Why does pain occur in the upper jaw?
Injuries
Damage occurs as a result of household, street, sports, automobile, and industrial injuries.
The bruise is characterized by moderate pain that goes away after a few days. Fractures of the upper jaw are accompanied by extremely intense acute pain, rapidly increasing swelling, facial asymmetry, and stepped dentition. In case of fractures of the alveolar process, lacerations are visible on the mucosa, and sometimes the end of the displaced bone fragment is determined. The occlusal contact is sharply impaired, the teeth are mobile. With an isolated fracture of the walls of the maxillary sinus, severe aching pain in the upper jaw, infraorbital area, significant swelling, and hemorrhages is observed. Nasal breathing is difficult. With combined damage to the bone walls of the sinuses, a clinical picture of a concussion and profuse nosebleeds are revealed. Perforation of the maxillary sinus occurs during dental procedures. If the damage was not detected, swelling of the cheeks, a nasal tone of speech, pressing or bursting pain in the jaw, and projections of the sinuses subsequently appear.
In some cases, radiating pain in the jaws is detected in victims with subluxation of the cervical vertebra. Irradiation to the back and shoulders is also possible. The clinical picture includes a forced position of the head, neck pain, muscle tension, and sometimes dizziness, weakness, convulsions, and paresthesia in the arms.
Dental reasons
Discomfort and mild pain may be associated with the use of removable dentures and orthodontic structures. Pulling, pressing, aching pains occur in children due to malocclusion, including those caused by deformation of the upper jaw with a cleft lip and cleft palate. Some soreness is normal after tooth extraction, especially molars and wisdom teeth.
With the development of alveolitis, the pain disappears, and then reappears 3-5 days after tooth extraction. Intense pulsating sensations are noted in the projection of the socket, intensify as inflammation progresses, and sometimes cover the upper jaw and half of the face. Attacks of severe pain spreading along the trigeminal nerve are characteristic of acute diffuse pulpitis. More local pain is observed in acute periodontitis.
Upper jaw pain
Purulent processes
Intense tugging, tearing, bursting pain occurs with purulent inflammation of the upper jaw and nearby soft tissues. Combined with hyperthermia, deterioration of general condition, intoxication syndrome. The most striking clinical picture occurs in acute osteomyelitis. The disease begins suddenly, the symptom progresses quickly, and the temperature rises to high levels. A foul odor emanates from the mouth, and pus accumulates in the gum pockets.
Periostitis has less severe symptoms. With a high intensity of pain, the general condition is slightly disturbed, the temperature is subfebrile. In patients with a perimandibular abscess, the abscess is limited, located in the soft tissues, the condition is moderate or closer to satisfactory. With perimaxillary phlegmon, the infection spreads quickly, twitching, shooting pains intensify with the slightest movements of the jaw, the condition is serious.
With abscesses of the salivary glands, the first symptoms are dry mucous membranes and an unpleasant taste in the mouth. Hyperthermia up to 40°C is noted. Maximum pain is determined in the projection of the affected salivary gland, complemented by pronounced swelling. Irradiation is noted in the upper jaw, neck, and ear.
Neuralgia
With ganglionitis of the pterygopalatine ganglion, a clinical picture of neuralgia of the trigeminal nerve is observed in the zone of innervation of its 2nd branch – n.maxillaris. An attack of intense shooting pain develops spontaneously, often occurring at night. Pain sensations predominate in the upper jaw, eye, hard palate, and at the base of the nose, spreading to nearby anatomical zones. The episode lasts from several minutes to several hours, complemented by autonomic disorders: lacrimation, profuse salivation, hyperemia of half the face.
Atypical facial neuralgia, which is more often detected in middle-aged women, is considered as another possible cause of the symptom. Pathology is provoked by dental procedures. The pain is dull, sometimes burning. They do not reach the intensity typical of other neuralgia. They quickly transform from paroxysmal to permanent.
Diseases of the ENT organs
In otolaryngology, the manifestation is more often provoked by odontogenic sinusitis against the background of injuries, dental diseases, and endodontic treatment. The acute form is characterized by heaviness, bursting unilateral pain in the upper jaw, intensifying when lowering the head, and throbbing headache. There is a sharp pain when chewing food, a subjective feeling of lengthening of the teeth. For chronic sinusitis, the clinic unfolds gradually. The symptom is also combined with a headache, radiating to the forehead, temple, and orbit.
Radiating pain in the upper jaw, orbit, and temporal region can be observed in acute purulent otitis and is caused by irritation of the trigeminal nerve during infiltration of the mucous membrane of the tympanic cavity. Supplemented by severe pain in the ear, intoxication syndrome. A similar irradiation is found in mastoiditis, which develops simultaneously with otitis media or a few days later, manifested by profuse suppuration from the ear, throbbing pain behind the ear.
Tumors of the upper jaw
Against the background of benign neoplasia of the upper jaw (fibromas, cementums, osteomas, osteoblastoclasts), the pain is usually mild, dull, and aching. They do not occur in all patients. They grow slowly over a long time in parallel with the growth of the tumor. Sometimes they are complemented by progressive facial asymmetry. An exception is osteoid osteoma, which is characterized by intense pain that worsens when eating and at night.
With malignant tumors of the upper jaw (cancer, sarcomas), pain appears in the early stages. At first periodic, dull, aching or pressing. They quickly intensify, become permanent, acute, painful, unbearable. They radiate to adjacent anatomical zones. They are supplemented by tooth loss, infiltration of nearby tissues, decay with the formation of ulcers, and enlargement of regional lymph nodes.
Other reasons
Aching, initially paroxysmal, then constant pain in the upper and lower jaw is observed with bruxism and myofascial syndrome. In both cases, the cause is constant excessive load on the masticatory muscles. In patients with Horton's disease, the symptom is caused by irradiation and is combined with a dull headache that gradually increases over several weeks, more pronounced in the temporal region.
Pain in the temporomandibular joint
Temporomandibular joint dysfunction (TMJ) is one of the most common causes of facial pain and is often incorrectly referred to as temporomandibular dysfunction. There are 2 main types of TMJ dysfunction: myogenic (the source of muscle pain) and arthrogenic (the source of pain is the TMJ). Understanding TMJ Dysfunction
This disorder involves the presence of the following symptoms: - pain or discomfort in or around the ear, TMJ and/or muscles of the jaw, face, temple area and neck on one or both sides.
Pain can occur unexpectedly and increase in frequency and intensity over months and years. Mouth opening with a click, crepitus, closing, restriction of opening or deviation of the lower jaw during movement, difficulty chewing, and headache are also associated with TMJ. Structure of the TMJ The
temporomandibular joint, or TMJ, is a freely rotating and sliding joint, covered with fibrocartilage, a football-shaped ball (condyle), a fibrous pad (disc), a bone socket for the pad (fossa), ligaments, tendons, blood vessels and nerves.
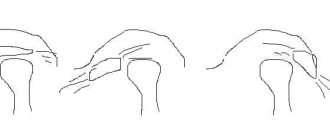
The disc functions as a moving shock absorber and stabilizer between the condyle and fossa. When the jaw opens, the condyle normally rotates first and then slides forward within the fossa with a disc located between the condyle and the fossa. Muscles of mastication
Muscles attached to the lower, upper jaw, skull and neck.
The muscles of mastication open, close, extend, and move your jaw, allowing you to speak, chew, and swallow. The accessory muscles of mastication (neck and shoulder muscles) stabilize the skull on the neck during chewing. Myogenic TMJ dysfunction (muscle-related)
Typically occurs due to overuse, fatigue, or tension in the masseter or accessory muscles, resulting in facial pain, headaches, and sometimes neck pain.
Arthrogenic TMJ dysfunction (joint-related)
Typically results from inflammation and degenerative changes in the hard and soft tissues of the joint.
Capsulitis or synovitis (inflammation), slipped disc (also called internal injury) and degenerative arthritis are the most common causes of TMJ dysfunction. Causes of TMJ Dysfunction The exact causes of TMJ
dysfunction are still unclear.
It is believed that the development of dysfunction is due to a combination of several severe factors, including injury and joint disease. Teeth clenching and grinding (bruxism), as well as tension in the neck and head muscles, are currently not proven causes of TMJ dysfunction, but they can aggravate the symptoms of this disease and must be taken into account in the treatment and management of patients with this pathology. It is important for patients with this dysfunction to understand that this disease can be chronic and can be very dependent on many factors, including emotional stability. Because there is no quick fix or emergency treatment for TMJ, the most successful and expert-supported treatments focus on self-monitoring and managing aggravating symptoms. Factors Associated with TMJ Dysfunction
- Trauma: Direct trauma to the jaw is associated with symptoms of dysfunction.
Direct trauma to the jaw can occur from a blow to the jaw, hyperextension (strain) of the jaw, and in some cases, compression of the jaw. Prolonged or forceful dental procedures, intubation during general anesthesia, and surgical procedures of the mouth, throat, and upper gastrointestinal tract (esophagus and stomach) can injure the TMJ. — Incorrect habits: Habits such as clenching teeth, clenching the jaw, grinding teeth (bruxism), biting lips or nails, chewing gum, and placing the jaw in abnormal positions are common. In relation to them, evidence of their involvement in the development of dysfunction has not been proven. Such habits are often associated with TMJ dysfunction and can contribute to the emergence of factors that translate into a chronic form and aggravate the existing symptoms of the pathology. — Occlusion: Dental occlusion refers to the way the teeth fit together or “bite.” Historically, dentists have viewed malocclusion as the primary cause of TMJ dysfunction. Recent studies have shown that malocclusion does not usually lead to this group of diseases, with the exception of a few cases. Each situation must be considered individually so that the doctor can make a differential diagnosis of facial pain. — Psychological factors: Many patients with TMJ dysfunction say that the onset of symptoms of the disease or worsening of its course is accompanied by an increase in emotional stress and psychological imbalance, leading to depression or anxiety. Scientific research shows that many patients with this dysfunction experience varying levels of depression and anxiety, and these levels are higher than those without this dysfunction. To date, it has not been established whether symptoms of depression or anxiety are present before the onset of TMJ dysfunction and then contribute to its formation, or whether chronic pain associated with this pathological condition leads to the formation of anxiety and depression. Many patients begin to clench and grind their teeth more frequently and intensely when they experience emotional stress, psychological imbalance, or pain. — Disorders of the temporomandibular joint: Some types of arthritis can lead to damage to the TMJ, as well as other joints. This is common in osteoarthritis developing in the aging population. Many other diseases, such as Parkinson's disease, myasthenia gravis, strokes, amyotrophic lateral sclerosis, can lead to excessive or uncontrolled movements of the masticatory muscles. — Other factors: Drug use and some prescribed medications can affect the central nervous system and muscles, and lead to TMJ dysfunction. Diagnosis of TMJ dysfunction.
Diagnosis of this disease should be part of routine practice among general practitioners and dentists.
A short set of diagnostic procedures may include: - History of the disease: complaints of pain in the jaw, headaches, neck pain, discomfort in the TMJ area, jaw closing, clenching of teeth, damage to the jaw, head, neck, as well as a history of cases of TMJ dysfunction or treatment of facial pain. - Objective examination: may include measurement of jaw opening, combined movements, jaw deviation during opening, palpation (finger pressure required) of the joint, jaw, head and neck muscles to determine pressure points and the presence of crepitus. It is also necessary to evaluate the gums, soft tissues of the mouth, teeth and make notes about the disease, the presence of dental lesions, as well as the symmetry of the jaw, face and head. If any abnormalities are found during the examination, a more detailed history should be collected and a more in-depth examination performed. Comprehensive assessment of TMJ dysfunction A comprehensive assessment may include:
- A complete analysis of all symptoms related to TMJ, head, neck, medical history, dental history, life history, heredity, psychological history.
— Comprehensive objective examination of the face, cervical spine, masticatory muscles, head and neck, neurological structures, teeth, gums, hard and soft tissues of the oral cavity. — Psychological history, including a short survey and testing. — Additional tests, including x-rays and imaging tests, biopsies, blood tests, urine tests, neurological tests, diagnostic injections. Treatment of TMJ dysfunction
Since there is no known cure for this pathology, the management of patients with symptoms of dysfunction is similar to the management of patients with other orthopedic or rheumatological disorders.
The goals of managing this group of patients are: reducing pain, adverse pressure and stress on the jaws, restoring jaw function, implementing a well-planned management program to treat the physical, emotional and psychological aspects. Management options and sequence of treatment for TMJ dysfunction are similar to other musculoskeletal diseases. As with many musculoskeletal disorders, the signs and symptoms of TMJ can be temporary and resolve on their own without developing serious long-term consequences. For these reasons, it is particularly important to try to avoid aggressive and irreversible treatment options such as surgery, major dental surgery or orthodontic treatment. Conservative management techniques include changes in behavioral habits, physical activity, medications, jaw exercises, and orthopedic devices. All of them have been found to be safe and effective treatments for cases of TMJ dysfunction. Most patients suffering from this disease achieve long-term remission with conservative therapy. Scientific studies show that in more than 50% of such patients, only a few symptoms persist or disappear completely. Self-monitoring of patients should include: - Limited jaw opening (no more than 2 fingers wide). — It is necessary to give your jaws a rest, avoiding prolonged chewing (chewing gum, bagels, tough meats). - Avoiding grinding and clenching of teeth by relaxing the jaw area and keeping the upper and lower rows of teeth at a distance. - Avoiding leaning or sleeping with the jaw resting. — Avoiding pushing movements with the tongue and chewing non-food items (nails, pens, pencils, etc.), stress, pressure on the jaw. - Use of cold, ice or moist-warm compresses, as prescribed by the attending physician or therapist. — Performing a massage of the affected muscles. - Perform gentle, limited jaw exercises as prescribed by your healthcare professional. — Use of medications as prescribed by the attending physician. Treatment options.
— Orthotics: You may be offered a brace (or a retainer known as a night watchman) that fits over your upper and lower rows of teeth.
The retainer has many different purposes, and it can be worn either constantly or part of the time, it all depends on the prescription of the attending physician. In most cases, retainers are used to separate rows of teeth, realign jaw joints, and help jaws relax. The unique style and adjustment of the brace will depend on your condition, how it changes while you wear the brace, and your overall treatment plan. Managing patients under stress.
One of the goals of treating TMJ dysfunction is to identify therapy for daily stress.
Your doctor may recommend several options for you to do this. These options include: biofeedback (biofeedback), breathing for relaxation, image management, and sometimes, referral to a specialist. Physiotherapy.
Physical therapists are specially trained professionals who assist in the rehabilitation of all types of physical injuries.
There are many treatment options that can help. These include: jaw exercises, posture training, ultrasound, electrical stimulation and mobilization. Your doctor and physical therapist will work together to formulate your treatment plan. Correcting your bite
Sometimes it is necessary to improve the way your teeth fit together.
This can be achieved in various ways. Orthodontics, usually with braces, will help move the teeth so they fit together better. In some cases, when the jaws themselves are not misaligned, they are corrected by a combination of treatment by an orthodontist and an oral surgeon. This is called orthognathic surgery. Correction of the bite occurs through the intensive work of the dentist, with the installation of crowns, bridges, and, if necessary, implants. This is done to replace missing teeth or to change the size and shape of teeth so that they fit together and function more harmoniously with the jaws and muscles. Surgery is sometimes performed to repair or reconstruct the jaws when conservative treatment fails to achieve comfort and good function. Surgery is rarely necessary, but it can be performed to remove debris that may have accumulated in the joint cavity, to repair damaged tissue, or even to replace the entire jaw, such as other joints (knees, hips, and shoulders). Conclusions
Extensive research is now being conducted to determine the safety and effectiveness of treatments for TMJ dysfunction/orofacial pain syndrome. Many researchers and clinicians advocate reversal and conservative treatment of dysfunction. Even when the symptoms of this dysfunction persist for a long time and are pronounced, many patients with this pathology do not require invasive treatment. Treatments designed to change the bite or reposition the jaws through orthodontic or dental reconstructive procedures are usually not necessary. And if they are used, then only when absolutely necessary. If permanent treatment is being considered for TMJ dysfunction or orofacial pain, we recommend seeking a second opinion. Specially trained dentists, physical therapists, psychologists and clinicians are often the best source of correct diagnosis and further management of this group of patients.
Exercises for the temporomandibular joint
Diagnostics
Determining the causes of a symptom is the responsibility of the dentist. Patients may need to be seen by an ENT doctor and an oral and maxillofacial surgeon. Consultations with a neurologist, traumatologist or rheumatologist are less often indicated. The doctor collects complaints, examines the dynamics of the development of the disease, finds out possible provoking factors, establishes the nature of pain, their relationship with the time of day, food intake, and other circumstances.
Based on the survey data, general and dental examination, a diagnostic action plan is drawn up, which may include the following procedures:
- Radiography.
X-ray examination of the upper jaw is used to detect tumors, purulent bone lesions, traumatic injuries, and dental diseases. For sinusitis, X-rays of the paranasal sinuses are performed, and for mastoiditis, images of the temporal bone are taken. - Other imaging techniques
. and MRI are used at the final stage of the examination when radiographic data are ambiguous, to detail the changes identified on the X-rays. They allow you to accurately determine the location and extent of lesions in neoplasms, injuries, purulent inflammation, and other pathological processes. - Otolaryngological techniques
. Along with radiography and CT, anterior rhinoscopy, probing of the maxillary sinus, and diagnostic puncture of the sinus are used in the diagnosis of odontogenic sinusitis. If mastoiditis is suspected, otoscopy, hearing testing with tuning forks, and audiometry are performed. - Punctures, biopsies
. For deep perimaxillary phlegmon, a non-palpable area of fluctuation, puncture of the pathological focus is recommended. Enlarged lymph nodes against the background of space-occupying formations are an indication for a biopsy to exclude lymphatic metastases. - Lab tests
. During inflammatory processes, a general blood test reveals an increase in ESR, leukocytosis, and a shift in the leukocyte formula to the left. Examination of purulent discharge allows us to identify the causative agent of the process and determine antibiotic sensitivity. Histological or cytological analysis makes it possible to establish the type of neoplasm and differentiate between malignant and benign tumors.
Treatment planning
Migraine knocked on my head...
We all know headaches. The most common type of headache is a migraine. It often appears along with toothache. More recently, scientists have proven that sometimes it is teeth, even healthy ones, that can cause severe migraines.
A headache in itself is not a disease, but it is a symptom that not everything is okay with your physical and sometimes mental state. However, in many cases, despite a thorough examination, no cause for acute headache can be found. Experts say that prolonged attacks of headaches or migraines are a sign that you need to go to the dentist, even if the teeth themselves do not bother you.
Of course, most often the cause of severe headaches, which the vast majority of people suffer from, are injuries to the temporal part of the head. But, in addition, migraine attacks can be associated with inflammatory diseases of the oral cavity, in particular caries. This is due to some deformation of the teeth, causing the upper jaw to be too close to the lower jaw.
The fact is that headaches often occur due to malocclusion. And a huge number of people with crooked teeth are not even aware of their problem. When teeth are positioned incorrectly, pressure is placed on the muscles, nerves and blood vessels located nearby, causing migraine attacks.
As a result of the incorrect position, the temporomandibular joint, the movable connection of the lower jaw with the base of the skull, suffers. At the same time, researchers were able to identify a trend in which people who suffer from temporomandibular joint arthritis are also more likely to have dental problems. Their surfaces are almost constantly in contact, as a result of which severe tension arises in the chewing and facial muscles, accompanied by pain when eating food.
Typically, people experiencing these symptoms are referred to an otolaryngologist or neurologist, but they may also benefit from seeing a physical therapist and dentist. In turn, regular monitoring of the condition of teeth and timely treatment of caries can be one of the most reliable methods of preventing disorders of the temporomandibular joint, as well as most cases of practically untreatable migraine.
Be wary if your head hurts in the morning, if you experience pain behind the eyeballs, in the sinuses, in the neck and shoulders. It is necessary to visit a dentist as soon as possible. Consider having your teeth and gums examined at least twice a year.
Treatment
Conservative therapy
Pain syndrome is relieved with analgesics. The treatment plan is drawn up taking into account the cause of the symptom. The following methods are used:
- Dental diseases
. For alveolitis, wash the hole with hydrogen peroxide or nitrofural, apply applications with anesthetics and analgesics. For pulpitis and periodontitis, the tooth cavity is treated and disinfected, regenerating and anti-inflammatory pastes are used, pain is eliminated with analgesics, and antibiotics and sulfonamides are prescribed to combat inflammation. - Traumatic injuries
. A conservative method of treating fractures of the upper jaw is the application of dental splints connected to a horseshoe-shaped bracket in the forehead area. To immobilize the alveolar process, a splint-bracket made of aluminum wire is used, fixed to the teeth using a light-curing composite and adhesive material or metal ligatures, if necessary, in combination with a chin sling. - Purulent processes and ENT pathologies
. Patients are prescribed broad-spectrum antibiotics; after a bacteriological examination, the drug is replaced taking into account sensitivity. Additionally, immunocorrectors, detoxifying, anti-inflammatory, and antihistamines are used. Local treatment includes rinsing and dressings. - Ganglionitis of the pterygopalatine ganglion
. To reduce pain, the nasal cavity is lubricated with dicaine, and turundas with novocaine are administered. In severe cases, ganglion blockers and ganglion blockades with anesthetics are recommended. Local administration of hydrocortisone is effective. Medicines with antiallergic and restorative effects are indicated.