- Caries
- Pulpitis
- Stomatitis
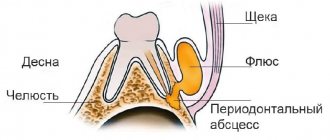
- Flux
- Gingivitis
- Tooth cyst
- Wedge-shaped defect
- Periodontal disease
- Periodontitis
- Periodontitis
- Causes of bad breath
- Signs of pulpitis
- Treatment of dental cyst
- Chronic periodontitis
Periodontitis – inflammation of the periapical (surrounding the root) tissues of the tooth – is a fairly “popular” dental disease.
In terms of frequency of occurrence, it is surpassed only by caries and pulpitis. The dynamics of the symptoms of this dental disease look like this:
- The appearance of aching pain associated with a specific tooth;
- The appearance of bad breath;
- Acute attacks of pain, becoming more pronounced when touching a tooth;
- Swelling of the gums around the affected periodontal area;
- Complication of chewing function - it is difficult for the patient to take not only hard food, but even drink;
- Formation of a fistula through which pus escapes into the oral cavity.
Many patients ignore the initial symptoms of the disease and self-medicate. But independent treatment of periodontitis is extremely incorrect: pain relief with medications, heating and rinsing with herbs will only lead to the fact that the symptomatic picture will be blurred.
An advanced disease is extremely dangerous: the pus that accumulates in the sac at the apex of the root may not find a way out, and the infection will begin to spread to other organs through the muscle tissue.
What is periodontitis?
We can easily notice changes in the appearance of teeth and the appearance of carious lesions on the enamel at home, limiting ourselves to one visual examination of the oral cavity. But things are completely different when you need to know the condition of the pulp. The pulp is the heart of the tooth, which is hidden from prying eyes. To see it, you need to undergo an x-ray examination by a dentist. The same applies to the root and basal tissue of the tooth; their diagnosis is carried out only using an x-ray. Inflammation of the periodontal tissues can be fraught with dangerous consequences; if the infection penetrates deep into the tooth and goes beyond the root canals, a person may lose the tooth.
Reasons for installing a crown
A crown is a kind of cap that is placed on a tooth, covering and protecting its tissue. Installed in three cases:
- If the natural crown of the tooth is destroyed by more than half and it is impossible to restore it with filling material or other restoration methods;
- To improve the aesthetics of the dentition - correct the shape of the tooth, hide visual flaws;
- When using prosthetics using a bridge. In this case, crowns are placed on the supporting teeth.
A crown can only be installed on a tooth with an intact root. If the upper part is significantly destroyed and the carious process has reached the pulp, before installing the crown, the tooth is depulped and the root canals are filled.
When installing a bridge, the supporting teeth are covered with dental crowns, even if they are not destroyed. If the tooth is relatively healthy, the dentin and pulp are not affected, crowns can be installed without depulpation.
Our clinic’s specialists do not recommend that patients install bridges, but offer alternative types of prosthetics if the supporting teeth are healthy. To place a crown, the doctor must prepare (grind) the tooth, that is, completely remove the enamel. Without a natural protective layer, even if covered with a crown, the tooth becomes vulnerable and gradually collapses. A bridge should only be placed on teeth that have “nothing to lose.”
Reasons for the development of periodontitis.
When caries begins, pathogenic bacteria begin to actively multiply and if the disease is not cured in a timely manner, the inflammatory process spreads to the enamel and affects the dentin. When the infection reaches the pulp, a complication of caries develops. It is untreated pulpitis that causes periodontitis. Once in the periodontium, the infection begins to irritate it, causing its response. This is how our body reacts to problems: the patient may experience increasing pain, which is localized and sometimes becomes completely unbearable.
It should also be noted that the formation of periodontitis is also possible under other conditions:
Poorly sealed canals.
When filling, it is important to fill the root canals tightly and correctly with the material, and for this it is necessary to determine their size using radiography. If the dentist skipped this stage and did not fill the canal, inflammation may begin in the remaining space.
Mechanical injury to the jaw or teeth.
Very often, periodontitis occurs in children, because... Little fidgets constantly fall, and sometimes they can hurt their faces, you should pay attention if your child, after such an active walk, begins to complain of severe tooth pain.
Development of infection under the crown.
In this case, periodontitis occurs due to the incompetence of the doctor, or he incorrectly carried out the preparation stage and poorly processed the tooth and filled it, or an error was made when placing the crown, and the dentist did not remove the dead pulp.
Use of arsenic.
Previously, arsenic was used to kill the pulp, if the dose is incorrectly determined and with its long-term effect on the body, there is a high risk of an inflammatory process in the periodontal area. Currently, dentists use high-quality anesthetics that allow them to treat and remove the pulp without exposure to arsenic paste.
Use of antiseptic drugs.
One of the main reasons for the development of drug-induced periodontitis is the excess concentration of drugs during filling and treatment of root canals.
Prevention
To reduce the risk of disease, it is important to follow simple rules:
- maintain oral hygiene,
- visit the dental office twice a year,
- perform prosthetics only by a qualified implantologist,
- Carefully care for the crown, prosthesis or bridge structure.
A wide range of services for the prevention and treatment of periodontitis under the crown and other diseases is offered by dentistry on Vernadsky. Our specialists will conduct an accurate diagnosis and eliminate the cause of the disease.
The use of modern equipment and new anesthesia drugs eliminates pain during the treatment process. Pre-registration for an appointment is by phone.
Symptoms and signs of periodontitis.
As mentioned earlier, periodontitis may not manifest itself for a long time; the patient runs the risk of finding out about the disease too late, when it has entered the acute stage. In this case, the signs of inflammation of periodontal tissues will be felt much more clearly. Periodontitis is characterized by the following symptoms:
Deterioration of general condition.
There is an increase in temperature, worsening sleep, weakness, etc.
- Pain when chewing food and when closing the jaws.
- Change in gum color (become darker).
Based on this symptom, periodontitis can be identified in its initial stages of development. Also, the periodontal tissues may swell, and the swelling may spread to the cheek and neck.
Painful sensations.
In the acute course of the disease, the patient begins to be bothered by a sharp, aching pain that radiates to neighboring teeth.
- Slight tooth mobility.
- The appearance of bad breath.
- Increased sensitivity due to mechanical impact on the tooth.
When a tooth hurts under the crown...
It is generally accepted that to treat a tooth, it is necessary to remove the crown. But high-quality dentures are not cheap, and they are not suitable for reuse. Therefore, it is doubly unpleasant when pain appears several months after prosthetics, and it becomes necessary to remove a crown that has not served its purpose.
In this case, patients often put off a visit to the dentist with all their might. For example, they take painkillers and antibiotics or experiment with very dubious “folk” methods. But by self-medicating, you will not solve, but will only aggravate the problem, since advanced inflammation is much more difficult to treat. If discomfort or pain occurs, you should immediately visit your dentist. Moreover, contrary to popular belief, modern treatment methods, in some cases, make it possible to do without removing the crown.
In some cases, treatment is possible without removing the crown.
Types of periodontitis.
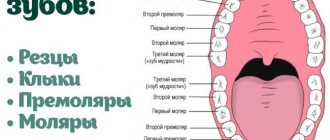
There are several classifications of periodontitis; it is usually distinguished by the place of formation: apical (infection affects the base or apex of the root) and marginal (occurs in the area of the gum edge due to injury).
According to the nature of the course of the disease, the following stages are distinguished:
Acute periodontitis.
It is further divided into several forms: serous acute periodontitis is the initial stage of the development of inflammation; it occurs after the infection penetrates through the apex of the tooth root into the periodontal area. Then it develops into purulent acute periodontitis. This form of the disease is very dangerous because The pus penetrates the bone structures and can spread throughout the body. It is characterized by: severe increasing pain, painful sensations when pressing on the tooth and when biting, headache, swelling of the mucous membrane, etc.
Chronic.
It has three stages of development: fibrous, granulating and granulomatous. Chronic periodontitis is characterized by a calm and even imperceptible course of the inflammatory process; only sometimes the patient may experience slight pain when tapping a painful tooth. But at the same time, this stage is considered the most dangerous, because may lead to tooth loss. With the development of the granulating form, the unit and the tissues around it are destroyed. A fistula forms on the gum, from which pus flows. Granulomatous periodontitis is characterized by the formation of a granuloma, a sac filled with purulent fluid, which subsequently develops into a cyst if not removed. Tooth mobility increases, gums bleed, and abscesses develop.
Types of complications with fixed dental prosthetics
The most common types of complications encountered with fixed prosthetics are:
Stomatitis and gingivitis (inflammatory processes of the gums)
Stomatitis and gingivitis
This type of complication mainly arises from improper grinding of teeth; this concerns preparation without the so-called ledge on which the lower part of the crown sits and in no case should it hang over the tooth or be pressed into the gum. The second reason may be a very massive intermediate part of the bridge, which puts pressure on the gum. Accompanied by cutting pain, redness and swelling in the pressure area. It would also be incorrect to consider too large or too small a space between the intermediate part and the gum - the rinsing space; this will lead to the accumulation of food debris and bacteria, which will ultimately cause an unpleasant odor and an inflammatory reaction. The presence of sharp edges of bridges and individual crowns can provoke chronic injury - rubbing of the tongue and cheeks . In case of any inflammatory phenomena of the oral mucosa after prosthetics, you should consult a doctor. As anti-inflammatory therapy, you can use various gels, for example Metrogyl Denta, as well as various herbal decoctions and extracts, for example Rotokan.
Dental diseases under dentures (caries, pulpitis, periodontitis)
It is important to understand that all orthopedic structures are fixed either to completely healthy teeth or to teeth prepared in advance for prosthetics. In case of insufficient diagnosis or improper preparation of the oral cavity for prosthetics, complications such as caries under the crowns, pulpitis or even periodontitis may occur. A pathological process that goes undetected in time will ultimately lead to tooth extraction. Periodontitis can also be caused by non-compliance with certain rules when planning the structure, for example, if a bridge is too long in length or a crown that is too high, which will lead to overload of the tissues that hold the tooth in the bone.
Periodontitis (inflammatory processes of all tissues surrounding the tooth)
Periodontitis
The most important cause of periodontitis in fixed prosthetics is the preparation of teeth without a ledge. As a result, the dental technician will not be able to make the correct crown on the model. It will definitely hang over the tooth and cement will remain under the overhanging edge during fixation, which will provoke a pathological reaction and it is not possible to remove this cement from there without damaging the structure. This is manifested by cyanosis of the gums, swelling and bleeding , followed by recession, darkening and exposure of the gray edge of the crown. Naturally, aesthetics are also compromised.
The choice of design depends on many factors, such as the general condition of the body, gum biotype, length of the defect, etc. If all conditions are not taken into account sufficiently, an inflammatory reaction of all tissues surrounding the tooth may occur, which will lead to rapid atrophy of the bone around the affected tooth and, accordingly, its loss. To prevent this complication, an odonto-periodontogram is often performed before prosthetics, which is a graphical recording of the condition of the periodontium and the degree of atrophy of its tissues. Odontoparodontogram during prosthetics helps to choose the correct design of the prosthesis and determine the number of supporting teeth.
Allergic reactions to materials used in prosthetics
Allergic reactions to materials used in prosthetics.
Mainly allergies after orthopedic treatment when an artificial prosthesis comes into contact with the gums and can manifest itself locally in the form of gingivitis with symptoms such as redness and rashes on the oral mucosa, burning and dryness in the mouth, or more general ones. reactions of the body, such as a rash on the skin of the face , swelling, an attack of bronchial asthma. Such reactions can appear either immediately or several hours or even days after installation of the prosthesis. Any allergic reaction during prosthetics requires analysis of the cause and subsequent treatment.
Galvanic syndrome
Such a reaction as galvanism requires special consideration. It manifests itself in the presence of various metals in the oral cavity, and this only happens on exposed metal and does not apply to dentures lined with ceramics. When saliva enters, which acts as an electrolyte, the metals acquire different potentials, resulting in the formation of galvanic currents. Symptoms of this complication are a metallic taste in the mouth, dryness, burning, headaches, sleep disturbances, and local darkening of metal dentures is possible. When galvanism is detected, it is necessary to replace all metal structures with prostheses made of more bioinert materials .
Cementation and loosening of a fixed structure
Dental cements on which permanent structures are fixed must meet certain requirements. However, sometimes de-cementation (“unsticking”) of the permanent structure occurs. This can occur from excessive load, an incorrectly ground tooth, a bridge that is too long, expired or insufficient cement for fixation, as well as one large or several small fillings on a tooth that fly off while remaining in the crown.
Chips of the lining of artificial teeth and crowns
Chips in the lining of artificial teeth and crowns
The lining of crowns and artificial teeth consists of porcelain, this material is beautiful and strong, but if overloaded, it cannot withstand deformation and chips. The cause may be an error in the planning of the orthopedic design, a technical error in manufacturing, as well as the patient's frequent consumption of too hard foods, such as nuts and bones. Sometimes chips can be restored without removing the orthopedic structure, right in the oral cavity, but only the attending physician can resolve this issue.
Malocclusion due to crowns and teeth that are too low or too high
In the case of too low clinical crowns, the efficiency of the chewing function will be quite low, and in the case of too high crowns, the entire masticatory apparatus . Malocclusion sooner or later causes even more serious disorders of the temporomandibular joint, as well as neurological disorders, which can often be expressed in the form of headaches. If the patient feels that he is not grinding food tightly and too large pieces of food remain, or feels pain in the joints after prosthetics, he should immediately consult a doctor to correct the bite.
Violation of the plane during prosthetics
For any prosthetics, the so-called occlusal plane is very important. By it we mean a plane passing through the cutting edges of the central incisors and the distal cusps of the seventh teeth separately for the upper and lower jaws. Incorrect prosthetics can lead to disruption of this plane and disruption of the movements of the temporomandibular joint. This often manifests itself with serious adverse consequences in the form of facial and headaches, pain in the joint area, and clicking when opening the mouth. Such errors require long and careful treatment. In this case, in-depth gnathological studies will be needed, which are carried out in our clinic. Gnathology examines the interaction of all organs of the dental system and affects many factors. Today, much attention is paid to the development of gnathology and neuromuscular dentistry.
Fractures of bridges and crowns
Fractures of bridges and crowns
Fractures, as a rule, can occur in those fixed prostheses that cannot withstand excessive load, as well as due to technical errors: too thin a frame or a very narrowed part. This complication mainly applies to stamped-soldered and temporary plastic structures. Stamped-brazed structures today are practically replaced by prostheses made of stronger materials. And replacing temporary plastic ones, if necessary, is practically easy and does not take much time.
Treatment of periodontitis.
During the examination, the dentist will determine the degree of development of periodontitis, and the treatment plan will depend on this. Making a diagnosis is not difficult; upon visual examination of the oral cavity, one will notice severe destruction of the tooth structure, a change in the color of the gums, and there is no reaction to cold and hot water. Eliminating the consequences of inflammation of periodontal tissue can take quite a long time; you will have to visit the doctor several times. Several years ago, such a diagnosis forced doctors to remove the damaged tooth, but now the patient has the opportunity to maintain the integrity of the dentition and get rid of the inflammatory process.
Treatment of periodontitis is possible in several ways; if therapeutic methods are not effective, the dentist uses surgical intervention. Let's take a closer look at the stages of treatment:
Treatment of a damaged tooth.
First, it is necessary to open access to the root canals, remove softened dentin and remnants of infected tissue. This procedure is performed using a special bur, after which the cleaned cavity is treated with antibacterial drugs. Then the tooth canals are widened, washed with antiseptic solutions and the medicine is placed in them. Until the inflammation is stopped, the doctor has no right to proceed to the next stage.
Filling.
At the end of the treatment, the root canals are tightly filled. In most cases, these actions are enough to get rid of inflammation, the microflora of the tooth is normalized, and its tissues are regenerated.
This treatment option is a conservative method; surgical intervention is performed according to a different plan:
The operation is performed under anesthesia. In the area where the granuloma is located, an incision is made into the mucous membrane and periosteum, resection of the root apex is performed and the purulent neoplasm is cleaned out. The wound is washed with antibacterial drugs, disinfected, and sutures are applied.
If the patient's periodontitis is in the last stages of development and treatment does not have a positive effect, then a decision is made to remove the tooth.
Materials for making crowns
Modern dental crowns are made from:
- Metal.
Metal dentures are considered obsolete due to their lack of aesthetics, but are still used because they are the cheapest option; - Metal ceramics.
A relatively inexpensive and durable option, but due to the metal base it is difficult to achieve a “healthy” whiteness of an artificial tooth; - Ceramics.
Ceramic crowns are more aesthetically pleasing than metal-ceramics, but are inferior in strength, so they are usually installed only on the front teeth; - Porcelain.
A type of ceramic crown. Porcelain dentures are indistinguishable from living teeth, since the optical properties of the material are almost identical to tooth enamel. They are also installed on the front teeth; - Zirconia.
They are made on the basis of zirconium dioxide and covered with ceramics on top. Durable, aesthetic, but quite expensive crowns.
Zirconium dentures can be installed on any tooth.
The material, contrary to popular belief, does not cause toothache, but may be the answer to the question of why the gums hurt after installing a crown. Inflammation of the mucous membrane and gums can cause an allergic reaction to the metal in a metal-containing crown. Patients with ceramic and zirconium prostheses do not encounter such problems.
Possible problems
Treating toothache under a crown is often fraught with problems. Among them:
- The crown is installed on a pin, which must be removed during treatment. This may lead to perforation of the root, which can lead to its fracture and subsequent root removal;
- the canals are filled only after the previous filling has been completely removed, which often causes root perforation;
- After cleaning the old filling, it is necessary to undergo a course of treatment with anti-inflammatory drugs and only then can a new crown be installed.
Treatment methods in our clinic
In most cases, treatment is radical and consists of the following steps:
- Removing the old crown.
- Complete removal of old filling material.
- Eliminate the source of inflammation.
- Taking a course of anti-inflammatory therapy, which can last 2-3 months.
- Canal filling.
- Installation of a new crown.
Such therapy often costs more than conventional prosthetics.
Dental treatment under a crown
If the source of inflammation is located at the top of the root, then it is quite possible to perform a tooth root resection. It involves removing the source of pus through an opening in the bone tissue. The option is very convenient, because you do not have to undergo long-term therapy and install a new crown. However, it is not always available. This operation lasts no more than an hour and its big advantage is that it is non-traumatic.
Treatment with medications and herbal medicine
Situations where a tooth hurts under a crown, but there is no way to quickly visit a doctor, are not uncommon. In such cases, you can slightly reduce the pain by using various medications. Among them:
- non-steroidal anti-inflammatory drugs - will reduce pain and relieve inflammation, but they cannot be taken for a long time;
- lotions using hydrogen peroxide;
- rinsing with a soda solution of 1 tsp. baking soda diluted in a glass of water.
Similar medications are prescribed after surgery to alleviate the patient’s condition and reduce pain. In addition, herbal preparations, for example, a decoction of calendula, sage, thyme, as well as chamomile or oak bark, will help reduce pain. They are used as a mouth rinse.