From this article you will learn:
- how to treat aphthous stomatitis in children,
- symptoms and treatment of aphthous stomatitis in adults,
- list of effective drugs.
The article was written by a dentist with more than 19 years of experience.
Aphthous stomatitis is a disease in which one or more round ulcerations appear on the oral mucosa, which are covered with a necrotic coating of a gray or yellowish tint. Such ulcers (synonymous with aphthae) are not the result of acute infections, and therefore are not contagious, but nevertheless, such damage to the mucous membrane will require specific therapy.
According to statistics, up to 20% of the population suffers from this form of stomatitis. Young children, as well as adults aged 20 to 30 years, are especially susceptible to this disease. In people of more mature age, there is a dependence: the higher the age, the less likely it is to develop. Aphthous stomatitis has a code according to ICD 10 - K12.0. Below you can see what this disease looks like in children and adults.
Aphthous stomatitis in children: photo
Aphthous stomatitis: photos in adults
The most important thing in treating stomatitis is to first correctly determine its form. Indeed, depending on its form, and it can be either herpetic or aphthous stomatitis, treatment for both adults and children will be completely different. Therefore, if you are not very sure of the diagnosis, it is best to familiarize yourself with the symptoms of both forms before starting treatment.
Aphthous stomatitis: symptoms
If you suspect you have aphthous stomatitis, the symptoms are quite similar. A day or two before the onset of ulcers, patients usually notice a slight burning sensation in some areas of the oral mucosa. A little later, one or 2-3 clearly defined ulcers (aphthae) appear, covered with a necrotic coating of a gray or yellowish tint. The ulcers are round in shape and their diameter is usually no more than 1 cm, and along the perimeter they are surrounded by an inflammatory red halo.
Ulcers of this size usually heal within 10 to 14 days without scarring. However, in 10-15% of patients, the diameter of the ulcers may exceed 1 cm, and sometimes they can even reach 2-3 cm in diameter. Ulcers of this size are usually deeper than ulcers smaller than 1 cm (which may cause the ulcer border to appear raised). Healing of such ulcers usually lasts up to 6 weeks, and most often with the formation of scar tissue.
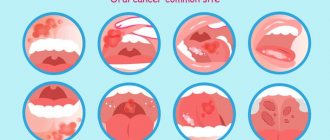
Important: the typical localization of ulcers is on the mucous membrane of the cheeks and the inside of the lips, on the soft palate (Fig. 7-8), tonsils, as well as the lower and lateral surfaces of the tongue. This localization is due to the fact that ulcers in aphthous stomatitis occur primarily on “non-keratinized” areas of the oral mucosa, i.e. where keratinization of the mucosal epithelium does not occur.
Less commonly, ulcers can occur on the keratinized mucous membrane (hard palate, dorsum of the tongue, tightly attached alveolar gum around the teeth) - this may be a signal of autoimmune diseases or HIV infection. In contrast to aphthous stomatitis, keratinized gums are affected precisely in herpetic stomatitis, which can also be a distinguishing feature of these two main forms of stomatitis from each other.
Foci of aphthous stomatitis on the soft palate (photo) –
→ Symptoms of herpetic stomatitis
ETIOLOGY OF HERPETIC STOMATITIS
The etiology of herpetic stomatitis is simple. If there is a virus, there are diseases. The virus that causes herpetic stomatitis belongs to the HERPES VIRIDAE family. This family includes about 80 different viruses, and, note, 8 of which cause human illness. Herpetic stomatitis is caused by the herpes simplex virus type 1 (HSV-1), and if it was a congenital or intrauterine (neonatal) infection, then this infection occurred with the herpes simplex virus type 2 (HSV-2).
It would seem that the virus is simple - the infection is simple. But the herpes simplex virus itself is very cunning and insidious. This virus, the herpes simplex virus, has come up with 4 ways of entering the human body:
- Airborne (therefore, it is recommended to avoid people with visible manifestations of the virus);
- Contact (lips affected by herpes are unlikely to give pleasant kisses);
- Transplacental (that is, from mother to child);
- Transfusion (with blood transfusion).
Causes of aphthous stomatitis –
The leading role in the development of recurrent aphthous stomatitis is played by the immune system, namely reduced “immunological reactivity”, as well as disturbances in the system of “nonspecific protective factors”. For parents, it is not necessary to know the details, but it is important to understand that such changes in the immune system are primarily caused by - 1) the presence of foci of chronic infection in the child, for example, this could be a sore throat, chronic tonsillitis or pharyngitis, 2) diseases of the gastrointestinal tract, 3) frequent stressful situations can also play a role.
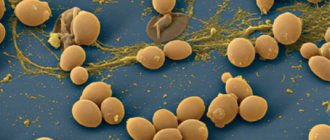
In patients with aphthous stomatitis, the following occurs: a decrease in the number and functional activity of T-lymphocytes - with a simultaneous increase in the number of B-lymphocytes, an increase in the level of serum immunoglobulins (antibodies) of the IgG class and circulating immune complexes. The result of all this is an excessive immune response to bacterial antigens. The main bacterial antigen for aphthous stomatitis is the α-hemolytic streptococcus Streptococcus sangui (absolutely all people have it, and in the normal state of the immune system it is not pathogenic).
An excessive immune response manifests itself in the development of an autoimmune reaction, which is also directed against the epithelial cells of the oral mucosa. This reaction involves both the cellular immune system (for example, neutrophils, mast cells) and humoral immunity (antibodies). As a result of the autoimmune process, foci of epithelial necrosis appear on the oral mucosa, i.e. Several ulcers form.
Additional factors –
But in addition to the main mechanism for the development of aphthous stomatitis (which we described above), some other reasons can lead to the development of aphthous stomatitis:
- food allergens,
- allergy to components of oral hygiene products (for example, parabens),
- large amounts of nitrates in drinking water and foods.
In addition, there is a large list of chronic diseases and conditions of the body that can also cause aphthous stomatitis or increase the risk of developing it (see list below). The risk of developing aphthous stomatitis will be higher if the patient has pathology of the gastrointestinal tract, immune system, blood disease, etc. Predisposing factors also include frequent biting of the mucous membrane of the cheeks and lips, as well as the use of toothpaste with sodium lauryl sulfate (SLS).
Important: a clinical study that revealed the effect of sodium lauryl sulfate, found in many toothpastes, on the development of aphthous stomatitis was published in the medical journal “Oral Diseases” (Jurge S, Kuffer R, Scully C, Porter SR. 2006). At the same time, you must understand that sodium lauryl sulfate is not an independent cause of ulcers on the mucous membrane, and that it only increases the risk of developing repeated outbreaks of aphthous stomatitis - in the presence of real reasons (for example, an excessive immune response to bacterial antigens, or in the presence of food allergies) .
The effect of lauryl sulfate is that it stimulates desquamation (squamation) of epithelial cells of the mucous membrane, which leads to a decrease in its thickness. A decrease in the thickness of the mucous membrane makes it more vulnerable to the real causative factors in the development of aphthous stomatitis (24stoma.ru). Therefore, in patients with recurrent aphthous stomatitis, it is better to use toothpaste without lauryl sulfate, as well as without parabens.
Systemic diseases and conditions of the body –
- during menstruation in women,
- in case of abrupt cessation of smoking,
- celiac disease, enteropathy, malabsorption,
- for hematological diseases,
- diseases of the immune system,
- with a lack of folic acid, vitamins B6 and B12,
- against the background of cyclic neutropenia, Behcet's syndrome, Reiter's syndrome, PFAPA syndrome (periodic fever, aphthous pharyngitis + cervical adenopathy), as well as against the background of systemic lupus erythematosus, reactive arthritis, inflammatory bowel diseases - especially Crohn's disease, as well as against the background of HIV .
What is the diagnosis based on?
The diagnosis of aphthous stomatitis is made based on visual examination, and in most cases does not require any laboratory tests. Only in severe forms or constantly recurring (recurrent) aphthous stomatitis is it necessary to conduct a complete blood count, which may indicate the presence of neutropenia or iron deficiency anemia.
As we said above, enteropathy may be the cause in about 5% of cases, and it can be diagnosed by detecting endomysial antibodies in the blood serum. Behcet's syndrome can be suspected if inflammation of the uvea (uveitis) occurs simultaneously.
Testing for HIV is always required if stomatitis recurs often or is severe, and especially if ulcers occur not only in areas of the mobile mucous membrane of the oral cavity, but also in areas of keratinized mucosa (for example, on tightly attached alveolar gums near the teeth , back of the tongue, hard palate).
PATHOGENESIS OF HERPETIC STOMATITIS
The pathogenesis of herpetic stomatitis is quite complex and not fully understood. It is not fully explained by what factors the inner shell of the virus is dissolved, what viral factors allow it to penetrate DNA - human cells, and why the virus, when it is inactive (that is, there are no clinical manifestations) cannot be treated.
However, scientists believe that at the time of infection, the herpes simplex virus attaches to specific receptors on the cell membrane (cells that are sensitive to HSV). Then the fusion of the cell membrane and the outer shell of the virus occurs. At the moment of such penetration, the cell membrane of the cell is not damaged, but the virus seems to bud inside. Then cellular enzymes work, those that dissolve the inner shell of the virus and the “naked” virus penetrates the DNA of the host cell. And the herpes simplex virus can remain in this state for a long time until the provoking factors work.
FACTORS PROVOKING RECURRENCE OF HERPETIC STOMATITIS
Factors that provoke relapse of herpetic stomatitis represent a large group. In principle, herpes can be triggered by anything, from climate change and time zone to ARVI and other infections. And so, the group of factors that provoke a relapse of herpetic stomatitis includes:
- Any change in body temperature (hypothermia is more favored by the herpetic stomatitis virus);
- Decreased immunity (any infection, etc.);
- Trauma to mucous membranes and skin;
- Stress, overwork or overexertion;
- Consumption of alcoholic beverages;
- Smoking;
- Menstruation;
- Change of climate and time zone;
- Taking medications.
As you can see from the lists, there are many factors, and the virus is just waiting for the body to give up. Children from 6 months to one year get sick due to the cessation of protective proteins from the mother. Therefore, let's talk about the prevention of herpetic stomatitis.
Aphthous stomatitis: treatment, drugs
Aphthous stomatitis in adults is the same as canker sores in children - the treatment is the same, and the treatment strategy described below is suitable for patients of any age. As for the medications listed later in the article, some of them do have age restrictions, which we will also indicate.
Due to the fact that it is usually impossible to clearly identify the specific cause of aphthous stomatitis in a particular patient, treatment will be multifocal, i.e. drugs of several groups are used simultaneously. The choice of treatment strategy and medications will depend on the following 3 factors:
1) on the severity of symptoms, 2) on the frequency of relapses, 3) on identified predisposing factors.
Treatment at the first stage should be aimed at reducing pain and inflammation in the area of ulcers, and at the second and third stages - at speedy epithelization of ulcers and preventing their occurrence in the future. To facilitate the choice of the best treatment option, all patients can be divided into 3 types (according to the criteria - severity of the disease and frequency of relapses).
- Type A - in patients of this type, aphthous stomatitis occurs no more than several times during the year and is characterized by slight pain.
First of all, in such patients it is necessary to identify local predisposing factors and eliminate them (for example, overhanging edges of fillings or hygiene products with sodium lauryl sulfate). It is important to ask the patient about eating habits to evaluate a possible relationship between stomatitis outbreaks and certain foods. The patient is advised to avoid solid foods (eg, crackers, toast), all types of nuts, chocolate, eggs, acidic drinks or foods - fruit or citrus juices, tomatoes, pineapples, salty foods. You should avoid eating spicy foods, any spices, including pepper and curry, as well as alcoholic and carbonated drinks. In type A patients, local symptomatic therapy is mainly used, which includes antiseptic rinses and gel applications for pain and inflammation + antihistamines.
- Type B - in such patients, aphthous stomatitis develops almost monthly, and the ulcers are so painful that they force the patient to change habits (for example, brushing teeth less often due to severe pain). It remains important to identify local and general predisposing factors and, if possible, eliminate them. It is very important to teach patients of this type to feel the first signs of the imminent appearance of ulcers - burning, itching or swelling of the mucous membrane, in order to provide early local treatment even before the formation of the ulcers themselves.
- Type C - in patients of this type, ulcers are very painful, appear so often that while one lesion is healing, the next one appears almost immediately. This group also includes patients in whom local treatment in the oral cavity is completely ineffective, and improvement in their condition occurs only after the use of systemic therapy (we will also discuss such therapy below).
PREVENTION OF CANDIDOSAL STOMATITIS
Prevention of candidal stomatitis includes:
- Competent prescription and use of antibiotics, antidepressants, etc.;
- Timely treatment of diseases;
- Pregnancy planning;
- Thorough cleaning of rooms;
- Whitening only washed vegetables and fruits, fresh meat and dairy products;
- Visit the dentist at least once every six months;
- Mothers should provide their baby with clean nipples and bottles and not neglect hygiene.
Thanks for reading! Take care of yourself and your loved ones!