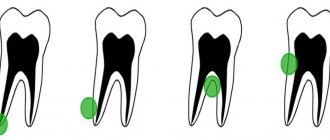
A dental cyst is a benign neoplasm that is located inside the bone tissue of the jaw, in the upper part of the tooth root. A cyst is formed by isolating pathological cells from healthy ones by a dense membrane. It protects the roots of adjacent teeth and the body from further spread of inflammation.
The diameter of the cyst is from 0.5 to 3 cm. A dental cyst is dangerous because it develops into a malignant tumor. It also provokes various consequences in the form of:
- damage to neighboring teeth;
- tooth loss;
- destruction of the bone tissue of the jaw.
What is a cyst? Jaw cyst
A cyst is a cavity that is lined with epithelium and filled with fluid or soft material.
The formation of teeth (odontogenesis) is a complex process in which connective tissues and epithelium (enamel organ, dental follicle and dental papilla) participate.
The enamel organ refers to an epithelial structure derived from the oral ectoderm. The dental follicle and dental papilla are ectomesenchymal structures, because they are partly derived from neural crest cells.
For each tooth, odontogenesis begins with the apical (affecting the tip of the tooth root) proliferation of the epithelium of the oral mucosa, known as the dental lamina. The dental lamina gives rise to the enamel organ, a cap-shaped structure that subsequently takes on the shape of a bell. After the formation of the enamel organ, the dental lamina cord usually fragments and degenerates. However, small islands of dental lamina may remain after tooth formation. They are believed to be responsible for the development of some odontogenic cysts and tumors.
The enamel organ has four types of epithelium. The inner lining of the enamel organ is called the inner enamel epithelium and becomes the ameloblastic layer that forms tooth enamel. The second layer of cells adjacent to the inner enamel epithelium is the intermediate layer. Adjacent to this layer is the stellate reticulum, followed by the outer enamel epithelium. The enamel organ is surrounded by loose connective tissue known as the dental papilla. Contact with the epithelium of the enamel organ causes the dental papilla to produce odontoblasts, which form dentin. As odontoblasts lay down dentin, they induce ameloblasts to form enamel.
After initial crown formation, a thin layer of enamel organ epithelium, known as Hertwig's root sheath, grows at the apex of the tooth root. This epithelial expansion later becomes fragmented but leaves behind small nests of epithelial cells known as Malassez remnants in the space of the periodontal ligament. They are the source of epithelium for most periapical (radicular) cysts, but do not cause any odontogenic neoplasms, with the exception of squamous odontogenic tumor.
Conservative treatment
This type of therapy allows you to be cured without surgery. In this case, an incision is not required to gain access to the tumor. At the initial stage of treatment, the dentist drills out and cleans out the affected root canal. The apex of the tooth root connects to the cyst, so once the root canal is opened, the contents flow out. After cleaning and disinfecting the root canal, the doctor introduces antibiotics and substances into the cavity that destroy its capsule.
After this, the doctor fills the resulting cavity with a special paste that will help restore bone tissue. The hole is then filled. If after 6 months the cyst is not detected on an x-ray, the treatment can be considered successful. This method helps in about 75% of cases.
An innovative treatment method without surgery
is depophoresis. It helps eliminate infection in all root canals without drilling them. The dentist exposes the mouth of the canal and inserts an electrode into it. Another electrode is pressed against the surface of the cheek, which produces a weak current discharge. Together with the discharge, copper-calcium hydroxide is passed through the root canal, which penetrates into all hard-to-reach areas, destroying all bacteria, microorganisms and dead cells.
After three sessions of depophoresis, the damaged tooth is filled and its crown is restored. Regardless of what type of tumor was detected, treatment with depophoresis allows you to get rid of it in almost 100% of cases.
Why do jaw cysts form?
Odontogenic cysts (developing or inflammatory) get their name from the nature of their origin. Most jaw cysts are lined by epithelium, which is derived from odontogenic epithelium.
The occurrence of such cysts is usually associated with unerupted teeth (third molars of the lower or upper jaw, second premolars of the lower jaw, and canines of the upper jaw). They can also form near additional teeth and in combination with odontomas. The occurrence of odontogenic cysts is rarely associated with baby teeth.
Most often, jaw cysts are discovered between the ages of 10 and 30 years. Men, especially white-skinned men, suffer from them more often.
In most cases, dental cysts do not manifest themselves in any way and are an accidental finding obtained during an X-ray examination. But, in some cases, they can reach significant sizes, which lead to the expansion of bone tissue, but even they may not give pronounced symptoms until a secondary infection occurs.
Removal of upper teeth
The bone of the upper jaw is somewhat softer than the lower jaw.
The units are positioned straighter and are easier for the surgeon to grasp. Therefore, removal of the upper molar in many cases is faster and less painful. Patients are often frustrated by the need to have their front teeth removed. The smile zone is always visible, so the absence of one brings a negative attitude and leads to a decrease in self-esteem. But today such an operation is not scary. There are every opportunity to quickly restore the integrity of the dentition.
Removing the front tooth on the upper jaw is simple - it has only one cone-shaped root and is located conveniently for manipulation. The operation will take about 20 minutes, including waiting for the anesthesia to take effect. If there are no contraindications, then simultaneous implantation is recommended - the destroyed unit is removed and an artificial root is immediately installed in the same hole.
Our clinics employ implantologists who are proficient in advanced techniques and have completed internships in foreign clinics. Only premium implants are used. Therefore, you will quickly gain a new beautiful smile. It is possible to install a temporary plastic crown on the pin on the day of removal. The front teeth will be in place, and no one will notice the changes.
Treatment from world-class doctors cannot be cheap, but we have found an opportunity to make help accessible - we treat immediately, and offer to pay for services in installments in convenient amounts, without charging interest.
Removing the upper root of a tooth is a more complex process. The root branch is drilled into several parts, which are removed step by step. This procedure for intervention is typical for molars and wisdom teeth, when the walls have completely crumbled and the root is also not viable.
How do jaw cysts appear?
In most cases, the cyst does not cause significant symptoms. Its development can be provoked by incorrect treatment of dental diseases or caries.
Odontogenic cysts are usually distinguished by type of origin:
· dentofacial cysts – their occurrence is associated with the crown of a tooth that could not erupt;
· keratocysts – are a consequence of Nevoid basal cell carcinoma syndrome;
radicular or radicular cysts – are of inflammatory origin and most often result from a reaction to necrosis of the dental pulp;
· bifurcation buccal cyst – typical for children 5-10 years old, it is formed in the area of buccal bifurcation of the first molars of the lower jaw;
· primary cyst – in most cases it is a keratocystic odontogenic tumor;
· orthokeratinized cyst – also refers to a subtype of keratocystic odontogenic tumor;
· eruption cyst – usually formed from a degenerating dental follicle and forms in the gum when the tooth erupts;
· newborn gum cyst – formed from the remains of the dental plate on the gum of a newborn;
· adult gingival cyst – is a variant of the lateral periodontal cyst;
· lateral periodontal – a non-inflammatory cyst on the side of the tooth, formed from the remains of the dental plate;
· calcifying cyst is a rather rare pathology, which is characterized by cystic and neoplastic signs;
· glandular cyst is a formation with a respiratory epithelial lining and potential relapse; in its manifestations it is similar to the central variant of poorly differentiated mucoepidermoid carcinoma.
Odontogenic cysts are difficult to detect at an early stage. It gives virtually no symptoms. The patient may be alarmed by tooth displacement or a change in the color of the diseased tooth. If the cyst has reached a significant size, the patient may notice protrusion of the bone structures.
A long asymptomatic course can lead to the formation of inflammatory processes, which are dangerous due to the development of suppuration and can provoke pathological fractures of the jaw bones.
If a cyst has formed in the upper jaw, it can cause nosebleeds, headaches and impaired nasal breathing.
The main symptoms associated with the presence of an odontogenic cyst (pain, fever, inflammatory changes in the oral cavity) usually appear in the later stages of the disease.
Causes of maxillary sinus cysts
Predisposing factors for the formation of a maxillary sinus cyst are:
- Individual anatomical and topographical features of the structure of the nasal cavity, which impede the free movement of air through the nasal canals (congenital deformities, deviated septum).
- Blockage of the excretory duct of the glands located in the mucous membrane of the paranasal sinus. This happens with frequent rhinitis, sinusitis, allergic rhinitis and polyposis.
- Inflammatory dental diseases with infection spreading to the root canals. The paranasal sinuses are separated from the roots of the molars and premolars by a thin septum, so infection from pulpitic or periodontitis teeth often causes an inflammatory process in the maxillary sinus.
- The formation of a dental cyst, which grows into the maxillary sinus and continues to grow inside it.
The maxillary cyst gradually grows larger, filling the sinus without pronounced clinical symptoms. The presence of a formation can be suspected during exacerbations caused by colds, acute respiratory viral infections, local hypothermia, and decreased immunity.
How are odontogenic cysts diagnosed?
The leading method for identifying odontogenic cysts is radiography, which is capable of visualizing jaw cysts at an early stage of their development. On an x-ray image, the cyst is distinguished by the presence of clear boundaries, and the formation itself gives a characteristic shadow of a round or oval shape, immersed in the sinus of the tooth root.
Ultrasound examination also helps to recognize odontogenic cysts.
As already mentioned, pronounced symptoms are characteristic of the late stage of development of a pathological formation, therefore it is difficult to diagnose a cyst at the initial stage, relying only on symptoms.
The final diagnosis is made on the basis of histological examination. It is important to differentiate an odontogenic cyst from other pathologies (adenomatoid odontogenic tumor, ameloblastic fibroodontoma and calcifying epithelial odontogenic tumor).
The CT scan method is widely used in the diagnosis of jaw cysts to confirm the presence of calcifications along the wall of the cyst, as well as tiny spots that are usually not found on x-rays. In addition, computed tomography is necessary during the surgical planning stage.
What is the prognosis for the disease?
How successfully the situation in a patient with an odontogenic cyst will be resolved depends on at what stage the cyst was discovered, how severe the symptoms were and how it was treated.
As a rule, the use of surgical treatment gives a positive prognosis. Therapeutic treatment provides a positive prognosis only if it is started at the initial stage of the disease.
A negative prognosis may be associated with detection of the disease at a late stage: odontogenic cysts can provoke the development of serious pathologies that cause deformation of the maxillofacial tissues.
What treatment methods for jaw cysts exist?
The choice of treatment method for an odontogenic cyst directly depends on the symptoms it causes, as well as the results obtained during instrumental and laboratory diagnostics.
If surgical treatment is chosen (cystotomy or cystectomy), the maxillofacial surgeon performs complete removal of the cyst. In some cases, it is necessary to remove the cyst along with the affected parts of the tooth root. Treatment is carried out in a hospital setting.
If the choice falls on therapeutic treatment, the doctor will carry out procedures aimed at reducing inflammation. This is a long process, taking at least six months.
The first step is to drain the contents of the cyst using a special drainage tube, which is inserted into a small incision in the tumor. As the contents drain out and the tumor shrinks, the size of the tube is adjusted downward.
After removing the contents of the cyst, the dentist cleans the root canals and administers medications that destroy the tumor tissue. At the end of all procedures, the doctor uses a special solution aimed at accelerating healing.
Treatment is monitored radiographically.
Both after surgical and therapeutic treatment, the patient requires preventive measures that will help avoid the re-formation of an odontogenic cyst.
Symptoms of a dental cyst
The danger of dental cysts lies in the fact that the disease is diagnosed, as a rule, in the last stages, when the cyst has already significantly increased in size and the tooth root canals are being damaged.
At the stage of formation and growth of a dental cyst, the process is asymptomatic. Classic toothache, which manifests itself in other diseases of the oral cavity, in the case of a cyst may be mildly expressed or absent altogether. It joins only if the infection enclosed in the shell has caused acute inflammation of the root and gumboil.
The classic picture of a dental cyst is accompanied by a number of symptoms, but not clearly expressed:
- non-localized pain;
- swelling of the gums;
- discomfort when chewing food;
- the formation of a small bump on the gum or palate.
A frequent complication of a cyst is flux (periostitis), its appearance may be accompanied by the release of the contents of the cyst along the fistulous tract.
As the cyst grows, the following symptoms may appear:
- general weakness in the body;
- increased body temperature;
- enlarged lymph nodes.
If the disease was caused by infections of the nasopharynx, the appearance and growth of the cyst may be accompanied by periodic or constant headaches.