cartilage tissue.
Ultrasound allows babies to be examined without the use of harmful radiation.
Moreover, with the help of ultrasound it is possible to obtain a more detailed picture of the development of pathology than with x-ray examination, which is not able to provide information about the condition of cartilage and connective tissue.
If a woman who has just given birth needs to undergo an X-ray examination to avoid health problems, she should not worry about changes in the quality of breast milk, since such radiation does not have any effect on it. If there are any concerns or the use of contrast agents, the mother can refuse feeding for a couple of days, having first expressed the milk. If it is necessary to examine an infant using X-rays, you should first obtain a full consultation with a doctor. It is better for infants to use ultrasound instead of x-rays.
Indications for tooth extraction during lactation
During the procedure, drugs are used that can penetrate into mother's milk. If it is possible to postpone the date of the operation, then extirpation is carried out after the child is transferred to artificial nutrition. A dental unit is removed urgently during a purulent inflammatory process, as it contributes to the spread of infection throughout the body.
In what cases is surgery necessary:
- suppuration of a cyst, abscess, periostitis;
- unsteadiness due to periodontitis, periodontal disease of the third, fourth degree;
- odontogenic osteomyelitis, sinusitis, phlegmon;
- tooth root fracture;
- pulpitis, which cannot be cured due to the complexity of the canals;
- impacted figure eight, complicated growth of the third molar, pressure on neighboring teeth;
- deep caries that affected the root.
Unscheduled extraction is also performed in cases of severe, persistent pain.
The procedure has contraindications, including acute respiratory infections, chronic diseases in the acute stage, oral infections, sinusitis, severe pathologies of the liver, kidneys, heart, blood vessels, leukemia, bleeding disorders, and mental disorders.
When should a chest x-ray be taken?
Plain radiography of the chest organs is carried out:
- During an annual preventive health examination to identify risk factors and life-threatening diseases such as cancer or tuberculosis.
- For pain in the chest and heart area.
- With painful or bubbling breathing, sensations of lack of air.
- With loss of appetite and a sharp decrease in body weight.
- For swelling and high blood pressure.
- For injuries, to identify foreign objects in the esophagus, lungs, and respiratory tract.
- If you suspect lung diseases: pneumonia, abscess, pleurisy, silicosis, etc.
Alternative Research Methods
In some cases, minimal radiation doses can lead to negative consequences. Therefore, if it is possible to make a diagnosis using alternative research methods, then it is better to resort to ultrasound. And if the results obtained are not enough, then a more expensive research method is used - MRI.
Women at risk and those whose babies are susceptible to allergies should approach such diagnostic methods with caution. But you shouldn’t neglect your health, so if the procedure is recommended and justified, then it is better to take an x-ray and, if possible, protect the baby as much as possible. After all, if the mother is healthy, then the baby will grow strong and healthy.
Table of approximate radiation exposure values for CT (MSCT)*
*The table shows average and approximate values, which may vary up or down depending on:
- Research protocol;
- Number of scanning zones;
- CT scanner;
- Patient weight;
- Patient's height;
- The ratio of muscle and fat tissue in the patient;
- Goals and objectives of diagnostics.
The tomograph is equipped with a dosimeter, which allows you to determine the level of effective radiation exposure in each specific study. This value is indicated in the conclusion and in a special report file on a DVD or flash drive given to the patient based on the results of the study.
When can an x-ray be prescribed?
A traumatologist or surgeon may prescribe digital radiography of bones and joints (skull, bones of the shoulder, forearm, foot, hand, femur, hip bone, etc.; temporomandibular, elbow, knee, wrist, hip joints, etc. ):
- If the patient experiences pain, crunching, movement blocking, or joint instability.
- In case of injury or suspected injury: dislocation, fracture, sprain.
- In order to make or exclude a diagnosis: longitudinal flatfoot.
- For the diagnosis of growths and calcified areas, metastatic lesions and tumors.
The process of tooth extraction in a nursing mother
The procedure for a woman during lactation is no different from that performed for ordinary patients.
Extirpation of a dental unit is carried out in stages:
- antiseptic treatment of mucous membranes;
- anesthesia with local antiseptics or general anesthesia;
- applying forceps and disconnecting the ligament;
- rocking or dislocation;
- extraction from the hole;
- stop bleeding.
If the third molar from below is removed, the operation becomes more complicated. In order to pull it out, the doctor cuts the gum, removes part of the bone, divides the roots into fragments and removes them separately. To prevent infection, the wound is treated with antibacterial drugs. After all manipulations, the gums are sutured with absorbable or non-absorbable suture material.