Causes of the disease
Other diseases and bad habits can lead to the development of this disease, such as:
- viral and bacterial infections;
- nicotine abuse;
- weakened immune system;
- sinusitis and tonsillitis;
- ARVI;
- dental diseases.
Risk factors are:
- hypothermia;
- increased mental and physical stress;
- frequent stress.
The influence of factors often leads to accelerated tumor growth. Teeth that were previously filled or reconstructed are most susceptible to this disease.
The main causes of pain in the gums
As soon as the anesthesia wears off, the patient begins to feel pain. Gum pain after tooth extraction for 10 days is normal. It is during this period that the wound heals completely.
Pathological pain longer than this period indicates the presence of a progressive infection. There are many reasons for inflammation. However, they all have a common beginning - removal of a formed blood clot. Food enters a fresh, unhealed wound, thereby accelerating the formation of harmful bacteria.
The main causes of cheek pain can be:
- Inflammation of the trigeminal nerve. Unfortunately, the patient may also experience hearing loss. Such a complication cannot be allowed to occur; it is worth seeking professional help.
- The remainder of the tooth in the wound will certainly provoke the accumulation of pus. This often happens when working with “complex” teeth that have crooked roots.
- The clot can be easily washed out of the dry socket. In such cases, bacteria easily penetrate the open wound, causing inflammation.
- Patients suffering from diabetes are susceptible to the formation of hematomas in soft tissues. Over time, the accumulated blood suppurates.
- The pathological process can be triggered by a cyst, which usually grows on the root of the tooth, and may remain even after surgery.
- Alveolitis is inflammation of the gums. This problem occurs when an infection gets into an open wound.
- After tooth extraction, patients often experience bleeding. This is considered the norm. However, prolonged bleeding is a reason to consult a dentist.
- Osteomyelitis is considered to be one of the most dangerous complications. The fact is that destruction occurs not only of the soft gum tissue, but also of the jaw bone. Weak immunity or neglected dental problems are the main causes of osteomyelitis. The worst thing is that the complication can infect the brain.
Symptoms
Many patients wonder what a dental cyst is and how to treat it. To find the answer, you need to understand the symptoms. As already noted, signs of the presence of a formation can be noticed only at a late stage. The symptoms of a dental cyst are as follows:
- pain in the jaw area that does not have a specific location;
- discomfort when chewing food;
- inflamed gums.
A tubercle is formed in the area of the tooth root, which subsequently increases in volume. The consequence of this process can be flux.
A cyst under a tooth can cause the following conditions:
- physical weakness;
- increased size of lymph nodes;
- increase in body temperature.
A serious danger is that the severity of pain with this disease is much lower than with other dental diseases. An extracted tooth with a cyst cannot be restored, so you must immediately consult a doctor if any discomfort occurs.
They removed a tooth cyst, but it still hurts: what to do?
A dental cyst is a cavity filled with pus that forms at the apex of the tooth root. In itself, this is a very painful disease, which is also fraught with the spread of infection and various complications. Therefore, if you notice swelling at the root of the tooth and experience pain when biting, be sure to contact a specialist who will remove the cyst.
How to remove a tooth cyst
There are several ways to remove a tumor. Including laser, therapeutic and surgical interventions. Therapeutic treatment includes antiseptic treatment of the tooth, cleaning and sealing. The essence of laser treatment is clear - the cyst is removed due to the action of laser radiation. Surgery is usually performed in particularly advanced or complicated cases.
A tooth cyst was removed, it still hurts: what to do?
Let's say you removed a tooth cyst, but it still hurts. What to do? Don’t worry, experts admit the possibility of pain after surgery, which is associated with the recovery process. If a tooth cyst has been removed and it hurts and the gums are swollen, first try rinsing with an antiseptic solution as prescribed by a specialist, or take anti-inflammatory and painkillers. However, don't get carried away, remember that such medications put a lot of stress on your liver and can do more harm than good.
Normally, pain after removal of a dental cyst can last for about 1-3 days, but a positive trend in its subsidence should be felt. If it hurts and swells as before or even more strongly, this is one of the indicators that the treatment was not carried out properly, or you violated a number of conditions for proper recovery after removal of a dental cyst. In any of these cases, you need to see a doctor again - he will examine the diseased tooth and make the necessary appointments.
How to recover after tooth cyst removal
If you want to recover quickly after surgery, follow all your doctor's instructions. For the first few days, refrain from smoking and drinking alcohol, and do not eat too hot or too cold food (the same applies to drinks). Do not apply warm compresses or take antibiotics unless prescribed by a doctor! Avoid chewing pressure on a sore tooth, rinse your mouth after every meal, and when brushing your teeth, carefully walk around the sore spot so as not to injure it.
You can get a consultation at the DENTISTRY clinic. Make an appointment by calling +7 (8342) 308–088 or using the form below.
Make an appointment
Tooth hurts after extraction
Fact #1
Aching pain after tooth extraction is a normal reaction of the body to surgery.
Why does pain occur?
After tooth extraction, pain is inevitable, because removal is a surgical operation. Depending on the complexity of the manipulation, the patient begins to feel aching or throbbing pain almost immediately as soon as the anesthesia wears off.
Tooth extraction (tooth removal) is a relatively simple operation, if it is not an impacted, dystopic eighth tooth (wisdom tooth). Surgery is accompanied by damage to soft tissues, which require time to recover. Soreness, swelling, redness are natural reactions of tissues to injury.
Pain is a normal reaction of the body to injury to the mucous membrane during and after the procedure. If the pain does not go away within a few days, but only intensifies, you should immediately consult a doctor.
Recommendations after tooth extraction
After tooth extraction, the dentist and surgeon will definitely give you recommendations and explain which sensations are considered within normal limits, and in which cases it is necessary to urgently come for an examination.
Standard recommendations include:
- It is recommended to keep ice in the cheek area on the side of the extracted tooth (the doctor's assistant will offer you ice immediately after the operation). This will minimize swelling and speed up regeneration.
- You should not touch the socket of an extracted tooth with your tongue, much less with your finger or other objects.
- Do not try to remove something from the hole that seems unnecessary to you. In our clinic, a self-absorbing collagen sponge is placed into the hole; it helps to form a full-fledged clot in the wound. The clot protects the wound from infection; it works like biological glue.
- If the surgeon has placed stitches, do not touch the threads with your tongue or try to remove them. During your post-op check-up, you will be given a date to remove your sutures in a sterile dental office (usually day 7). If the sutures are self-absorbing, they will disappear within 10 days.
- It is recommended not to eat for 2 hours after surgery - this is the minimum. This is necessary so as not to cause bleeding or infect the wound.
- Food and drink should not be hot. For the first time, they exclude foods that are too sour, salty, and spicy.
- Alcohol-containing drinks are excluded because they dilate blood vessels and can cause bleeding.
- It is necessary to refrain from smoking for at least 3 hours after surgery, since nicotine reduces the protective response of the soft tissues of the oral cavity.
- You should not overheat - visit the bathhouse, sauna, take a hot bath and hot shower.
- Physical activity and sports are excluded.
- You cannot rinse your mouth with active movements; baths are recommended - just keep the rinse in your mouth.
- You should not blow your nose too much, as this can cause bleeding and disrupt the healing process in the socket.
Oral hygiene after removal
is allowed only the next day after surgery. You must use a soft toothbrush. You need to brush your teeth bypassing the wound at the site of the extracted tooth. If the doctor has prescribed baths, you must follow the recommendations. Good oral hygiene after surgery is very important and promotes a speedy recovery.
How long does pain last after tooth extraction?
How many days pain can persist after tooth extraction is purely individual. The norm is considered to be up to three days, and starting from the third day, with normal healing and the absence of complications, the pain begins to subside. The healing process depends on the general condition of the body and on what the situation was in the oral cavity at the time of removal - if against the background of inflammation, then the infection can provoke swelling of the gums and a longer and more painful recovery.
Swelling after tooth extraction
Normally, tooth extraction may be accompanied by swelling of the cheek in the following cases:
- If there was already swelling before surgery.
- If tooth extraction was carried out against the background of an inflammatory process.
- If the tooth extraction was difficult - when the operation requires cutting the gums.
- Do not panic if swelling of the cheek after a complex removal leads to asymmetry, difficulty swallowing and discomfort when opening the mouth - these temporary phenomena will pass as healing occurs.
Fact #2
Swelling in the area of the removed extreme molar occurs in 90% of cases.
In what cases should you urgently consult a doctor?
If the nature of the pain after removal goes beyond what the attending dentist warned you about, you should consult a doctor.
Symptoms that should alert you include the following:
- More than 3 days have passed since the tooth was removed, and the pain does not subside.
- There is bleeding that lasts for 24 hours.
- Body temperature increased above 38.
- The swelling of the cheek does not decrease, but rather increases.
- On the 3rd and 4th days, difficulties in opening the mouth persisted.
Our doctors
Is a tooth cyst a death sentence or not?
A dental cyst is a pathological neoplasm inside the bone tissue of the jaws as a result of the body’s defensive reaction to infection or injury. A dental cyst, as a rule, has an epithelial membrane and is filled with cystic exudate. The cyst in most cases has a chronic course and continuous growth.
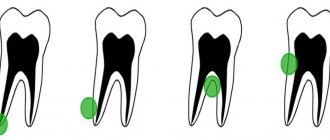
A dental cyst has several stages of development: granuloma (small, less than 5 mm in diameter); cystogranuloma (up to 1 cm in diameter); cyst (more than 1 cm in diameter)
Reasons for the formation of cysts in the maxillofacial area:
- endodontic treatment of root canals . The tooth canal has more than one nerve trunk; it has many lateral branches. When treating the root canal of a tooth, infected tissue remains in these lateral micro-branches and after abturation of the canal a chronic inflammatory process can begin. Initially, a small granuloma (destruction of bone tissue) is formed, which eventually develops into a cyst. The simpler the anatomy of the root canal and the more accurately the treatment protocol for complicated caries is carried out, the lower the risk of developing cysts. In multi-rooted teeth with complex anatomy of the root system (bent, curvature, scarring, difficult access), the likelihood of developing root cysts increases significantly.
- Acute dental trauma. If a tooth has suffered trauma (impact), you should consult a doctor. Death of a nerve in a tooth or rupture of the neurovascular bundle may be invisible at first after injury and not cause concern to the patient. But such a tooth needs to be observed for several years, control x-rays taken, in which the doctor will be able to notice changes in the bone tissue in time and thereby prevent the formation of a root cyst on the root of the tooth.
- Chronic injury. There are two main reasons for this. One of them is long-term overload of the tooth as a result of missing neighboring teeth or a large number of lost teeth. This also includes occlusal supracontacts as a result of improper prosthetics or tooth treatment. The second is a vital (living) tooth covered with a crown. According to statistics, in 10% of such cases there are complications - nerve death. And if this is asymptomatic, then over time a cyst will form on the root of the tooth.
- Complications of other diseases. A root cyst of a tooth as a result of chronic sinusitis or a lateral cyst of a tooth as a result of chronic periodontitis. It is extremely rare that we encounter the formation of a cyst as a result of the transfer of infection by the bloodstream in any general somatic disease.
- Retention cyst . Cyst of an unerupted tooth. This is usually a wisdom tooth cyst. But cysts of other impacted teeth also occur.
- Residual cyst. The remaining cyst after tooth extraction. It can also increase in size and can lead to an inflammatory process. And most importantly, in the presence of such a cyst, it is not possible to carry out two-stage dental implantation.
Clinical symptoms of a dental cyst
- Asymptomatic. The course can last for years. The patient does not notice anything at all and nothing bothers him. The cyst is discovered by chance during an X-ray examination
- Chronic course. The patient can palpate (with his finger) the formation of some kind of tubercle in the area of the apex of the tooth root; discomfort when pressing; slight redness or minor pain symptoms that periodically make themselves felt. When visiting a doctor and R-graphic examination, the presence of a cyst in this area is determined.
- Acute course. With an exacerbation of the chronic process, the cyst suppurates and pain, swelling, redness, temperature, and general malaise appear. Pain appears when pressing on the causative tooth, which intensifies with chewing. A fistulous tract may form in the area of the root apex. Regional lymph nodes are involved in the process.
Consequences of an untreated dental cyst
The consequences of a cyst include, first of all, the likelihood of its exacerbation and the development of periostitis, purulent abscess or osteomyelitis. Inflammation of the cyst is quite pronounced and often ends with tooth extraction and can lead to short-term disability. If the patient at this stage does not consult a doctor and does not receive qualified dental care, sepsis may develop. This is an extremely serious condition, characterized by infection entering the blood and spreading throughout the body.
As a result of an asymptomatic course, the cyst gradually increases in size, destruction (destruction) of the bone tissue around the tooth occurs. The cyst can reach several centimeters in diameter and in this case the likelihood of complications is very high.
Here, for example, are some complications of an overgrown cyst:
- destruction of the bottom of the maxillary sinus, germination into it and, as a result, sinusitis.
- destruction of the cortical plate of the alveolar process and, as a consequence, the formation of a fistulous tract and the impossibility of installing an implant subsequently.
- growth of the cyst into the canal of the mandibular nerve, leading to neuritis.
- the growth of a cyst on the lower jaw can lead to a pathological fracture of the jaw.
- the growth of the cyst leads to the involvement of the roots of neighboring teeth in the pathological process and, as a result, their removal (removal of completely healthy teeth!)
Treatment methods for dental cysts
1. Conservative treatment
This type of treatment allows you to save the tooth. The dentist creates access to the root canal of the tooth, opens it and cleans it. Since the apex of the tooth is connected to the root cyst, the contents of the cyst emerge from the canal. After antiseptic and mechanical treatment of the root canal, it is filled with special calcium-containing pastes. Treatment lasts from 1 to 6 months, depending on objective data and the patient’s ability to visit a doctor.
Only after 6 months, on a repeated R-graph of the tooth, one can see the regeneration of bone tissue, the formation of bone balls in the area of the cyst and say with confidence about the success of the conservative method.
In our Euro Dentistry clinic, dental therapists have extensive experience in treating dental cysts using a conservative method, have a large percentage of cases of successful bone tissue regeneration, and fight for each tooth together with the patient. Only in the most critical cases do they abandon this method and send the tooth for extraction.
2.Surgery.
Here, too, not everything is clear. There are several methods of surgical treatment of root cysts. These are:
— Cystectomy operation with resection of the root apex. This is the removal of the cyst and part of the damaged root. The method is highly effective, but is quite complex and requires highly qualified specialists.
- Hemisection. In this case, one root is removed from a multi-rooted tooth. The doctor removes the cyst, the damaged root and part of the tooth crown, and the tooth is covered with a crown. The method is less effective, complex and unpredictable.
- Removal of a tooth. It is carried out with the obligatory removal of the cyst capsule to avoid relapse.
At Euro Dentistry in Vitebsk, after examining the patient, clinic specialists will make a final diagnosis and offer the best treatment option for the dental cyst. A cystectomy or tooth extraction along with a cyst will be performed without pain.
Hematoma
In addition to alveolitis, another complication such as hematoma and suppuration of the hematoma occurs. At the same time, we see normal healing of the socket, but there is pronounced swelling and pain in the soft tissues (cheeks, along the transitional fold).
The main signs of a hematoma are:
- swelling of the cheek in the area of the extracted tooth or at the site of anesthesia;
- pain when touching the cheek;
- the cheek is warmer than the surrounding tissues;
- cyanosis appears on days 3-4;
- the temperature may rise.
There can be many reasons for the formation of hematomas, but the main ones are:
- vascular injury during anesthesia or removal of tooth fragments. All people have different vessels, and the surgeon cannot say with certainty where the vessel will go;
- problems with blood clotting (diabetes, leukemia).
Hematomas also cannot be treated at home. You definitely need to see a surgeon.
If the hematoma is relatively small and there are no signs of suppuration, then drugs are prescribed to resolve the blood. If the hematoma is large and there are signs of suppuration (fever, sharp pain, redness of the cheek and increased skin temperature, tissue tension), then an incision is made along the transitional fold, pus and excess blood are released, and drainage is placed in the wound. After a week, the wound heals, leaving a scar.
Home treatment of hematomas is fraught with the formation of abscesses and phlegmons, which may require external incisions and subsequent cosmetic surgeries, and in advanced cases can cause serious complications for the body as a whole.
Tooth root cyst: what is it and why is it dangerous?
The author of the article is dentist-surgeon-implantologist A. A. Kipel.
A cyst is a signal that the process of destruction of living tissue in the oral cavity is in full swing. If the patient ignored preventive examinations and consulted a doctor only when pain appeared, the tumor had already reached serious proportions. It will have to be removed surgically. Visit Stoma specialists have performed hundreds of such operations and were able to save even the most “hopeless” teeth.
In the early stages, the danger can be neutralized without the intervention of surgeons - using conservative treatment methods. But for this, you need to know what a cyst is, how it arises and develops.
Cyst development
If an infection gets into the bone tissue of a tooth, it begins to break down. The injured cells die and a cavity appears in their place. The body does its best to resist inflammation and builds up a protective film around it - a barrier that prevents the further spread of infection. The cavity at the top of the tooth root, surrounded by a dense membrane, is a cyst. Inside it is filled with exudate - bacteria, secretions from blood vessels with a high content of leukocytes and dead bone cells. Unfortunately, even under the membrane the cyst continues to grow. The inflammation seems to be eating away at the bone from the inside, and if no action is taken, it simply won’t remain under the tooth.
The bone cavity can be of any size. The longer the infection remains in the bone, the larger the cyst grows. The neoplasm develops in 3 stages. The division is conditional. The stages of cyst development are determined by its size and monitored on an x-ray, but only a histologist can reliably determine them.
The first stage is granuloma. It grows on the root of the tooth quite quickly and does not exceed 5 mm in diameter. The next one is cystogranuloma. This formation is not cavitary, without exudate, but is already surrounded by a membrane characteristic of a cyst. The coverage does not exceed 8 mm. The final stage of the development of the disease is a cyst, which is a cavity larger than 9 mm. The last 2 phases are irreversible without surgical treatment.
Reason for appearance
Cysts on the top of the tooth are the result of inflammation that has become chronic. There are known cases of their degeneration into malignant tumors.
Even a small inflammatory process in the oral cavity can lead to bone damage and the formation of a depression in it.
How does a tooth root cyst develop?
Affects the formation of cysts and the general condition of the body. Most often, cysts form in women over 45 years of age.
The main reason for the appearance of granulomas and cysts is poor-quality or untimely treatment of caries. And you can avoid it only by consulting a doctor in time.
Duration of pain after tooth extraction
Every patient is concerned about the question: how many days does the gum hurt after tooth extraction? A period of 2 to 4 days is considered normal. Provided that the pain is not acute, but moderate. After the removal of a molar, the gums hurt for several days longer.
Attention! Your gums cannot hurt for more than one week, much less for a whole month. During this time, the hole should heal completely. If a person is constantly accompanied by this symptom, he urgently needs to consult a doctor. It is important to relieve inflammation in the initial stages; in advanced cases, treatment will be longer and more complex.
Normal and signs of complications
Since tooth extraction is a full-fledged surgical operation, pain is inevitable. During the removal process, nerve endings and blood vessels are injured, bone is injured, so pain in the gums is inevitable.
The following course of the postoperative period is considered normal:
- aching pain (no pulsation, shooting);
- every day the pain becomes less;
- In the first three days, swelling in the area of removal may increase, and from the third day onwards it subsides. After the removal of the lower wisdom teeth, it may be difficult to open the mouth due to swelling or facial asymmetry - this is also normal;
- body temperature is normal or elevated on the first day after removal;
- there is a blood clot in the socket on the first day, on the second day there is a white or grayish film, which is replaced over time by new mucous membrane;
- The gums at the site of removal are red on the first day, and then, every day, they become less swollen and acquire a normal pale pink color.
The strength and severity of all these symptoms depends on the complexity of removal. If a tooth was removed due to periodontal disease, and this tooth was already mobile and its root was 1/3 in the bone, then after removal, the patient may not experience any discomfort on the first day. If the tooth was deep in the bone, and to remove it it was necessary to make an incision, saw out or bite off part of the bone, saw the tooth into pieces and take it out piece by piece, and then apply sutures, then the pain will be normal even within a week.
What symptoms indicate that the healing of the hole is not going properly and there are complications?
- The pain does not decrease every day, but remains at the same level or intensifies;
- the nature of the pain is pulsating;
- in the area of the extracted tooth, the gums are red and painful to touch;
- swelling of the mucous membrane increases (as well as along the transitional fold or in the cheek area);
- the appearance of bad breath;
- elevated temperature.
If inflammation in the socket progresses after removal, this situation is called alveolitis. Such inflammation can occur both due to the fault of the doctor and the fault of the patient.
The dentist may accidentally leave part of the root of the tooth being removed or a movable fragment of bone in the socket, may leave part of the cyst capsule, and may also not control the process of formation of a blood clot. There are cases when, after removal, the gum does not bleed and the socket is dry - the doctor must ensure that the socket is filled with blood, and if there is none, with special preparations to protect the bone.
Through the fault of the patient, alveolitis most often begins due to non-compliance with recommendations:
- active rinsing (as a result of which the clot is washed out and unprotected bone remains);
- eating hot food and drinking on the first day or lifting weights (also leads to increased pressure and removal of the clot from the socket);
- non-compliance with prescriptions (refusal of rinses, antibiotics or other prescribed therapy).
In addition, there are situations where complications after removal are associated with general health. With reduced immunity (due to taking corticosteroids, diabetes, leukemia and other diseases), blood clotting and resistance to infections are impaired - all this can cause alveolitis. If you have complex systemic diseases, you need to warn your doctor about them.