With a decrease in the density of the bone tissue of the jaw, various dental pathologies develop, which contribute to the destruction of dental units with subsequent removal. To restore the functionality and aesthetics of the dental system, prosthetics are necessary. Many patients are interested in the question of whether dental implantation can be performed for osteoporosis. There is no direct contraindication to the procedure in this case. Some doctors, on the contrary, recommend the implantation of titanium roots, since this triggers regeneration processes and the bone becomes denser.
Indications and contraindications
With the help of implantation, you can restore a lost dental unit, replace a destroyed tooth that is subject to removal, restore a dental segment or a complete row in case of multiple edentia. It is performed on the upper and lower jaws.
If the patient’s medical history includes a diagnosis of osteoporosis, the doctor makes a decision regarding the possibility of implantation after a thorough diagnosis. For this purpose, a 3D computed tomography is performed. On it you can examine the condition of the jaw bone from any angle and layer by layer. Using a three-dimensional image, the doctor assesses the degree of development of the disease, bone tissue atrophy, and mineral composition.
In the list of contraindications:
- tuberculosis;
- bleeding disorders, blood diseases;
- malignant tumors;
- bruxism;
- mental disorders;
- severe vascular and cardiac pathologies;
- venereal diseases;
- pathological bite;
- acute infections;
- exacerbation of chronic diseases;
- alcoholism, smoking, in which the patient cannot give up cigarettes for a long period;
- pregnancy, lactation;
- exacerbation of chronic diseases;
- low level of immunity.
Some contraindications are temporary and surgery becomes possible after they are eliminated.
Impact of osteoporosis on teeth
Naturally, osteoporosis is not only a problem for teeth, but also for the whole body. In relation to dentistry, bone depletion has a very detrimental effect on periodontal tissue, and this is especially negatively manifested on the gums.
To study the role of osteoporosis in dentistry, an experiment was conducted in a clinical setting in which middle-aged and elderly women (all with periodontitis) participated. The study included x-rays, measurement of root exposure, determination of the degree of bleeding and a number of additional physiological factors.
In patients without osteoporosis, periodontal disease had a milder form, in contrast to women with bone depletion. The latter had severely exposed tooth roots - large periodontal pockets.
The results of the experiment showed that treatment and preventive measures for osteoporosis can greatly influence the condition of the oral cavity.
In other words, in order to avoid the development of periodontitis and not lose teeth, you need to treat osteoporosis. Moscow metro station Zvezdnaya, Danube Avenue, 23
Implantation methods
Depending on the clinical picture, implants can be implanted using two-stage or one-stage treatment protocols. The latter are preferable because the screws can be installed at an angle, which provides greater coverage of the bone tissue, which means the system will be better stabilized.
With the classical method, an implant is first installed, and prosthetics are performed on average six months later. The operation is performed with dissection of the gums and suturing, that is, it is highly traumatic. Bone augmentation is almost always carried out. Bone grafting also requires a recovery period.
One-stage treatment protocols allow you to restore teeth in one stage, without blood and stitches, since micro-punctures are made in the gums to introduce an artificial root. A minimally invasive procedure is more comfortable for the patient, and the recovery period is easier.
One-stage implantation methods:
- installation of an implant immediately after tooth extraction - one-step;
- restoration of a tooth segment or a complete row - basal;
- treatment of complete edentia - All-on-4 or All-on-6 protocols.
The doctor decides which method to choose after diagnosis.
Symptoms of osteoporosis
Osteoporosis is an insidious disease in its own way. It begins to develop without obvious symptoms. In most cases, osteoporosis is diagnosed only during examination of a fracture.
A fracture in osteoporosis is a complication indicating significant destruction of bone tissue. Let's say a person stumbles and falls. With healthy bone tissue, a fracture due to a simple fall is unlikely. With osteoporosis, any fall or injury can lead to a fracture. The most vulnerable are the femoral neck, arm bones, wrist, and spine. A vertebral fracture in osteoporosis can occur simply from heavy lifting or bumpy driving.
Until a fracture has occurred, the manifestations of osteoporosis are usually interpreted as symptoms of osteochondrosis, especially since osteochondrosis is its usual companion. These symptoms are often ignored, which should not be done.
Osteoporosis may be indicated by:
Back pain
Osteoporosis can manifest itself as pain in the lumbar or thoracic spine during prolonged static load (for example, if you have to sit all day long).
Convulsions
With osteoporosis, leg cramps may occur at night.
More about the symptom
Slouch
With osteoporosis, stooping and decreased height are observed due to a decrease in the height of the vertebrae.
Parodontosis
The consequence of osteoporosis can be periodontal disease - a non-inflammatory lesion of the periodontium (periodontal tissue).
Implantation stages
Regardless of treatment protocols, the procedure is performed sequentially. The classic correction method takes a lot of time, and all manipulations using single-phase methods can take only a few days. This period includes diagnostics, surgery to install titanium roots, and prosthetics.
Preparing for implant installation
At the initial appointment, the doctor collects anamnesis, examines the oral cavity, and conducts a computed tomography scan. The patient undergoes blood and urine tests to exclude general contraindications. You may need to seek permission from your physician.
If one or more implants are installed, professional hygienic cleaning of the oral cavity from dental plaque is carried out. When dental diseases (caries, gingivitis, etc.) are detected, appropriate treatment is first carried out.
After diagnosis, the dentist chooses a method of restoring the dentition, implantation systems. If complete edentia is treated with one-stage protocols, then 3D modeling of the result is carried out, and surgical templates are printed.
Performing implantation
The procedure is carried out in stages:
- pain relief with local anesthetics;
- preparing a bed for a titanium root;
- screwing the implant into the bone.
If the tooth is previously removed, the prosthesis is installed on the same day. In this case, special systems are used that can be installed directly into the hole.
The final stage is prosthetics
In the immediate loading protocol, temporary crowns are installed within three days. The permanent prosthesis is installed after at least six months. Some temporary orthotic systems can last up to several years.
With delayed loading, prosthetics are done after the implant has completely healed. In this case, a permanent crown is immediately placed.
What to do if you have periodontitis
If the diagnosis is confirmed, the disease must be treated. How dental periodontitis is treated depends on the form and stage of inflammation. The correction program may include therapeutic and surgical techniques.
Conservative therapy
Conservative methods are aimed at maximizing the preservation of the structure of the unit and restoring its functionality. The program includes elimination of the source of inflammation and endodontic treatment. All manipulations are performed under local anesthesia. Treatment regimen:
- Conducting anesthesia.
- Opening the crown, providing access to the root canals.
- Expansion of the cavity.
- Pulpectomy (if the segment has not been previously treated) or unfilling of the canals.
- Antiseptic, medicinal treatment of cavities.
- Temporary filling (for the period of anti-inflammatory treatment).
- Removal of temporary filling, filling of root canal.
- Restoration of the coronal part of the unit.
- Prescribing a course of antibiotic therapy.
Surgical intervention
Invasive methods are used when other methods are ineffective. The operation can be carried out using different protocols:
- Resection of the apex of the tooth root followed by filling the cavity with special bone-forming materials.
- Extraction of the diseased segment.
If periodontitis is not treated, complications are possible: odontogenic periostitis (inflammation of the periosteum), abscess, phlegmon, etc. The infectious process spreads to nearby lymph nodes, and lymphadenitis occurs. In severe cases, possible: tooth loss, osteomyelitis, sepsis.
Rehabilitation period
You should strictly follow your doctor's instructions. If antibiotics are prescribed, then you need to complete the recommended course. Pain can be relieved with analgesics, swelling can be relieved with a cold compress.
In the first two weeks, careful oral hygiene is important. It is necessary to carefully remove plaque with a soft toothbrush, use dental floss, and rinses. In order not to disturb the injured tissues, it is necessary to eat soft food at a comfortable temperature. It is not recommended to visit the sauna, take a hot bath, or sunbathe on the beach.
Smoking should be stopped for the entire recovery period until the osseointegration process is completed, approximately 4 to 6 months.
Treatment of periodontitis
If during caries microbes are found in the hard tissues of the tooth, during pulpitis - in the tooth cavity (pulp chamber) and root canals, then during periodontitis - they extend beyond the boundaries of the tooth root.
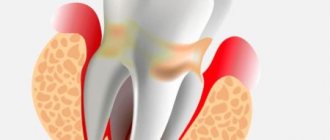
This complication is called periodontitis , i.e. periodontal inflammation. Periodontium - the ligamentous apparatus of the tooth - is the connective tissue that fills the narrow space between the tooth and the bone bed of the jaw (these are ligaments, nerves, blood and lymphatic vessels). The main functions of periodontal tissue are shock-absorbing and nutritional. When chewing food, the periodontium absorbs the load on the tooth and evenly redistributes it to the bones.
When a tooth remains untreated for a long time, there is a risk of a serious complication of caries - periodontitis. First, cariogenic microorganisms destroy hard tooth tissues (enamel and dentin), then penetrate into the pulp chamber, infecting the vessels and nerves located in it and causing pulpitis. When pulpitis is asymptomatic and is not treated for any reason, the inflammatory process deepens and, passing through the canals, extends beyond the root apex.
Periodontitis is an inflammation of the tissues surrounding the root tip. The periodontium itself is a complex of tissues located in the gap between the tooth root and the jaw bone. Behind the root, the infectious process creates a focus of increased pressure, which causes spontaneous pain in the tooth, which sharply intensifies when biting on it. Patients often complain of the feeling of a “grown tooth” or “lengthened root”. Sometimes on the gum, or less often on the skin near the causative tooth, a “swelling” occurs - a fistula, from which contents from the source of infection are periodically released. Under certain circumstances, periodontitis is asymptomatic, without causing pain or complaints; periodic exacerbations of the disease are possible. In any case, the infectious process causes rarefaction (loss) of the bone tissue behind the root, which ultimately leads to the formation of a large cavity in the bone tissue - a cyst.
- Penetration of infection from the root canal through the hole at the apex of the root: untimely treatment of caries or pulpitis;
- poor-quality root canal filling;
- incomplete elimination of foci of infection during the treatment of pulpitis;
According to the nature of the course, periodontitis is divided into acute and chronic.
Acute periodontitis is manifested by sharp pain in the tooth area, aggravated by touching it. Swelling of the lips, cheeks, gums is enlarged, the tooth is mobile. Sometimes there is a hole in the gum from which pus flows. This is a fistula, i.e. a channel that has formed to drain contents from an infected cavity.
Chronic periodontitis can manifest itself in the form of unpleasant and mild pain (feeling of heaviness, fullness, awkwardness, pain when chewing load on this tooth). Chronic periodontitis may not manifest itself for a long time and may be discovered by chance on an x-ray during the treatment of neighboring teeth.
The first measure in the treatment of periodontitis is to release the impurities that have accumulated behind the roots. To do this, it is necessary to remove the softened carious tissues of the tooth and go through the entire length of the infected canal. Typically, the patient then experiences immediate pain relief. Next, it is necessary to expand the root canal, which contributes to the rapid drainage of infection and recovery of the tooth. Rinses are prescribed, and medicine is placed into the diseased canal. When the inflammatory process behind the root subsides, the tooth canals are filled, after which the coronal part can be restored with a filling.
The photographs can be used to trace the dynamics of bone tissue restoration behind the root of a chewing tooth after high-quality endodontic treatment of periodontitis.