This patient guideline is based on the Estonian treatment guideline “Perioperative treatment of acute pain” approved in 2016. The management's wishes for treatment were compiled based on a literature review based on scientifically proven facts. The purpose of the patient guide is to help patients manage postoperative pain and answer questions related to acute pain. Knowledge of pain treatment options helps patients actively participate in treatment. The importance of the topics covered in the patient guide, as well as the accessibility of the text, were appreciated by patients with acute postoperative pain. The patient guide explains the following topics: what acute postoperative pain is, why it is important to treat acute pain, and how to evaluate it. Various chapters describe treatment options for acute postoperative pain. The reader will receive answers to the following questions: why the use of oral medications is preferred for treating pain, whether different painkillers can be taken together, and what else can be done besides medications to relieve pain. Recommendations are also given on how you can manage post-operative pain at home. You can read more about the topics covered in this patient guide on the web pages at the end of the guide (see Appendix 1).
|
What is acute postoperative pain?
Pain is a subjective and unpleasant sensation that affects consciousness and impairs well-being. Acute pain is short-lived, most often has a clearly defined area, a specific onset time, and subjective and objective physical signs: heart rate and breathing become faster and blood pressure rises. Severe pain interferes with sleep and creates feelings of fear and anxiety. Acute postoperative pain occurs due to a surgical procedure or surgery. The severity of pain depends both on the severity of the operation and the size of the surgical wound, and on the person’s pain threshold. People feel and react to pain differently. Pain sensations may also be influenced by the patient's early experiences with pain, his age, gender, cultural background, and psychological factors. In the case of children, their parents' attitude towards pain may also influence pain sensations.
Early pain after amputation
Most often they are associated with crude operating technique, lack of treatment of nerve trunks, and accumulation of fluid in the stump area (hematoma, lymphocele). These pains occur immediately after surgery and continue for a long time, gradually changing their character.
Inflammation or suppuration of the stump in the early postoperative period leads to increased temperature, copious purulent discharge, and wound dehiscence. The pain is bursting in nature and is relieved with anti-inflammatory drugs (analgin, diclofenac).
Continued critical stump ischemia. Incorrect choice of amputation level in an area of poor blood circulation leads to the continuation of gangrene. The wound cannot heal, severe ischemic pain occurs. In this situation, only repeated amputation of the leg will help.
Treatment of gangrene
Amputation Rescue Center
Contact your doctor
or we can contact you
Why is it necessary to treat acute postoperative pain?
Postoperative pain should not be tolerated, as pain may increase the incidence of postoperative complications: recovery after surgery will be slower and therefore the length of hospital stay may increase. If pain is left untreated, chronic postoperative pain is more likely to occur. Effective treatment of postoperative pain eases the functioning of the heart and lungs, reduces the risk of vein thrombosis and helps normalize digestion.
Treatment of late pain after amputation
If phantom pain becomes constant and reaches a level that prevents further rehabilitation, comprehensive treatment is required. Moral acceptance of the fact of the loss of a limb, massage of the stump, uniform pressure created by the bandage, early initiation of physical exercise, the use of temporary prostheses and physiotherapeutic procedures contribute to the reduction of phantom pain. In rare and complex cases, nerve blocks and surgery are required.
Removing a body part is a difficult process. In addition to the participation and support of family and relatives, the help of professional psychologists should not be neglected. In the first months after surgery, factors such as cold or hot temperatures, depression, tension, lack of sleep, poor circulation in the amputated limb, prolonged immobility, and infections (such as influenza or urinary tract infections) can cause increased pain.
In cases where conservative treatment and nerve blockade do not lead to the elimination of pain, it is necessary to perform reamputation with full treatment of the nerve trunks and rational prosthetics. During primary amputation, you need to take care of the conditions for prosthetics and the subsequent rehabilitation process.
How is the severity of pain assessed?
Assessing the severity of pain after surgery is a routine part of patient monitoring. Pain is assessed regularly, and the frequency of assessment depends on the patient's condition and the severity of the operation. Since the sensation of pain is individual and subjective, only you yourself can assess the strength of the pain you experience. The nurse will assess your pain regularly both before and after taking pain medications, both while you are at rest and when moving. Based on the information received, it will be possible to create a pain treatment plan that suits you personally. Various pain scales are used to assess pain. For example, a scale for digital assessment is used in adults. It is used to rate the severity of pain on a scale of ten, where zero means no pain and 10 means the worst pain you can imagine. The patient is asked to rate the pain experienced over the past 24 hours using three different methods. Rate:
- the severity of the existing pain,
- the weakest feeling of pain and
- the strongest feeling of pain.
The arithmetic mean of the obtained scores will show the strength of the patient's feeling of pain during the last 24 hours. Sometimes you are asked to choose words that describe your pain. These words could be:
- no pain
- slight pain
- moderate pain
- strong pain
- very severe pain
- unbearable pain
Figure 1. Numerical Pain Rating Scale Sometimes the face scale (FPS-R) (see Figure 2) or the so-called face scale is used to evaluate pain. This scale can be used, for example, with older children. The face scale will need to be explained to the child so that they can use it to rate their pain. The child will need to explain the scale as follows: “This face (point to the face on the far left) shows that there is no pain at all. Other faces (point to each face from left to right) show that the pain is getting worse and worse. The face on the far right shows that he is in great pain.” After the explanation, you can ask the child which face shows how much pain he is now? According to the child's choice, the rater will be able to give the indicated pain a score of 0, 2, 4, 6, 8, or 10 points, counting from right to left: 0 = not painful at all. 10 = very painful. When evaluating, you cannot use the words “sad” or “happy.” It is imperative to clarify that we are talking only about how the child feels, and not about the external facial expression.
Figure 2. Facial Pain Rating Scale (FPS-R) The above scales are used not only to assess pain in older children, but also for patients with mild to moderate mental illness. For small children, infants and patients with severe mental illness, a behavior scale is used, in which the severity of pain is assessed by a nurse. These scales take into account the patient's vital signs such as heart rate, blood pressure, blood oxygen levels and behavior (facial expression, restlessness, sleep) to assess the severity of pain.
| For best results in pain management, tell your nurse right away if you feel pain—even if the pain is mild or if it occurs at night. Don't endure the pain! |
Phantom and late pain
During amputation, another type of pain may occur that is not associated with tissue injury - phantom pain, which is sometimes difficult to treat with medication. Phantom sensations occur as if in a distant limb (for example, itching in a missing finger; or the ongoing sensation of tearing and crushing tissue that occurred at the time of the accident). The appearance of phantom pain after amputation is often associated with the formation of neuromas (dense, painful, round formations on crossed nerve trunks associated with the growth of nerve tissue).
Our clinic successfully uses the method of treating phantom pain using “mirror” therapy. Sometimes pain in the stump is associated with the formation of ulcers and abrasions during the use of the prosthesis. This situation requires the combined efforts of the surgeon and prosthetist and sometimes requires elective reamputation of the limb. The cause of later pain is mainly negligence in caring for the stump and improper use of prostheses. If, despite following all the rules for using the prosthesis, severe or phantom pain occurs in the stump, you should consult a doctor.
How to treat pain after surgery?
In the treatment of post-operative pain, different medications are used with different methods of administration. In addition, the use of alternative methods is permitted, which can be used in case of mild to moderate pain. To prescribe appropriate pain treatment, it is important to know what medications (including painkillers) you have already used, whether you are allergic to medications, and whether you have had any side effects. When prescribing medication, we take into account modern medical principles related to the operation you performed and pain medications. The choice of an appropriate painkiller, the dose of the drug and the duration of treatment depend on the severity of the pain (mild, moderate or severe pain), the type of pain (whether there was, for example, wound pain or nerve pain), the person himself (elderly, child, pregnant woman, etc.) ), as well as from concomitant diseases. To achieve the best effect of painkillers, take your medications regularly (at regular intervals). Painkillers of different effects are often combined.
Groups of painkillers
Medicines are used as painkillers, which are divided according to the type of mechanism of action into three main groups:
- Simple painkillers. For example paracetamol, ibuprofen and diclofenac.
- Opioids. Medicines in this group are divided into weak opioids - for example, tramadol, codeine, and strong opioids - for example, morphine.
- Maintenance medications. They are used, for example, to treat nerve pain.
CRITERIA FOR SELECTION OF A DRUG FOR ANTIBIOTIC PROPHYLAXIS
Activity spectrum
AMP should include the most common causative agents of postoperative infections, primarily staphylococci, since they cause 80% of the total number of postoperative suppurations. In addition, the spectrum of AMP activity should cover other endogenous microorganisms that contaminate the wound when the integrity of internal organs or mucous membranes is damaged.
Dose
AMP during antibiotic prophylaxis corresponds to the usual therapeutic dose.
Time of administration
AMP is the most important factor in antibiotic prophylaxis. The concentration of AMPs in tissues is comparable to the concentration in blood serum and is achieved 30 minutes after intravenous administration of the drug. For most planned and emergency surgical interventions, it is considered optimal to administer AMPs during induction of anesthesia - 30-40 minutes before surgery.
Frequency of administration
determined by the half-life. A repeated dose is administered when the duration of the operation exceeds 2 times the half-life of the AMP. Prescribing antimicrobial agents to prevent wound infection after surgery is ineffective and impractical.
Route of administration
. It is preferable to administer the antibiotic intravenously, which ensures its optimal concentration in the blood serum during surgery.
Drugs of choice
. From the point of view of effectiveness and safety, the most acceptable antibiotic prophylaxis in surgery are I-II generation cephalosporins (cefazolin, cefuroxime) and inhibitor-protected aminopenicillins (amoxicillin/clavulanate, ampicillin/sulbactam). The main complications when using β-lactams are allergic reactions, which in most cases can be prevented with a careful history taking.
Various perioperative antibiotic prophylaxis regimens have been developed depending on the type of surgery and the suspected pathogen (Table 2). Based on the above regimens, one should also take into account local data on the causative agents of wound infections and their sensitivity to antimicrobial agents in order to promptly make changes to perioperative prophylaxis protocols.
In accordance with the latest international recommendations, the intravenous route of administration is the most optimal for antibiotic prophylaxis. During certain operations (transurethral resection of the prostate, shock wave lithotripsy), it is possible to use AMPs orally.
Paracetamol
Paracetamol is often the first choice for mild to moderate pain. Paracetamol differs from other painkillers (for example, ibuprofen and diclofenac) primarily in that it does not irritate the mucous membrane of the digestive tract. Side effects are rare when taking paracetamol. The most severe possible side effect is liver damage, which is rare and most often occurs due to an overdose of the drug. Paracetamol should be used cautiously in cases of liver or kidney failure, chronic malnutrition or alcoholism. Paracetamol should be prescribed to a child according to his age and weight. If additional medications are used (for example, so-called flu teas), which include paracetamol in combination with an anesthetic, you need to ensure that the amount of paracetamol taken per day does not exceed the permitted daily dose (for adults, 4 grams per day).
Maintenance medications such as gabapentin, pregabalin.
Maintenance medications are those medications that were not originally developed as pain relievers but were later discovered to be useful in relieving certain types of pain. For example, gabapentin and pregabalin were originally used to treat epilepsy. Often these medications are used to treat chronic nerve pain. They are also effective for treating post-operative pain, reducing pain and the need for other pain medications.
| If any side effects occur, tell your nurse or doctor right away! |
After surgery, painkillers can be taken:
- through the mouth
- through injections into a vein or muscle
- through an epidural catheter
- using a medicinal suppository
After surgery, oral pain medications are preferred. Medicine taken by mouth is as effective as medicine given by injection, and there is no pain or injection-related complications such as bleeding or inflammation at the injection site. Pain medications taken by mouth are suitable for all types of pain, but you must be able to eat and drink.
Injecting medication into a vein
If taking the tablets by mouth is not possible due to surgery, the nurse will give you the medication through a cannula into a vein. The analgesic effect will occur within a few minutes. As soon as you start eating and drinking, you can go back to taking pills. After a major and painful operation, painkillers can be taken using a special pain pump, with which you can regulate the dose of painkiller (opioids) injected into the vein. This method is called patient-controlled pain relief or PCA (short for Patient Controlled Analgesia). To take painkillers, use a special pump that will allow you to receive painkillers as soon as you feel the need. The doctor will calculate the dose of medication that is appropriate for you and enter it into the pump’s memory. If you feel pain, press the button and the pump will inject you with the appropriate amount of medication through a cannula into a vein. There is no danger of overdosing on the medication because the pain pump is programmed according to your needs. You must press the pump button yourself; you must not let anyone else do it. If the dose of medicine calculated for you is not enough and does not reduce your pain, tell your nurse or doctor, who will adjust the dose of the medicine given according to the severity of the pain. The PCA pump is also used for children if the child is old enough to use it and he is able to understand the principle of operation of the pump.
Figure 3. PCA pump
Injecting medication into muscles
They try to avoid administering painkillers by injection, since due to heterogeneous absorption, the effect of anesthesia may be less than the expected effect. In addition, the injection can be painful.
Administration of medication using medicinal suppositories
Sometimes, if taking painkillers by mouth is impossible for some reason, medications can also be taken through the rectum. Medicinal suppositories are often used to relieve pain in young children.
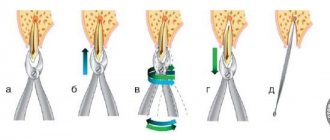
Taking medications through an epidural catheter
Using local anesthesia, if necessary, the anesthesiologist will place a thin plastic probe (epidural catheter) in your epidural space surrounding the spinal canal before surgery. The epidural space is located in the spinal canal, where the roots of the nerves that transmit pain pass. The medicine injected there affects the roots of the nerves and thus prevents the spread of the pain pulse. Therefore, the introduction of drugs into the epidural space is one of the most effective methods of pain relief. Opioids and local anesthetics - a mixture for local anesthesia - are continuously injected into the epidural catheter through an automatic syringe throughout the day. The analgesic effect begins no later than 20 minutes after starting to take the medicine.
Figure 4. Installation of an epidural catheter. Epidural analgesia may cause:
- Nausea and vomiting - anti-nausea medications can help
- Weakness and numbness in the legs - they go away on their own
- Urinary problems - if necessary, a catheter is placed in the bladder
- Lower blood pressure – blood pressure is monitored regularly
- Head or back pain - tell your nurse or doctor. If headaches occur after surgery while you are receiving treatment at home, contact your healthcare provider immediately.
Nerve plexus block
Nerve plexus blocks are most often used to relieve pain in the extremities. Blockades are made either with a single injection or with the use of a catheter, which is installed next to the nerve plexus and is needed for continuous administration of medication (local anesthesia). Medicines are administered through the nerve plexus catheter either with a single injection or with an automatic syringe.
The effect of alternative pain treatment methods on postoperative pain is small, so you should not use such methods alone, but only together with painkillers. Alternative methods can reduce anxiety and tension throughout your hospital stay. Most methods, such as music therapy or distraction, are safe and you can use them without special training or additional equipment. If the pain is mild or moderate, then in addition to painkillers, you can use methods from the list below. You can ask your ward nurse for more information about the different methods.
After discharge
The duration of postoperative rehabilitation averages from 6 to 12 weeks and depends on the type of surgery. The approximate recovery time will be explained to you by your attending physician. Upon returning home, you may experience discomfort and general weakness - this is a normal rehabilitation process.
Activity
After surgery, we recommend that you be as active as possible in your health. Try to walk every day. Just walking down the street or walking on a gym will do. If the weather is not very suitable for walking, you can spend time in the shopping center. Climbing stairs is also suitable as a workout. Do not lift more than 3-5 kg for 4-6 weeks after surgery. Before returning to work, discuss this with your operating surgeon at your first postoperative visit. We do not recommend that you drive a car until the pain is eliminated.
Pain
Moderate chest pain is common after thoracic surgery. The intensity and duration of pain is individual for each patient, but usually goes away within the first month. In addition to pain, you may experience numbness in the suture area and below, tingling and/or increased sensitivity of the skin in this area. These sensations are normal and will also subside in the postoperative period. If pain or other sensations begin to intensify for several days in a row, this is a reason to contact your doctor.
Medicines
Mostly you will be prescribed painkillers. We prefer non-steroidal anti-inflammatory drugs: ketanov, ibuprofen (Nurofen-express), Nise (imisulide), xefocam (lornaxicam), diclofenac. Other painkillers will also work. It should be remembered that these medications irritate the stomach and should be taken after meals. Food should not be too spicy or irritating. If you take painkillers for more than 5-7 days, you should start taking medications that protect the stomach (omeprazole 20-40 mg at night).
You need to watch your diet, drink more fluids, eat more fruits and other foods containing fiber. The intestines should be emptied at least once every 2-3 days. If you are prone to constipation, you can take magnesia or Duphalac.
Postoperative wound care
The surgical incision area should be kept dry and clean. Do not use creams or ointments. You should shower once a day. You can wash with soap or shower gel and do not rub the seam area with a washcloth. After a shower, the postoperative wound should be carefully dried and treated with a solution of brilliant green or potassium permanganate. There is no need to apply any bandages. After all the crusts fall off from the wound on their own and a pink, smooth scar appears, treatment can be stopped. Avoid taking baths for the first 3-4 weeks.
Cold compress
Cold causes blood vessels to constrict and bleeding in the injured area slows down. If you have no contraindications, you can use a cold compress to reduce swelling and pain in the surgical area. As a cold compress, you can use special gel packs sold in pharmacies; any package from the freezer is also suitable. Wrap the cold bag in a towel and then place it on the damaged area and apply a compress if necessary. The towel will protect the fabrics from possible local exposure to cold. Keep the cold compress in place for 20-30 minutes at a time, then pause for 10-15 minutes and repeat the procedure if necessary.
Physiotherapy
Physiotherapy is recommended to be added to the postoperative treatment regimen, as it reduces the risk of complications and facilitates the recovery of the body after surgery. Physiotherapy is carried out by a specialist. He will explain to you why it is necessary to start moving as quickly as possible after surgery, teach you how to take as comfortable and relaxed a position as possible after surgery, and how to support your body with pillows or the surgical area with a bandage. In addition, he will teach you breathing techniques, as well as motor exercises.
Music therapy
Listening to music reduces anxiety, slightly reduces the severity of post-operative pain, and with music the stress reaction associated with pain occurs less frequently. Therefore, the need to take opioids is reduced. If you enjoy listening to music and it relaxes and calms you, then we recommend that you take your favorite music with you to the hospital. You just need to remember that other patients may not like your favorite music, so we recommend that you use headphones when listening to music.
Why does postoperative pain occur?
Postoperative pain according to ICD-10 (International Classification of Diseases) refers to unspecified types of pain and does not carry any signaling information for either the patient or the doctor, since the causes and mechanisms of its occurrence are clear. Therefore, modern principles of patient management after surgery provide for maximum relief from unpleasant pain. Moreover, pain has a negative impact not only on healing, but also on vital processes in the body: the functioning of the cardiovascular, respiratory, digestive, central nervous systems, as well as blood clotting4.
The formation of painful sensations is ensured by a multi-level reaction that connects the immediate area of damage (wound surface) and the central nervous system. It begins with mechanical stimuli in the area of the incision and the release of biologically active substances (prostaglandins, bradykinins and others)4, and ends with information processing in the cerebral cortex and the connection of emotional and psychological components.
Pain syndrome develops as a result of the emergence of areas of increased pain sensitivity (hyperalgesia). Primary hyperalgesia is associated directly with damage and forms near the wound. The area of secondary hyperalgesia covers a larger area and occurs later, over the next 12-18 hours4, as it is associated with stimulation of other types of receptors. It is she who is responsible for the preservation and intensification of pain on the second or third day after surgery, and subsequently for the development of chronic pain syndrome7.
Up to contents