Bacterial stomatitis: before and after photos
The causes of infection may be:
- pockets of bacteria accumulation on carious teeth;
- germs entering the mouth due to herpes;
- infection during treatment - bacterial stomatitis can develop if the doctor does not comply with antiseptic rules;
- chronic diseases of various organs;
- contact with a sick person (for example, a kiss).
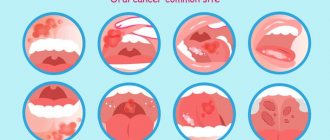
Symptoms of infectious stomatitis are, first of all, redness of the oral mucosa in the place where microbes entered the wound, swelling, and in the necrotic form, a rash. In children, cracks may form in the mucous membrane, and the gums begin to bleed. The damaged area is itchy and painful.
If bacterial stomatitis is not treated, the temperature rises, a headache appears, the lymph nodes and tonsils become inflamed, and due to intoxication of the body, the rash spreads throughout the body. Children may develop a sore throat and experience pain in the knee joints.
How to treat the disease
Therapy involves the use of local and sometimes systemic drugs. The treatment regimen for the disease depends on what type of stomatitis is diagnosed. For this reason, you should not self-medicate, as it may turn out to be useless and the pathology will continue to develop into dangerous conditions.
The exception is mild catarrhal inflammation associated with poor hygiene. It is enough to exclude the cause and rinse your mouth with antiseptics for several days.
Treatment at home for other types should be discussed with your doctor. The use of folk remedies is not contraindicated, but they can only be used as a supplement to the main therapy. Only a dentist can evaluate the appropriateness and harmlessness of a particular prescription.
Effective drugs for adults
To relieve inflammatory processes, combat pathogenic microflora, and relieve pain, rinses, gels, sprays, lozenges, and ointments are prescribed. For severe pain, pain medications can be taken orally. Since treatment must be carried out regularly, it is important to choose a medicine for stomatitis that will be convenient to carry in your purse and use at work.
Popular medicines:
- Chlorophyllipt, Inhalipt, which have an antiseptic effect. Available in the form of sprays. Apply up to 5 times a day for one week. Sprays are convenient to use if there is stomatitis in the palate or throat.
- Solcoseryl accelerates tissue regeneration, restores mucous membranes, and protects against the development of ulcers. The gel is applied several times a day. The course is from 7 to 14 days.
- Cholisal has a detrimental effect on bacteria, relieves inflammation, and improves tissue healing. The gel is used three times a day for at least a week. An analogue of the drug is Kamistad. Excellent help with aphthous, bacterial form of the disease.
- Viferon, Acyclovir are prescribed to patients with a viral infection. Ointment for stomatitis in the mouth is applied to areas of inflammation several times a day. The course of therapy is up to 2 weeks.
- Lidocaine Asept, Lidochlor are used for any form of pathology, since the main purpose is to relieve acute pain. Available in spray form. Can be used up to four times a day, no more than 1 week.
- Lugol kills bacteria, treats ulcers, and relieves inflammatory processes. The oral cavity is treated with a spray 2 - 3 times a day.
- Miconazole and Nystatin are prescribed for fungal infections. In severe cases of the disease, the ointment is used in combination with systemic medications. Apply to affected areas 2 to 4 times a day.
Any medication for stomatitis must be prescribed by a doctor. The symptoms of the varieties of the disease are similar and it is impossible to independently understand the cause of the inflammatory reactions.
What can you rinse your mouth with?
To treat pathology, you can use pharmaceutical drugs aimed at destroying bacteria, reducing inflammation and healing tissue.
Medicinal solutions that can be bought at the pharmacy:
- Aqualor with sea salt;
- Stomatofit, Dr. Theiss Sage based on sage;
- Romazulan with chamomile extract;
- Chlorhexidine (pre-diluted with water).
Decoctions and infusions for rinsing are easy to prepare at home from chamomile, calendula, aloe juice, sea buckthorn, linden flowers and other medicinal plants. A solution of salt and soda helps a lot.
Treatment of bacterial stomatitis
Self-medication for infectious stomatitis is completely excluded, since it is necessary to accurately identify the pathogen and select drugs that suppress it. Such studies are carried out in the laboratory. This is especially important when it comes to babies. To prevent possible complications, parents of a baby should immediately consult a doctor as soon as they see an inflamed scratch or swelling in the child’s mouth.
When treating bacterial stomatitis, the following are used:
If necrosis has developed, dead tissue is removed surgically, after which it is necessary to completely sanitize the oral cavity.
In parallel with medical measures to eliminate the symptoms of bacterial stomatitis, the patient is prescribed a diet. During this period, it is necessary to ensure maximum sparing of the oral mucosa, limit the consumption of carbohydrates and enrich the diet with vitamins and proteins.
- Superficial (catarrhal). In this case, symptoms of intoxication manifest themselves in a deterioration in appetite and an increase in temperature. There is discomfort when chewing and swallowing food, and the secretion of saliva periodically increases. When examining the oral cavity, a white coating on the tongue is found (on its lateral surfaces there are clearly visible imprints of teeth), bleeding gums, and hyperemia of the mucous membrane. Lack of treatment for catarrhal bacterial stomatitis leads to the disease progressing to the next, more severe form.
- Deep (ulcerative-necrotic). The patient's condition worsens. Symptoms of intoxication intensify: a person has a headache, the temperature rises to high levels, sleep and appetite are disturbed, weakness, irritability, and lethargy appear. Also, bacterial stomatitis in this form is characterized by pain when chewing, bad breath, and increased salivation. When examining the oral cavity, bleeding gums, hyperemia of the mucous membranes, and the presence of ulcers are revealed - first small, covered with a grayish coating, then enlarged, deep, with traces of tissue decay. Immunostimulants. They are necessary to boost immunity and prevent new outbreaks of the disease. These drugs have local and general effects. The doctor selects the optimal treatment option depending on the patient’s condition. For the same purpose, it is recommended to take a course of vitamins.
- Antibiotics. They are prescribed when bacterial stomatitis has become severe or the cause of the disease is systemic diseases of the internal organs. Effective remedies that stop infection directly in the oral cavity are ointments that contain an antibiotic. They give excellent results if the causative agent is a coccal infection. Among the drugs for oral administration in the treatment of bacterial stomatitis, penicillin, lincomycin, gentamicin, kanacimin and others are used.
- Antiseptics. At the initial stage and in the middle of the disease, rinsing with a chlorhexidine solution and treating the mucous membranes of the oral cavity with an anti-inflammatory gel with an analgesic effect are recommended. After the disappearance of acute symptoms, treatment of bacterial stomatitis continues with the help of epithelializing agents that promote rapid healing of defects.
Reasons for development
Stomatitis often occurs in people with reduced immunity and impaired microflora. If these 2 conditions are observed simultaneously, then even opportunistic microorganisms can cause severe inflammatory processes. Many other factors also influence the development of the disease.
Inflammation of the oral mucosa can occur in the following cases:
- mechanical, chemical, thermal injuries - hot burn, injury from solid food, cheek bite, etc. leads to tissue damage, penetration and spread of infection;
- poor nutrition, lack of vitamins, especially C, group B, minerals - zinc, iron and others;
- failure to comply with hygiene rules, eating unwashed fresh berries, vegetables, fruits, dirty hands while eating;
- treatment with medications that reduce salivation, antibiotics that destroy beneficial microflora, and a number of other medications;
- Frequent brushing of teeth with a paste containing sodium lauryl sulfate leads to a decrease in saliva secretion and dry mucous membranes, which become more susceptible to aggressive substances;
- poor-quality prosthetics and dental treatment due to which the gums are constantly injured;
- smoking, drinking alcohol;
- dehydration with prolonged diarrhea, vomiting.
Stomatitis often occurs during pregnancy due to hormonal imbalance. At risk are patients with diseases of the heart, blood vessels, gastrointestinal tract, pathologies of the immune and endocrine systems, and those with helminthic infestation. In diabetes mellitus, the aphthous form is diagnosed. People who use hormone inhalers to relieve asthma attacks suffer from candidiasis.
To answer the question whether stomatitis is contagious or not, differential diagnosis is necessary. Bacteria, viruses, and Candida fungi can be transmitted from person to person. The most contagious is the viral form of the pathology. However, with good immunity, the infection will not necessarily develop. It is also important how stomatitis is transmitted. If this is direct contact, for example a kiss, then the risk of getting sick is higher.
Prevention
In the oral cavity of any person there is a conditionally pathogenic microflora, which can be activated when immunity decreases. For this reason, it is important to lead a healthy lifestyle, eat well, and treat illnesses.
Hygiene rules must be observed. Do not eat dirty vegetables, wash your hands before eating, and replace your toothbrushes regularly.
For persons predisposed to the disease, any trauma to the oral mucosa should be excluded. Do not eat scalding, hard foods or spicy seasonings. If a wound appears, you should immediately treat it with an antiseptic.
It is imperative to carry out timely treatment of dental and ENT diseases. Chronic diseases and advanced caries are sources of infection.
Diagnosis of the disease and its differences from other pathologies
The doctor receives the first data after examining the patient’s mouth. Next, the doctor collects an anamnesis of the disease and the patient must answer when the first symptoms appeared, how quickly the disease developed, whether there were injuries (including burns) to the oral cavity, allergies to foods and medications, whether close relatives suffered from stomatitis.
To identify the causative agent of the disease, you will need to take a smear on the flora and exclude manifestations of herpes and candidiasis. For this purpose, laboratory tests are used - bacterial culture and PCR smear.
For persistent stomatitis, you should check your blood glucose level.
Symptoms of aphthous stomatitis
The onset of acute aphthous stomatitis in children may resemble ARVI: there is malaise, increased body temperature, and more profuse salivation may appear. The main symptom of the disease is the appearance of ulcers in the mouth: first, a red dot appears on the mucous membrane, which subsequently becomes an ulcer (aphtha) within 2-3 days. Accidental touching causes pain. The child refuses food and hygiene procedures.
Single erosions occur more often, but there are cases of multiple aphthae formed in groups. They usually measure up to several millimeters, but in severe cases the diameter of the ulcer reaches one centimeter. The disease is characterized by the appearance of a bright red rim around the aphthae; a grayish or yellow film-like coating forms on it.
There are also general symptoms that accompany aphthous stomatitis. These include:
- sleep disturbances (due to pain or discomfort);
- decreased appetite;
- pain while talking;
- increased fatigue, lethargy;
- whims, irritability.
Early treatment of aphthous stomatitis in children can prevent complications, shorten recovery time, and prevent further development of the disease.
How to recognize the disease
It is not difficult to understand that discomfort in the mouth is associated with stomatitis. At first, mild swelling appears. In certain places, the mucous membranes become red and more shiny. Afterwards, zones covered with plaque form on their surface. Then the person begins to feel severe itching and burning.
Gradually, painful lesions turn into ulcers (aphthae) and oval or round wounds. Most often they are located on the palate, under the tongue, on the inner surface of the lips and cheeks. Due to aphthae, normal eating becomes impossible - when trying to eat something solid, a person experiences acute pain.