How to use prosthetic teeth for periodontitis and periodontal disease
Periodontitis and periodontal disease are gum diseases with different origins. The first pathology occurs due to pathogenic microorganisms, and the cause of the second is a metabolic disorder in tissues. The processes in both cases lead to loose teeth, so it is much more difficult to prosthetize teeth. However, modern dentistry can cope with such situations and return the aesthetics of a healthy smile to the patient.
Differences and characteristics of diseases
Periodontal disease occurs when there is a metabolic disorder, which leads to a failure in the process of renewal of gum tissue. This, in turn, causes loose teeth. In the early stages, the pathology is almost impossible to detect, since there is no pain or bleeding. Other signs include:
- bad breath is noticeable;
- gums become pale;
- the roots of the teeth are exposed.
Important: without treatment, the patient may completely lose teeth.
Periodontitis is different in that it is caused by gum inflammation and in most cases it is a consequence of bacterial gingivitis. The disease has characteristic symptoms:
- swelling and severe pain;
- bad breath;
- redness of the gums.
The acute form is manifested by bleeding and constant pain. Without treatment, gum tissue erodes and cannot hold teeth in place. These pathologies have several treatment options, which are prescribed by the dentist. Advanced stages definitely require one of the prosthetic methods.
How to choose a denture for periodontal disease
The disease cannot be completely cured at the moment, but medicine can achieve stable remission and a stable condition. If the disease is detected at an early stage, then therapeutic methods are used. If the condition is neglected, the teeth will need to be completely removed and replaced with dentures.
In any case, dentists carry out treatment to achieve remission of periodontal disease and stop the loss of bone tissue. Only after this, a prosthetic option is selected, using removable or non-removable orthopedic structures:
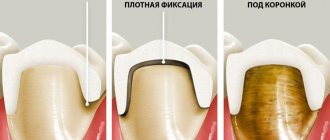
- zirconium crowns, which are placed on your own ground teeth. Usually they are placed in the smile zone;
- bridges fixed to crowns or abutment teeth. This solution is suitable only for the initial stages of pathology;
- splinting clasp dentures. This is a conditionally removable option that has minimal impact on the oral mucosa;
- implant-supported dentures (to avoid the risk of rejection, it is important to regularly treat periodontal disease).
The choice of orthopedic design depends on the clinical case and general health. If the patient still has his own teeth, the doctor will recommend a removable denture. In difficult clinical situations, two methods are suitable: installation of splinting clasps and implantation with immediate loading.
Removable tires
The splinting properties of removable splints are provided by various combinations of continuous support-retaining and reversible clasps, as well as different shapes of occlusal pads. Their spread was facilitated by the development of parallelometry techniques, precision casting on refractory models, and the use of cobalt alloys and precious metal alloys.
Removable splints can be used to splint one group of teeth or the entire dentition. When immobilizing the front teeth, it is advisable to bring the splint to the premolars, and when splinting the lateral teeth, to the canines.
Removable splints can be included in the design of the arch prosthesis as its integral part. These are prosthetic splints:
1) continuous clasp type tire;
2) splint guard;
3) a single splint for the entire dentition.
Orthopedic systems for periodontal disease
Before selecting the optimal option, it is necessary to evaluate the supporting teeth to see whether they can withstand the chewing load. They must not be allowed to fall out or become loose after prosthetics.
Important: before taking impressions, the gums should not be inflamed due to periodontal disease, otherwise the finished prosthesis, crowns or inlays will be uncomfortable to wear. In addition, the risk of root infection will increase.
The most commonly used constructions are:
- Zirconium crowns.
For this pathology, metal ceramics are contraindicated and porcelain is not used. Therefore, the patient is offered products made from zirconium dioxide. They are more expensive than other crowns made from other materials, but are biocompatible with gum tissue and provide excellent aesthetics.
- A bridge that is used only in certain cases.
Its peculiarity is that installation requires supporting teeth, inlays or implants. The gums and other tissues experience pressure from such a prosthesis, which gradually leads to bone atrophy, so the system does not last long, about 5 years.
- Implantation, which is possible even in one stage.
Previously, it took time for artificial tooth roots to heal, and only six months later permanent crowns were fixed on them. The one-stage method involves making a small puncture into which a titanium base is inserted and the prosthesis is almost immediately put on. The method is also called momentary loading implantation.
- Clasp prosthesis.
Option suitable for periodontal disease and periodontitis. It does not have high aesthetics, but returns functionality when eating. With the help of a prosthesis, the load on the bone is distributed evenly. Abutment teeth will be required for installation.
Main types of splinting.
The direction of pathological mobility of any tooth is always cut out and depends on its location in the dental arch. For molars and premolars, the lines of their mobility lie in almost parallel planes, for incisors and canines - in planes located at an angle to each other. The best result of splinting is achieved if the splint unites the teeth and the fracture lines lie in intersecting planes.
For the anterior group of teeth, a splint is used to unite the incisors and canines. This is anterior immobilization. It is convenient because, firstly, the periodontium of the canines is less affected and takes on part of the pressure, unloading the weakened periodontium of the incisors, and secondly, the unity of a group of teeth that have the same is restored; thirdly, the teeth are located in an arc, due to this Shinan has greater stability. Immobilization of teeth, in which the splint is located in the anteroposterior direction, is called lateral (sagittal). Lateral immobilization allows you to create a block of teeth that are resistant to forces developing in the vertical, transverse and anteroposterior directions. With the slightest degree of atrophy of the sockets, this is enough to reduce the functional load and obtain a therapeutic effect.
Prosthetics for periodontitis
Before choosing one of the methods, the specialist conducts training. It will be approximately the same for periodontitis and periodontal disease. The set of activities includes:
- elimination of caries;
- cleaning gum pockets and teeth from stone and plaque;
- antibacterial and physiotherapy;
- removal of loose teeth.
Until recently, many types of prosthetics had contraindications for periodontal tissue diseases. The problem is that pathologies lead to thinning of the bone and loosening of the teeth.
But now prosthetics have become possible subject to certain conditions, including:
- installation of certain types of systems;
- stabilization of the pathological process;
- use of special materials.
As with periodontal disease, bridges are used at the initial stage. To restore chewing and aesthetic functions, clasps and prosthetics on implants are more often used.
Help: there is also the option of a complete denture (densary jaw) made of acrylic or nylon, but it, like the “bridge,” is rarely used because it does not prevent bone loss.
Orthodontic treatment in patients with severe forms of periodontitis: a clinical study
Today, the need for orthodontic treatment is increasing among all age and social groups. The success and effectiveness of such treatment directly depends on the response ability of periodontal tissues. Orthodontic tooth movement involves remodeling of the alveolar bone, while the movement itself is associated with a physiological process of cellular activity in the periodontal connective tissue and activation of the osteoblast-osteoclast complex in the alveolar bone. Due to the complexity of aesthetic and functional rehabilitation, the joint solution of periodontal and orthodontic problems becomes a necessity to achieve therapeutic goals.
Orthodontic therapy using fixed and removable appliances can lead to various side effects, such as plaque formation or the development of caries. Moreover, bacterial contamination increases in areas of retention, in which mechanical removal of plaque becomes very difficult. These changes can cause a quantitative increase in bacteria, including periodontal pathogens, Actinobacilus actinomycetemcomitans and Porphyromonas gingivalis. Orthodontic treatment has a significant impact on periodontal health, promoting the accumulation of plaque, which leads to enlarged gums, an increase in the depth of gum-gum pockets, and bleeding during probing. All of these problems can be solved by a strict approach to oral hygiene during and after treatment.
Due to permanent trauma to periodontal tissues and decreased supporting function, orthodontic tooth movement is contraindicated in patients with untreated periodontitis. Periodontal treatment in the form of scaling, root planing, and deep pocket removal should be performed before orthodontic therapy is initiated, as the presence of deep periodontal pockets can transfer microbial plaque from the supragingival to the subgingival, thereby causing attachment loss and the development of an angular bone defect.
Localized aggressive periodontitis, a form of severe periodontal disease, is associated with loss of connective tissue attachment, intraosseous pockets, and vertical bone defects in certain specific locations of the dental arch, such as first molars or earlier incisors.
In 30-50% of patients affected by moderate to severe periodontitis, pathological migration occurs along with loss of attachment and severe bone resorption, which is clinically manifested in elongation, diastema, rotation and labial inclination of the central teeth.
To relieve vertical bone defects, regenerative treatment is very successfully used, however, when the tooth migrates from its original location, ideal aesthetics and reconstruction of the interdental papilla cannot be achieved, which is why in such situations the need for orthodontic intervention arises.
A combination of periodontal tissue treatment and intrusion of anterior elongated teeth along with controlled hygiene is the best treatment plan for correcting the relationship of teeth in aggressive forms of periodontitis.
Moreover, vertical orthodontic movement may resolve some bone defects in these patients, eliminating the need for subsequent surgery.
Since the stability of periodontal therapy is of paramount importance, regular visits and monitoring are a necessity in such situations. For this purpose, instruction in oral hygiene, regular visits every 3-6 months, measurement of the depth of the gingival sulcus, assessment of tooth mobility, gum recession and bone structure are carried out.
The present study shows periodontal parameters at the end of orthodontic treatment in patients with severe periodontitis.
Materials and methods
This uncontrolled clinical study was approved by the ethics committee of Tehran University of Medical Sciences Dental School. Examinations were carried out after obtaining written consent from each patient. The subjects of the study were eight patients (seven women and one man with an average age of 30 years) who were referred for periodontal treatment of aggressive forms of periodontitis with a history of extrusion and orthodontic treatment. In all patients, the depth of the periodontal pockets was >=5 mm, intraosseous defects were noted, extrusion of up to 1 mm relative to adjacent teeth in the dental arch, and a plaque index of less than 15%. Participants were excluded from the study if they had systemic diseases, had used medications in the past 3 months, smoked, or were unable to pay for orthodontic treatment or participate in regular checkups.
All patients had clinical and radiological signs of aggressive periodontitis. All underwent scaling, smoothing of the root surface, as well as open curettage with removal of the internal pocket and infected contents. Instructions are given for oral hygiene before starting orthodontic treatment.
After stabilization of the periodontal status and reduction of periodontal pockets to 15% or less, after establishing strong bonds for regular visits, fixation of fixed orthodontic appliances to the entire dental arch, wire intrusion technique and alignment of the central incisors were carried out. The load was applied evenly to each tooth, 10-15 g (tested using Correx, HAAG-STREIT Holding, AG) according to the individual periodontal status. To prevent anchor loss, we used the full arch technique, adjusting the fixtures every 4 weeks. Oral hygiene instructions and root planing were performed every three months. Overall, orthodontic treatment lasted from 10 months to 2 years depending on the patient (Figure 1). Then the therapy was transferred to the retention phase. At the end of the treatment, the fixed equipment is released and retainers (Braided stainless steel, 0/38 mm, Dentaflex, Germany) are fixed on the lower and upper jaws. Recommendations on oral hygiene are again given.
Figure 1: (a,b) Frontal and lateral views of a displaced right upper central incisor associated with bone loss in a patient with aggressive localized periodontitis (pathological movement) after periodontal tissue treatment and before application of orthodontic force (c,d) 6 months of orthodontic treatment full-arch technique for intrusion of an anterior displaced tooth, (e) end of orthodontic treatment
PI was determined from the mesial, distal, buccal and lingual surfaces.
The depth of the periodontal pocket was also determined at six points: distolingual (DL), lingual (L), Mesiolingual (ML), Distobuccal (DB), Buccal (B) and Mesiobuccal (MB) using a William probe in mm. In addition, the height from the apex of the papilla to the cutting edge was measured (in mm) with a graduated probe to compare this indicator in adjacent teeth. Then targeted radiographs were taken. To achieve the correct position of the film, a silicone holder is made for each patient based on the occlusal component. The film was positioned parallel to the length axis and perpendicular to the source with a dosage of 40 Kvp. On the radiograph, a line (Tooth Crest point, TC) is drawn perpendicular to the root from the highest point of the bone crest (BC). The distance between TC and BC shows the width of the bone defect (DW). Then a line is drawn from BC to the point of greatest bone defect. The distance between the TC and the bone defect (BD) indicates the depth of the defect (DD). To measure root length (RL), a line is drawn from the inferior border of the root to the inferior border of the cemento-enamel junction (Figure 2).
Figure 2: The most superior border of the bony crest is defined as point BC. The point formed by drawing a perpendicular line to the root from the BC is defined as the ridge-tooth (TC) point. The point formed when drawing a line from the BC to the deepest zone of the bone defect is determined by the BD point. The measurement from the inferior border of the root to the inferior border of the cemento-enamel junction is recognized as root length.
Measurements were taken three and six months after completion of orthodontic treatment, while data were statistically analyzed using repeated measures ANOVA and Bonferroni at 0, 3 and 6 months after orthodontic treatment. P<0.05 was accepted as statistically significant.
results
The average and standard deviation of PI 27.39 + -8.75% at the end of orthodontic treatment (T0) decreased to 17.63 + -4.57% by the third month (T3) and by the 6th month (T6) it became 11.8 + -2.59 %. Changes in plaque levels were found to be statistically significant during the study period. Moreover, changes in PI were also detected in the interval between the end of treatment (T0), the third month (p = 0.032) and the sixth month after treatment (p = 0.022), which was also found to be statistically significant.
The mean and standard deviation of periodontal pocket depth were determined to be 1.93+-0.9 mm, 1.79+-0.87 mm and 1.7+-0.85 mm at T0, T3 and T6, respectively. A statistically significant difference was found between pocket depth at T0 and T3 (p=0.042), T0 and T6 (p=0.039) and T3 and T6 (p=0.047)
The average distance between the cutting edge and the apex of the papilla was 5.97 +-0.44 mm at T0, 5.99 +-0.42 mm at T3 and 5.97 +-0.33 mm at T6 without statistical significance (p=0.932)
In addition, the average depth of the bone defect was found to be 2.5 + -0.46 mm at T0, 2.34 + -0.54 mm at T3 and 2.09 + -0.7 mm at T6. The reduction in depth was found to be statistically significant at the segments T0 and T3 (p = 0.0432), T0 and T6 (p = 0.039) and T3 and T6 (p = 0.035).
A significant difference was also found between T0 and T3 (p=0.042), T0 and T6 (p=0.039), the width of the intraosseous defect (2.15+-1.11 mm, 1.9+-1.11 mm and 1.9+-1.11 mm, respectively), at stage T3 and T6 the difference was found to be statistically insignificant (p=0.59).
The root length remained unchanged throughout the 6 months, no statistically significant changes were recorded (p=0.95).
Discussion
In cases of aggressive periodontitis with intraosseous defects that led to tooth migration, regenerative treatment was applied. Since periodontal tissue therapy is unable to eliminate the destruction that has occurred due to pathological occlusion, especially leading to the elimination of the gingival papilla, orthodontic treatment is decided to be carried out for the intrusion and alignment of the involved teeth. The stability of the result is also important due to the extensive bone destruction, while data on long-term results are not yet available. In addition, patients may perceive the removal of devices as the final stage of treatment, omitting the retention phase. In the presented clinical case, all periodontal parameters were obtained precisely in the retention phase with reorganization of the periodontal ligament after removal of all equipment.
Some studies have reported side effects of orthodontic treatment in patients with aggressive forms of periodontitis with a history of extrusion of the anterior teeth. Such effects include failure of mechanical plaque removal after treatment, possible conversion of supragingival to subgingival deposits, destruction of periodontal tissues after therapy, and increased destruction of soft tissues in such patients. In such situations, for successful treatment of patients with vertical periodontal defects, we recommend the use of light orthodontic forces, as well as regular plaque control with follow-up visits within 3-6 months.
In the presented clinical case, patients were fitted with fixed orthodontic retainers. These retainers allowed physiological movements and also led to improved periodontal tissue, bone restoration and the prevention of unnecessary movements. In addition, these devices do not require ideal doctor-patient cooperation and do not violate aesthetics. If the clinical situation requires orthodontic and periodontal treatment, then the retention and stability of both approaches must be taken into account. Although many researchers insist on the importance of stability and retention, there is still limited data on long-term outcomes.
PI was constantly decreasing over the entire 6-month period, which may be due to the simplification of hygienic care after removal of the appliances and straightening of the dental arch. The same data were obtained by Re; before the removal of the equipment, the effectiveness of oral hygiene is very limited, which explains the large difference in PI between the periods T0, T3 and T6. In addition, the reduction in plaque accumulation between T3 and T6 may be associated with the use of a modified bass brushing technique, which is the most effective mechanical method of plaque removal. It is also obvious that the patient, observing good treatment results, will try to maintain them in the future.
A significant reduction in the depth of the pathological pocket at stages T0, T3 and T4 is also associated with the removal of the equipment and the use of a new modified cleaning method, which leads to simplified hygienic procedures, effective plaque removal, reduction of pathogenic microflora and improved gum condition. The direct relationship between PI and periodontal pocket depth is consistent with studies reporting reduction in sulcus depth and attachment restoration following reduction in PI and inflammation.
Significant improvement in the condition of periodontal tissues also occurred with the combined use of surgical methods and the use of antibiotics. These studies indicate a reduction in the inflammatory process and pathogenic population as a harbinger of a reduction in the depth of the periodontal pocket. Zhu showed that all patients with aggressive forms of periodontitis under 40 years of age experienced a reduction in pocket depth after intrusive therapy. Although stability of pocket depth remains after treatment and over the next year, as shown by Re, according to Melsen, the reduction in depth is associated with the formation of new connective tissue after the cellular activity of the periodontal ligament is activated and the space is closed by cells on the tooth surface. Passanzaei interprets the increased activity of connective tissue as a result of more active division of mesenchymal tissue compared to epithelial tissue. However, some reports deny the role of new connective tissue in reducing probing depth after orthodontic treatment.
Despite the reduction in the depth of the periodontal pocket, our studies could not find a difference between the new connective tissue and the junctional epithelium, since this procedure requires histological samples, which in this situation were impossible to obtain (however, based on observations and x-rays, it can be assumed that the formation new connective tissue).
There was no significant difference in the distance between the gingival papilla and the incisal edge at all stages T0, T3 and T6. This relationship is influenced by stable relationships with neighboring teeth, stable results of orthodontic treatment and the absence of recession. Similar to our studies, Re also did not reveal recession, external changes, or improvement in the condition of periodontal tissues throughout the entire year after treatment in patients with aggressive forms of periodontitis who underwent intrusion therapy and fixation of retainers. However, Levin considers retainers to be the cause of gum recession due to limited hygiene control, and as a result of observations in the period 4-40 months after treatment, 50% of retainer loosening was observed.
Root length remained stable at T0, T3 and T6 according to radiographic images. When tooth intrusion was performed using light orthodontic forces, no root resorption was observed. The forces during intrusion are concentrated at the apex and surrounding bone, while affecting the bone defect to a lesser extent, the risk of ischemic necrosis is reduced, and the cells of the periodontal ligament are activated. On the other hand, there is evidence of signs of root recession during the active phase of orthodontic treatment as a result of the natural mechanism of intrusive forces, which are associated with the conical characteristics of the anterior teeth and the concentration of force at the apex. Ischemic necrosis of the ligament, as well as a small elimination of pericementum, cementoblasts and denticlast colonies may be a consequence of this mechanism.
The present study also revealed a significant reduction in the depth and width of the bone defect, with a particularly pronounced reduction in width occurring between T3 and T6. Increased bone formation during orthodontic movement is confirmed by various mechanisms, for example, tension of the periodontal ligament, which acts as a natural barrier to epithelial cells (Guided Bone Regeneration), as well as increased bone formation with the participation of periodontal ligament cells, the effect of orthodontic forces is here the first impetus in the process of osteogenesis , which also begins in areas of defects. After orthodontic treatment, a reduction in intraosseous defects was observed on x-ray images. In addition, eliminating the swaying phenomenon with the help of retainers allows you to reduce the inflammatory process and reduce the activity of pathogenic microflora, which is extremely important in the formation and mineralization of new bone. In addition, orthodontic treatment may result in widening of the periolontal gap with decreased bone remodeling. Once orthodontic therapy is stopped and the force is eliminated, the periodontal ligaments return to their normal state. Thus, the reduction of bone defects is also caused by changes in the structure of periodontal structures.
The stable defect sizes at T3 and T6 can be interpreted as complete bone mineralization at T3, suggesting that the periodontal space and ligament structure also returns to normal size during this period.
However, the authors argue that observations of long-term results are also necessary for full conclusions.
Conclusion
Based on the limited research conducted, we can conclude that it is possible to achieve stable treatment results through regular observation and control of oral hygiene in patients with aggressive forms of periodontitis. The peculiarity of the treatment plan for this category of people is an integrated approach to the management of periodontal and orthodontic pathologies.
Authors: Afshin Khorsand , Departments of Periodontology Mojgan Paknejad , Departments of Periodontology Siamak Yaghobee , Periodontology and Dental Implant Research Center Amir Alireza Rasouli Ghahroudi , Periodontology and Dental Implant Research Center Hourieh Bashizadefakhar, Oral and Maxillofacial Radiology, Dental Faculty, Tehran University of Medical Sciences , Tehran Masoomeh Khatami , Department of Pediatrics Dentistry, Jondishapour University, Ahvaz Mohsen Shirazi , Department of Orthodontic, Dental Faculty, Tehran University of Medical Sciences, Tehran, Iran
Stages of prosthetics using implants
After preparing the oral cavity, classic one-stage or basal implantation is performed. The first option involves immediate installation of an implant after tooth extraction. Then the abutment is screwed onto it and a crown or prosthesis is put on. The procedure is different in that it does not require an incision in the gum and detachment of the periosteum; a small puncture is sufficient. After six months, instead of a temporary crown, a permanent crown is fixed; during this period, the implant should take root.
If the tooth has been removed a long time ago, tissue volume is increased or the basal implantation method is used. It lies in the fact that the artificial root is not implanted in the place of the previous one, but where there is enough tissue volume, that is, in a deeper layer (basal). Likewise, it requires no incision, just one puncture. This type of prosthetics is used most often when several adjacent teeth are missing. Immediate load on the bone will improve blood supply to the tissues, which will have a beneficial effect on periodontal diseases.