Pulpitis is one of the most common dental diseases, which in most cases can be effectively treated.
The main condition for the effectiveness of the measures taken is a timely visit to a dentist-therapist. If you feel painful symptoms, you should not postpone your visit to a specialist - the sooner you go to the clinic, the greater the chance of saving the tooth. Pulpitis is characterized by an inflammatory process in the inner part of the tooth, called the “nerve.” This determines the severity of the symptoms - the pain with pulpitis is very noticeable. In most cases, the disease develops as a result of caries if the patient does not consult a doctor in time. In rare cases, pulpitis is associated with improper treatment of caries, violations of the tooth preparation process or other manipulations, and it can also be the result of injury.
Types and symptoms of pulpitis
Symptoms, as well as treatment tactics for pulpitis, depend on the type of disease. The following classification of the disease is currently used:
- Spicy. Often this type of pulpitis is the result of untreated caries. If the patient does not pay attention to tooth decay, after some time the infectious process reaches the internal structure - first dentin, and then pulp, provoking its inflammation. Symptoms of this form of the disease include acute throbbing pain, which intensifies significantly when exposed to chewing, contact of the tooth with food or high-temperature drinks. The pain often gets worse at night. Acute pulpitis, in turn, is divided into two types:
- focal - in this case the pain is “point-like” in nature, observed in one area of the tooth;
- diffuse - pain sensations spread to one or another area of the jaw as a whole.
- Chronic. It results from ignoring the symptoms of an acute form of the disease. As a rule, about 2 weeks pass from the onset of inflammation until the disease becomes chronic. Painful sensations become less pronounced, severe discomfort disappears. However, the pain continues to persist and intensifies when exposed to the causative tooth. The tooth is destroyed, and the acute pain returns from time to time.
When should you visit a dentist?
The sensitivity of the neurovascular bundle of a tooth in a child is lower than in an adult, so the symptoms of its inflammation may be erased or absent altogether. It is important to contact a pediatric dentist when the first symptoms of caries appear - a dark spot on the tooth, or the child complains of pain. You should hurry up with your visit if:
- severe pain;
- increased pain when eating hot or cold food/drinks;
- bad breath;
- elevated body temperature;
- inflammation of the gums around the tooth;
- darkening of the enamel.
What happens if pulpitis is not treated?
It can be difficult for a modern person to find time to visit a dentist in his busy schedule. The most common mistake is to try to ignore painful symptoms by “masking” them with a large number of painkillers. You should know that even if the pain was calmed, treatment of pulpitis still cannot be avoided - pathogenic organisms in the pulp chamber continue to multiply, destroying the tooth and surrounding tissues. Changes occur inside the tooth that lead to the death of the pulp, its decomposition with the formation of pus.
Subsequently, the pus extends beyond the root and a flux, known to many, occurs - inflammation of the periosteum. This is accompanied by severe symptoms - high body temperature, severe swelling and facial asymmetry, and also entails not only unpleasant, but also life-threatening consequences. In advanced cases, we are no longer talking about preserving the tooth, but about preserving health - there is a possibility of developing phlegmon, damage to the bone tissue of the jaw, and blood poisoning.
Chronic pulpitis can occur with the preservation of the tooth for up to several years, especially at a young age, but this does not mean that the symptoms can be ignored - it is better to visit a dentist in a timely manner in order to save the tooth and prevent serious complications.
Prevention of pulpitis in children
Treatment of pulpitis in permanent teeth in children, as well as their “predecessors” - baby teeth - is a rather complex procedure that may require several visits to the doctor. Preventing a disease is easier than treating it - all you need to do is pay attention to hygiene procedures and teach your child how to brush their teeth correctly from a very early age.
It is also important to monitor the child’s diet - strengthen the enamel with solid foods (carrots, apples, etc.), provide a balanced diet to saturate bone tissue with minerals. It is better to limit sweets and give only water at night. Prevention of caries is the basis for preventing its complications, including pulpitis.
Diagnosis of pulpitis
The diagnosis is made by a doctor based on a survey and examination of the oral cavity. As a rule, pulpitis precedes developing caries, so there is a carious cavity in the causative tooth. The doctor performs probing - places an instrument into the cavity to assess its depth and reaction. Tapping is a method that also helps the doctor find out how the tooth reacts to mechanical stress. The main task of the specialist is to determine the difference between pulpitis and deep caries - treatment tactics depend on this.
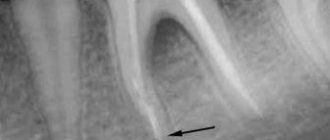
An X-ray examination is necessary in order to assess the nature of the disease, as well as determine the structure of the root system - the doctor will need this information for further endodontic treatment of tooth pulpitis (treatment and filling of canals).
Treatment of pulpitis
To avoid complications of pulpitis, it is important to start treatment in a timely manner. In rare cases, this allows you to save the pulp and avoid its extraction from the canal, but partial or complete removal of the neurovascular bundle is still more often practiced, and here’s why.
Removing the pulp allows you to completely eliminate the source of inflammation, which means preventing the spread of pathogenic microorganisms into the tissue surrounding the tooth. This is the basic principle of preserving the tooth and tissues from possible complications.
Treatment methods for pulpitis are divided into two broad categories:
- treatment that involves preserving living pulp;
- treatment of pulpitis of permanent teeth with pulp removal - complete or partial.
The decision to choose a method falls on the shoulders of the doctor - he assesses the condition of the pulp. The biological method (implying preservation) is used only when inflammation is observed at a very early stage, and it is also more often applicable to young patients who do not have other oral diseases.
Extirpation, or complete removal of the pulp, is the most common practice and is an effective and reliable method. It can be vital and devital - the difference is that in the first case the doctor removes the pulp under local anesthesia, and in the second, he first kills it using special means. Devital extirpation can be carried out without anesthesia, since the neurovascular bundle will no longer react to irritation, which means there will be no painful sensations. However, in practice, even in this case, an anesthetic is often given to avoid discomfort.
Preliminary devitalization consists of the fact that during the first visit, the doctor removes the destroyed tooth tissue, treats the cavity, and puts a special paste into the canals. Previously, in domestic dentistry, the method of devital amputation was used, which consisted of removing the neurovascular bundle inside the crown, while preserving the root pulp. For it, strong solutions were simply used to dry it out, but the voids in the root canals with pulp residues acted as fertile ground for the further development of the inflammatory disease. That is why today most often the pulp is completely removed - this is a reliable and effective treatment method.
A combination therapy method is the use of two or more methods. For example, removal of the entire root pulp from normal canals and partial removal (amputation) from those that have complex anatomy and are strongly curved. The prognosis in this case is more favorable than in the case of devital amputation, however, this is only true if certain conditions are met: most of the canals must be reliably sealed along the entire length, and high-quality materials must be used for this.
Modern dentistry offers a lot of opportunities for improving the method of treating pulpitis through vital extirpation. Pulp removal is carried out without first killing it, and for this purpose a rich arsenal of tools, equipment and means is used. They are designed to facilitate the process of pulp removal and canal treatment, as well as to prevent possible errors and ensure the convenience of the specialist’s work.
Modern anesthetics and devices for their controlled administration make it possible to avoid the need for devitalization - they provide effective anesthesia even for complex lower molars.
When pulp removal is inevitable
The list of indications that determine the need for pulp removal includes the following clinical situations:
- Development of acute inflammatory processes affecting the pulp chamber;
- Acute form of pulpitis that occurs against the background of infection of the cavity;
- The need to open the chamber due to mechanical damage;
- Failure to comply with the dental intervention protocol, causing complications;
- Preparation for prosthetics, which requires eliminating the risk of infection of supporting units.
The decision on devitalization is made based on the results of a comprehensive diagnosis.
Stages of pulpitis treatment
- The doctor performs anesthesia and drills out tooth tissue softened by caries, providing access to the internal structures.
- Removing the pulp - first, the doctor amputates the pulp using a bur or excavator, then performs extirpation - removes the neurovascular bundle from the root canals using thin instruments.
- Channel processing. Using small “needles” - files, reamers - the specialist passes the canals along their entire length, expanding and at the same time treating their walls with antiseptics. In this case, everything “unnecessary” is consistently washed out of the canals: bacteria, canal particles, pus, blood impurities, pulp residues, etc. Drug treatment ensures sterility - the likelihood of complications in the future depends on how carefully it is carried out. After treatment, the doctor dries the canals, places cotton pads impregnated with antiseptics there and installs a temporary filling.
- Filling. During the second visit, the dentist removes the temporary filling and medications from the canals. The treated root canals are filled to the apex - a natural narrowing or the narrowest point. For this purpose, pastes and gutta-percha pins are used that are mixed with the patient.
- Control. X-ray diagnostics are performed to assess whether the canals are filled correctly and along their entire length. Then the doctor places a filling or inlay on the crown of the tooth.
Control makes it possible to prevent some serious errors in endodontic treatment. Removal of the filling material beyond the root apex or insufficient filling are causes of possible complications in the form of the spread of the inflammatory process to the peri-root tissue, so it is important to monitor compliance with the treatment technology.
Pulp removal with preliminary devitalization is carried out according to the same principle, but in this case an additional stage is added and two visits to the doctor are required. On the first visit, the doctor applies a special paste - arsenic or arsenic-free - to the exposed pulp horn. In the first case, you need to come for an appointment within 24 hours, and if devitalization of the pulp of a multi-rooted tooth is carried out, after 48 hours. This type of therapy is more difficult to control by the doctor, because the patient may come for an appointment later than scheduled, which increases the risk of toxic effects of arsenic on the tooth root. That is why modern dentistry suggests using alternative solutions - using a paste without arsenic in the composition.
Methods and tools
Modern methods used for pulp removal include the following options:
- Application of depulp paste based on arsenic or formaldehyde;
- Electrochemical treatment leading to necrosis (coagulation) of the structure.
Due to the toxic properties of arsenic, determining the exact dosage and maintaining the duration of use are key factors. It should be noted that such compositions provide the shortest period of pulp killing.
Use of chemicals
The medical intervention protocol involves opening the upper part of the pulp chamber and applying an arsenic paste, which is delivered using a dental probe. The formed layer is carefully covered with a cotton swab soaked in an anesthetic. To close the cavity, a temporary water-dentin dressing is used, thanks to which the area is hermetically fenced off from external influences.
The duration of the composition inside the crown depends on the number of tooth roots, and varies in the range of 24-36 hours. If chemical periodontitis is diagnosed, pulp extraction is carried out immediately.
In the first hours after the intervention, a painful reaction occurs, for the relief of which it is recommended to use bromine-containing drugs or amidopyrine. Discomfort that persists for more than 3-4 hours is grounds for re-visiting a doctor. In addition, incorrect implementation of the procedure, as a result of which part of the composition is washed out of the cavity, can cause complex chemical burns, leading to necrosis of adjacent tissues.
For young patients, the use of formulations containing arsenic is contraindicated, which is determined both by the structural features of the root system and by the inability of children to identify and formulate the sensations that arise in the postoperative stage. Instead, phenol-based drugs are recommended to create an anesthetic effect.
Electronecrosis
In situations where the use of chemical compounds is impossible due to an allergy to their components, a procedure for electronecrotization of the pulp is prescribed. As part of the procedure, the chamber is opened, followed by the introduction of a composition into the cavity that provokes necrotic changes or mummification, after which the pulp is removed completely or partially, depending on medical indications.
The technique allows the use of one of two protocols:
- One-stage – implemented without chemical killing, using anesthetics;
- Multi-stage – involves the preliminary use of chemicals.
After perforation of the chamber, the selected agent is applied to the exposed area, the volume and duration of its presence in the chamber is determined both by the specifics of the drug and the characteristics of the patient’s condition. The list of restrictions that exclude the operation includes an acute form of leukemia, severe cardiovascular pathologies, diagnosed stomatitis, as well as mental illness.
It is worth emphasizing that devitalization is applied only to affected teeth, the treatment of which does not give the desired result. Removing a nerve from a dental canal is a stressful situation against which the body requires a gentle regime. Compliance with medical instructions makes it easier for the patient to go through the rehabilitation phase.
Additional methods of treating pulpitis
Today, it is possible to ensure impeccable disinfection of root canals during treatment using modern equipment - ultrasonic, laser.
In addition, copper-calcium hydroxide depophoresis is an effective method of therapy. It has a bactericidal and fungicidal effect - it destroys pathogenic bacteria and fungi.
Physiotherapy for pulpitis is more often used as a means of treating pain after filling - it can occur due to adaptation to the material. In general, physiotherapy is used relatively rarely.
Cost of pulpitis treatment
The cost of treating pulpitis is determined by several factors, including the geography of the clinic. In a good clinic, the price already includes anesthesia, canal treatment, fillings and other materials.
The total amount is added up taking into account the number of root canals, their anatomical features, the degree of destruction of the crown and the method of its restoration, if we are talking about caries. You can find out the exact cost during a consultation with a dentist-therapist at the Dentist-K clinic.
It is important to remember that you can avoid expensive treatment by consulting a doctor in a timely manner. It is necessary to maintain hygiene and undergo professional teeth cleaning on time - this will avoid the need for pulpitis treatment.
How to prepare a child for treatment?
Treatment of pulpitis of primary teeth in children is a rather complex task, so it’s great if the child is already familiar with the dentist’s chair. The first visit should be preventative - to familiarize yourself with the office environment, the doctor, and the instruments.
Also, the task of parents is to psychologically prepare the child. Required:
- talk to your child about doctors in a positive way - tell them that the dentist treats teeth and makes sure they don’t hurt;
- play dentist with toys and other family members;
- avoid mentioning pain or unclear, scary terms;
- do not deceive the child - explain that dental treatment may not be very pleasant, but it will not last long and the tooth will no longer hurt;
- remain calm, act gently but confidently if the child resists treatment;
- choose a suitable time for visiting - it is better in the morning, when the baby is alert and active;
- take a toy with you to calm the child;
- give the doctor the opportunity to establish contact with the small patient - do not rush him;
- Do not scare the child under any circumstances, do not threaten, do not blackmail.
If the situation cannot be controlled completely, you will have to reschedule the appointment for another day. However, the disease should not be ignored - treatment of pulpitis of baby teeth in children must be carried out one way or another. In special cases, treatment under general anesthesia may be considered, but this should be discussed with your doctor.