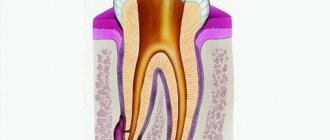
A radicular cyst is a cavity formation at the apex of a tooth root. The inside is lined with epithelial tissue and filled with cystic fluid. The most common cause of a radicular cyst is chronic periapical inflammation. The disease is often asymptomatic and is detected only during a dental examination or x-ray of nearby teeth.
Causes of radicular cysts
The development of a radicular cyst in most cases is caused by an infectious-inflammatory process. The body forms a cystic formation to isolate the source of infection. The inflammatory process begins due to:
- chronic untreated caries;
- pulpitis;
- granulomatous periodontitis (over time, granulomas transform into cysts);
- tooth or jaw injuries;
- previous infectious disease (angina, otitis, sinusitis);
- reduced immunity;
- malocclusion;
- complications during the eruption of wisdom teeth.
Treatment at Dr. Korenchenko’s clinic: a modern and professional approach
See also Treatment of ENT diseases Removal of a cyst in the nose Cyst in the maxillary sinus Treatment of a maxillary sinus cyst
Treatment of maxillary sinus cysts in Dr. Korenchenko’s clinic is carried out in accordance with international standards and using modern techniques. With this disease, thermal and physiotherapy procedures are unacceptable, and the use of any drugs is inappropriate. After examination, if indicated, endoscopic removal of the cyst is performed. The doctor carries out all the necessary manipulations intranasally - through the natural anastomosis of the maxillary sinus and nasal cavity. An endoscope with a camera and micro-instruments are used.
This operation does not lead to disruption of the natural ventilation of the maxillary sinus and gross scar tissue changes. It can be performed even on patients with various concomitant somatic diseases and contraindications for general anesthesia.
Symptoms
The disease has no pronounced symptoms. Minor signs that are sometimes observed are attributed by patients to other pathologies and ignored. When examining the oral cavity, a dentist may suspect a cyst when he discovers a darkened tooth or advanced caries. If you probe the root canals, a yellowish liquid discharge and absence of pain during manipulation will indicate a cyst.
The formations can reach 5 cm in diameter. With significant dimensions of the radicular cyst, displacement of the teeth occurs; upon palpation in the affected area, pliability and a “parchment crunch” are felt.
The cyst develops asymptomatically until it suppurates. It is accompanied by pain localized around one tooth, weakness, and fever.
Sometimes the infection spreads to the inner ear and sinuses, causing an acute inflammatory process. A large cyst can deform the walls of the maxillary sinus, cause atrophy of the spongy bone and sinusitis.
Diagnosis using dental CT
A dental computed tomogram (dental CT) is an informative diagnostic tool for dentists. Using a dental CT scan, you can determine the exact number of roots of a tooth, branches, bifurcation of roots, the presence of impacted teeth, the presence of inflammation at the roots of teeth (periodontitis), the condition of bone tissue, the sufficiency of bone for the installation of dental implants, the location of the jaw nerve and much more. Dial-Dent has its own tomograph, so a CT scan is done right in the clinic, in a few minutes. The doctor can immediately view the CT result and make the correct diagnosis.
Quite often, dental CT results reveal problems that the patient was not even aware of. In this case, a CT scan of the teeth was done before installing the implants. A CT scan of the teeth revealed inflammation at the roots, which over time could lead to loosening of the tooth and its loss. The patient did not even remember that this tooth had ever hurt. At the moment, nothing bothered me, and only the attentiveness of the orthopedic dentist S.V. Tsukora helped to notice the problem in time. At Dial-Dent, before dental prosthetics, they always do a full CT scan in order to see the condition of the entire oral cavity and not miss asymptomatic diseases that can reduce the quality of prosthetics.
A fragment of a dental CT scan, which clearly shows a cyst:
Diagnostics
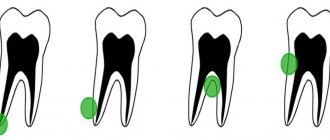
Often a cyst is found when neighboring teeth begin to be treated. A radicular cystic formation is clearly visible on an x-ray - it is a round-shaped shadow with a clear border, adjacent to the apex or wall of the root.
To clarify the diagnosis, electroodontometry is done. To clarify the nature of the neoplasm, a puncture with a thick needle is prescribed. To check the extent and distribution, you will additionally need radiography of the paranasal sinuses, sometimes contrast radiography and computed tomography of the upper jaw bone.
Treatment
Radicular cysts are treated through surgery—cystotomy or cystectomy.
Cystotomy is used in the case of a large cyst that affects the roots of several adjacent teeth and destroys the walls of the maxillary sinus. The operation involves cleaning out the cyst cavity through a small hole made from the mouth, nose or paranasal sinus. Upon completion, the surgeon disinfects the cavity and inserts a swab with iodoform there. A week later, the tampon is replaced with a new one, and this continues until the doctor is convinced that the inflammatory process has stopped.
Cystectomy is the removal of a cyst by separating the fibrous membrane of the formation from the surrounding tissue. The operation ends with tamponade of the cavity or bringing together the edges of the mucous membrane that have been damaged. Cystectomy is done for small cysts.
Postoperative recovery will be successful if the patient takes oral hygiene instructions seriously: use antiseptic rinses and brush teeth carefully. In case of increased body temperature, as well as intense and prolonged pain, you should immediately consult a doctor.
Tooth cyst (radicular cyst) - symptoms and treatment
Types of treatment for radicular cysts can be divided into conservative, surgical and conservative-surgical.
Conservative treatment
The conservative method is aimed at removing the necrotic neurovascular bundle of the tooth (pulp) and eliminating pathological changes in the bone behind the root apex.
The decayed pulp is removed with special endodontic instruments. Then the root canal is expanded and antiseptic treatment is carried out. Medicinal pastes are introduced into the root canal, which eliminate the microbial flora and restore the affected bone tissue. These pastes are administered for a period from several days to 1–1.5 months. Usually this process is well tolerated, but sometimes the pastes cause an exacerbation of the process with severe pain. To prevent the paste from getting into the mouth, the tooth cavity is hermetically sealed with a temporary filling.
If the inflammation of the bone tissue is eliminated, the root canals are filled with permanent material, and the defect in the hard tissues of the tooth is closed with a filling.
The fact is that there are no microorganisms in the cyst cavity itself. This is a response to a high concentration of microorganisms in infected root canals. After proper treatment of the canals, the number of microbes decreases and the body, with the help of cellular immunity, copes with a small number of microorganisms in the area of the root apex. The “barrier” in the form of a thin connective tissue membrane of the cyst becomes unnecessary, and macrophages completely destroy the membrane. With a small size of the cyst, rational treatment and the body’s ability to resist the disease, conservative treatment gives a good result - the shell of the radicular cyst is completely resorbed, the alveolar fascicle bone is restored.
After final treatment of the canals, it is recommended to do a CT scan after 6 and 12 months. If the cyst is completely resolved, there is no need to fear relapses, since the cause (bacterial infection of the canals) has been completely eliminated.
After root canal treatment, the tooth does not receive adequate nutrition, so it may deteriorate over time. To prevent this, it is recommended to cover pulpless teeth with artificial crowns.
If the conservative method is ineffective and the focus of destruction remains, surgical removal of the cyst is performed. This combination of methods is called conservative-surgical treatment.
Surgery
The surgical method involves removing a cyst from a previously pulpless tooth, and often the apex of the tooth root is cut off. The operation is carried out strictly according to indications: in case of a broken instrument, poor-quality treatment of the measles canal, or if the root protrudes into the cavity of the cyst. The extent of surgical intervention is determined during diagnosis.
To improve the prognosis after surgical treatment, bone defects are more often replaced with osteoplastic materials [15][16]. Such materials restore lost bone tissue and stimulate the formation of new one.
One of the main directions in modern reconstructive surgery is the use of biotechnologies, which allow accelerating the processes of regeneration of damaged tissues [17]. We are talking about platelet-derived growth factors obtained from the patient’s own blood. First, venous blood is taken from the patient. Then, using a centrifuge, the blood is separated into fractions. The platelet-rich fraction is used to restore bone tissue defects. This method is available almost everywhere.
There are two main surgical methods for treating radicular cysts: cystectomy and cystotomy.
1. Cystectomy is an operation in which the fibrous membrane of the cyst is completely removed. Usually performed in an outpatient setting under local anesthesia. If the cyst is large and affects the nasal cavity, maxillary sinus or mandibular canal, the operation is performed in a maxillofacial surgery hospital.
Surgical technique:
- Under local or general anesthesia, a section of the jaw bone in the projection of the cyst is skeletonized (exposed).
- Access to the cyst cavity is created, all affected bone tissue and the cyst shell are removed.
- According to indications, the root apex or part of it is cut off and retrograde filling of the root canal is performed (filling through the root apex) and filling of the apical openings of the canals with special cement intended for these purposes.
- The surgical wound is treated with antiseptic solutions, filled with osteoplastic material and sutured.
- Postoperative material is sent for pathohistological examination.
A dental microscope is used for treatment. It allows you to minimize the volume of removal of the root apex and effectively close the root canals.
You must visit the doctor the next day after the operation, then if the course is calm after 10–14 days, to remove the stitches. The patient should be under the supervision of the attending physician until the postoperative wound is completely healed, then return every six months to monitor the restoration of bone tissue and exclude relapse. As practice shows, relapses are rare; they are usually detected in the first year after surgery.
Types of material for filling a bone tissue defect after surgery:
- Autogenous material is obtained from another area of the patient’s bone tissue (branch of the jaw, chin, etc.). Due to its complete biological compatibility, such material is rarely rejected and quickly restores the defect. However, when the patient’s tissue is taken, the operation time increases, the intervention becomes more traumatic, which negatively affects the patient’s recovery.
- Xenogeneic material is obtained after special processing of mammalian bone tissue. The most commonly used bones are ox and pork. Processing removes substances that can cause immune and allergic reactions.
- The synthetic material contains calcium salts. For better compatibility it is often used in combination with autogenous material.
2. Cystotomy is an operation during which the cyst shell is not removed, but only its anterior wall is excised, which allows the contents of the cyst to be evacuated. With cystotomy, the scope of surgical intervention is smaller, but recovery after such an operation lasts longer (about a month). The resulting bone defect is filled with turunda with iodoform, then dressings are made with a certain frequency, replacing the turunda. This method is used less and less due to protracted recovery, the introduction of new techniques and the improvement of the material and technical base.
Oronasal (between the mouth and nose) cystectomy and oronasal cystotomy are performed if the cyst penetrates into the maxillary sinus or pushes it aside.
Surgical methods using laser technology are increasingly used in modern dentistry. Laser techniques are less traumatic. In addition, the laser has a bactericidal property, which reduces the likelihood of developing purulent-inflammatory complications [18][19][20].
Removal of a tooth. A tooth is removed only if saving it is not practical. Indications for removal:
- complete destruction of the crown part of the tooth;
- destruction of the hard tissues of the tooth below the level of the gingival margin by more than 2 mm, when it is not possible to advance the root orthodontically or when the root of the tooth is too short, which will complicate further prosthetics;
- lack of lumen in the root canal (due to structural features or previous treatment).
In all other cases, tooth-preserving operations described above are performed.
Complications after treatment
Complications after cyst removal occur infrequently. These include perforation of the maxillary sinus, damage to the inferior alveolar nerve, as well as the formation of a residual cyst, which is formed during incomplete excision of the radicular cyst.