About the prevention and treatment of common childhood dental diseases, the causes of candidiasis (thrush) and stomatitis. How can I help my child maintain oral hygiene? Note to parents.
Every parent, when visiting a pediatric dentist, wonders when can they start brushing their teeth? There are many opinions on this matter; some even argue that it is not necessary to clean dairy products. But this is a mistaken opinion. It is known that dental plaque contains pathogenic microorganisms that contribute to the occurrence of caries. It is necessary to accustom your child to brushing his teeth from the age of one. At first, the parent takes care of this himself, and later controls the process. By the age of one year, on average, a child has 8 to 12 teeth. If parents find it difficult to use a toothbrush, you can clean off plaque with gauze wrapped around your finger. This will reduce the trauma that can occur from a toothbrush, because... the child does not immediately begin to understand the meaning of this process. Later, you can start brushing with a soft-bristled toothbrush; you can find one in every pharmacy. There is a variety of choices, both in terms of external indicators and age.
Children's pastes are also varied. You can consult your dentist about your choice. When a child begins to brush his teeth on his own, parents should supervise this process, because children often do it in bad faith, for a short time. It is recommended to clean for up to 5 minutes, removing plaque from top to bottom.
Even despite hygiene, the child is not insured against such childhood diseases as candidiasis and stomatitis. Outwardly they are very similar, parents often confuse them. How to distinguish them and how to treat them?
ETIOLOGY OF CANDIDOSAL STOMATITIS
The etiology of canida stomatitis, as you could understand above, is simple. That is, the cause of candidal stomatitis is yeast-like fungi of the genus Candida. Let's get to know them. These fungi are classified as imperfect fungi, DEUTEROMYCETES, which have a complex structure. Firstly, they have a cell wall, which consists of 5-6 layers, secondly, they have a perforating organ that affects the host cells, and thirdly, they have significant differences in comparison with other yeast-like fungi.
The difference between fungi of the genus Candida and other yeast-like fungi is as follows:
- Ability to grow in an environment with a temperature of 30 -37 degrees Celsius;
- The optimal environment is slightly acidic/acidic (pH = 5.8 – 6.5)$
- Ability to ferment carbohydrates (main source of nutrition);
- Aerobes (love oxygen);
- Choose media with glycogen.
In general, candida is a conditionally pathogenic fungus, which means that in the absence of factors, they are basically safe. But as soon as changes occur in this balance, they become pathogenic. That is, you need to know and understand exactly what conditions lead to the activation of the pathogenicity of fungi of the genus Candida. After all, the main role here is played not by pathogenicity factors, but by the state of the immune defense of the human body. Of course, the pathogenicity of Candida fungi for animals and humans is different. For humans, the most dangerous is Candida albicans, for children - Candida tropicalis.
PREDISPOSIBLE FACTORS TO CANDIDOSAL STOMATITIS
Factors that contribute to the activation of pathogenic factors by candida are the following:
- A decrease in the body’s defenses - immunity (and who else remembers anything, let me clarify: namely cellular immunity);
- The presence of congenital or acquired immunodeficiencies;
- Metabolic disorders, endocrine disorders (for example, diabetes mellitus, amenorrhea, iron deficiency, etc.)
- Vitamin deficiencies (especially vitamins B1, B2, B12, which are involved in suppressing the action of microorganisms)
- Acute infectious diseases, or exacerbations of chronic diseases;
- Diseases of the female genital organs;
- Long-term use of oral contraceptives;
- Pregnancy;
- Large burns;
- Rickets;
- Prematurity;
- Oncology;
- Diseases of the gastrointestinal tract;
- Taking antibiotics, large doses of drugs, immunosuppressants;
- Working conditions. It was noticed that people working in hydrolysis-yeast factories, in factories for the production of antibiotics, beer and other alcoholic beverages, more often than others suffer from candidal stomatitis;
- Failure to comply with personal hygiene rules;
- Failure to maintain cleanliness and order in household items (candida can be found on children's toys, plates, cups, etc.);
- Eating unwashed vegetables and fruits;
- In infants, candidal stomatitis most often forms when they are overheated, that is, when wearing tight pajamas, bulky swaddling, etc.
- Artificial feeding of children up to 6 months;
- Iatrogenic factors: acute damage to fillings, incorrectly fitted dentures, chemical burns from formaldehyde, arsenic pastes, etc. That is, everything that leads to disruption of the integrity of the oral mucosa.
As you can see, there are a lot of reasons and facts for the activation of Candida. Therefore, the approach to treatment must be adequate, and the CAUSE must be treated first, and only then the manifestations.
PATHOGENESIS OF CANDIDOSAL STOMATITIS
The pathogenesis of candidal stomatitis is quite simple: the fungus is located on the surface of the oral mucosa or on the surface of the skin, and in the absence of damage or provoking factors, it does not penetrate the epithelium; if present, it is clear that it penetrates and visible pathology begins.
However, these are only two of the FIVE mechanisms of action of mushrooms on the body. Candidiasis is a very serious problem, because it can spread to organs. Thus, after penetration into the epithelium, Candida is able to interact with macrophages and neutrophils. After which it penetrates into the cells of organs such as the liver, heart, kidneys - granulomas are formed. And the very last and ominous stage is penetration into the blood and the development of candidemia. After which death occurs.
Therefore, in order to prevent this, read on and remember J
CLASSIFICATION OF CANDIDOSAL STOMATITIS
- Classification of candidal stomatitis according to ICD-10:
- AOO-B99 Some infectious and parasitic diseases;
- B35-B49 Mycoses;
- B37 Candidiasis
- B37.0 Candidal stomatitis - oral thrush.
- Classification of candidal stomatitis N.D. Sheklakov:
- Superficial candidiasis of mucous membranes, skin, nails;
- Chronic generalized (granulomatous) candidiasis;
- Visceral (systemic) candidiasis.
- With the flow:
- Acute pseudomembranous candidiasis (thrush);
- Acute atrophic candidiasis;
- Chronic hyperplastic candidiasis;
- Chronic atrophic candidiasis.
SYMPTOMS OF CANDIDOSAL STOMATITIS
In the future, we will look at the symptoms of candidal stomatitis, even each form separately. Here I will only indicate common symptoms with which a patient may seek help.
Symptoms of candidal stomatitis:
- Pain when eating;
- Pain at rest;
- Burning;
- Itching;
- Dry mouth;
- Bad breath;
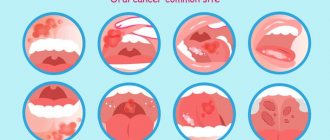
- Presence of spots on the mucous membrane;
- Perversion (change) of taste;
- Bleeding gums;
- Enlarged lymph nodes;
- Increased body temperature;
Most often, wounds are located on the mucous membrane of the cheeks, palatine tonsils and lips on the inside. Less often on the tongue and under the tongue.
Stomatitis
Stomatitis in a child
There are several types of stomatitis, the most common are herpetic and aphthous . It differs from candidiasis in that it is accompanied by high fever. Bubbles and aphthae appear on the tongue, soft palate, and gums. The child stops eating due to severe pain. Most often, children in kindergartens suffer from stomatitis. They are constantly in contact and put toys in their mouths. If one child gets sick with viral stomatitis, the other is more likely to get infected from him. One of the reasons for refusing a pacifier is not only a violation in the formation of the bite, but also hygiene. Repeatedly, infection occurs from a child who brought a pacifier to kindergarten and lent it to his friends. Reduced immunity can provoke the disease; if relapses occur, laboratory tests are prescribed to rule out common diseases.
Treatment
Treatment for general symptoms of stomatitis is prescribed by a local pediatrician and locally by a pediatric dentist. It includes treating aphthae with sea buckthorn oil, some recommend an aqueous solution of blue, before eating they recommend painkillers gels, soda gargles, and spraying the throat with aerosols. As a rule, stomatitis disappears suddenly, just as it began, and good immunity copes with the disease.
Every parent faced with such problems panics.
These diseases are treated almost every day. This is not a reason to worry, because... everything is treated in a short time, and maintaining hygiene, monitoring the child’s behavior, weaning from bad habits completely eliminates these problems. Moscow metro station Zvezdnaya, Danube Avenue, 23
DIAGNOSIS OF CANDIDOSAL STOMATITIS
Diagnosis of candidal stomatitis will be based on the patient’s data and clinical examination by a specialist. In addition, to confirm the diagnosis of CANDIDOSAL stomatitis, it is necessary to conduct laboratory diagnostics. To do this, I make a scraping (smear) from the surface and send it to the laboratory. In the laboratory, materials are studied in 2 directions:
- Sowing on nutrient media - Sabouraud's medium, wort - agar or candida - agar;
- Microscopy of stained smears.
Isolation of 300 colonies in 1 ml indicates candidiasis. Detection of a larger number of colonies during initial culture indicates candidiasis. But the diagnosis will be confirmed only with repeated culture and when the numbers are higher than 300 colonies per 1 ml.
ACUTE PSEUDOMEMBRANOSUS CANDIDIASIS
Acute pseudomembranous candidiasis is the most common form of candidiasis of the oral mucosa. It is acute pseudomembranous candidiasis that is thrush, and not any other types of candidiasis. What I mean is that not every stomatitis or candidiasis is silent. Infants and weakened adults are more often affected.
Symptoms of acute pseudomembraous canidosis:
- Complaints about the child refusing to feed;
- Children are lethargic and capricious;
- Complaints of pain when eating, burning and dry mouth.
Clinic of acute pseudomembraous canidosis:
On the mucous membrane of the oral cavity there are white or blue-white spots - a coating similar to “curdled masses”. Which in some cases are easily scraped off and the hyperemic surface is exposed. In other cases, the plaque is difficult to scrape off, bleeds, and an eroded surface is revealed. The process most often affects the tongue, palate, lips, but can spread to the pharynx, larynx and esophagus. If there is no treatment, acute pseudomembranous candidiasis turns into acute atrophic candidiasis.
ACUTE ATROPHIC CANDIDIASIS
Symptoms of acute atrophic candidiasis:
- Complaints of dryness and burning in the mouth;
- Pain when chewing, when talking;
- Inability to open your mouth wider;
- Complaints about scales on the lips;
- For dry and cracked lips.
Clinic of acute atrophic candidiasis:
The clinic of acute candidal stomatitis differs from the clinic of acute pseudomembranous canidosis in the ABSENCE of plaque.
In acute atrophic candidiasis, the mucous membrane is hyperemic, it is very red, it is called fiery, and it is also dry, which makes it difficult to open the mouth. There is no raid. On the tongue there is atrophy of the papillae (that is, smoothness of the pattern), the tongue is smooth and bright red. There may be teeth marks on the tongue. The red border of the lips is hyperemic, dry, with the presence of gray scales. There are cracks and erosions in the corners of the lips.
CHRONIC HYPERPASTIC CANDIDIASIS
Symptoms of chronic hyperplastic candidiasis:
- Complaints of pain when eating spicy, hot food;
- Perversion (change) of taste;
- Burning in the mouth.
Clinic of chronic hyperplastic candidiasis:
The appearance of plaques (“cobblestones”) is noted on the hyperemic mucosa. Plaques are gray-white, tightly adhered to the mucous membrane, which, when removed, contributes to bleeding and pain. Most often they are located on the back of the tongue. May spread to the tonsils, pharynx, throat and esophagus.
CHRONIC ATROPHIC CANDIDIASIS
Most often, chronic atrophic candidiasis is diagnosed in patients with oral dentures.
Symptoms of chronic atrophic candidiasis:
- Complaints of burning;
- Complaints of pain when eating;
- Complaints of dry mouth
Clinic of chronic atrophic candidiasis:
The mucous membrane under the prosthetic bed is swollen and hyperemic. In some places there is an easily removable white coating. When removing white plaque, the surface becomes hyperemic. In the corners of the mouth there are erosions, also covered with a white coating. There may be damage to the tongue: the tongue is smooth, the papillae are atrophied, teeth marks are on the tongue. In some cases, hypertrophy of the filiform papillae is noted - “black hairy tongue”
Candidiasis (thrush)
Candida
enter the oral cavity . In children, thrush is often confused with stomatitis. It is most often transmitted from poorly washed, unsterile nipples, bottles, as well as from an infected mother, through the birth canal, with low immunity. Most children get sick before they are one year old. Parents complain about a white, curd-like coating.
Treatment
Infants are not prescribed serious medications for uncomplicated cases. The dentist recommends cleaning this plaque with a soda solution (1 teaspoon per glass of warm water). An ear stick, as an option. The same solution is used to treat nipples, bottles, toys, and mother's nipples during breastfeeding. In most cases, candidiasis quickly passes without leaving a trace. Prevention includes regular monitoring of the sterility of items used by the child.
TREATMENT OF CANDIDOSAL STOMATITIS
Treatment of candidal stomatitis should be strictly individual. After all, most often, as I said earlier, candidal stomatitis is a secondary disease, so it is necessary first of all to look for the cause and eliminate it.
Treatment of candidal stomatitis should be both general and local.
General treatment for candidal stomatitis is:
- Prescribing general restorative therapy;
- Prescribing antifungal drugs;
- Prescribing diets excluding sweets and other carbohydrates. Food should be rich in fiber.
Preference is given to polyene antibiotics as the main remedy for the treatment of candidal stomatitis. Examples of drugs would be nystatin, levorin (it is advisable to dissolve the tablet and throw it away, since polyene antibiotics are poorly absorbed by the body). In parallel, multivitamin complexes with B vitamins, calcium and iron are prescribed. Desensitizing therapy is also carried out with drugs such as diphenhydramine and suprastin.
Local treatment of candidal stomatitis consists of:
- In the application of polyene antibiotics to the mucosa in the form of solutions or ointments for 14 days, 3-4 times a day;
- In the appointment of alkaline applications with 2-4% sodium bicarbonate solution.
- A thorough sanitation of the oral cavity, professional hygiene, and replacement of old and irrational orthopedic structures are carried out.
Treatment of candidal stomatitis in adults
How to treat the disease “candidal stomatitis”?
First of all, at the first signs of the appearance of red sores, it is necessary to contact a specialist who must correctly diagnose the disease and prescribe treatment. Quick and timely diagnosis is the key to successfully overcoming the disease and eliminating discomfort.
Most often, in the treatment of candidal stomatitis, drugs from the group of antifungal agents are prescribed. Depending on the stage and form of the disease, they are taken 4-7 times a day until any signs of thrush completely disappear. Be sure to consult your doctor before using any medications!
Also during treatment it is necessary to use local antifungal agents, such as:
- A solution of baking soda in water (a teaspoon per glass of water). For better dissolution, the water should be warmed up a little.
- Drops with nystatin.
- Lotions with potassium permanganate. Potassium permanganate dissolves at a rate of 1 to 10,000.
- Asepta rinse solution. It contains an anesthetic component that relieves discomfort. The rinse aid is convenient because it does not require preparation and is immediately ready for use. You can take it with you to work and periodically rinse your mouth with it throughout the day. The solution has an excellent disinfectant effect and relieves burning sensation.
PREVENTION OF CANDIDOSAL STOMATITIS
Prevention of candidal stomatitis includes:
- Competent prescription and use of antibiotics, antidepressants, etc.;
- Timely treatment of diseases;
- Pregnancy planning;
- Thorough cleaning of rooms;
- Whitening only washed vegetables and fruits, fresh meat and dairy products;
- Visit the dentist at least once every six months;
- Mothers should provide their baby with clean nipples and bottles and not neglect hygiene.
Thanks for reading! Take care of yourself and your loved ones!