Mechanical trauma is the most common type of damage to permanent and temporary teeth in children. It leads to a violation of the anatomical integrity, changes in the dentition or destruction of surrounding tissues. According to statistics, the front teeth, including the upper incisors, are most often susceptible to traumatic damage in children aged 6-10 years. The lack of proper treatment in this case often leads to serious complications, which can manifest as inflammatory-destructive processes, the appearance of cysts and other negative consequences.
Causes of dental damage in children
The increase in injury cases is primarily due to the growing popularity of team, contact and other sports. For example, hockey, wrestling, boxing, football and others. Also, the cause of dental damage in children of different ages can be accidental falls during active games on the street or school. No less common are injuries sustained in everyday life, fights, road accidents and other cases where there is a high probability of being hit by a hard object.
The risk of tooth damage increases if a child has orthodontic pathologies. For example, in patients with a distal bite (with protrusion of the upper jaw), injuries occur 5 times more often than in those with an orthognathic (normal) bite.
Also, dental damage often occurs in children with visual impairments, problems with the musculoskeletal system and various neuropsychiatric diseases.
What is tooth luxation
A small piece of connective tissue called the periodontal ligament helps hold the segment in the alveolar ridge. It is a cluster of collagen fibers penetrated by capillaries and nerves. The ligament is very thin. On the inside, the tissue is attached to the cement of the tooth root. From the outside - to the bone surrounding the unit.
During dental trauma, damage to the ligamentous apparatus and neurovascular bundle occurs. Due to the forced action, the fibers cannot support the segment, which leads to its deviation.
Classification of injuries to children's teeth
The nature and severity of the damage is determined based on a comprehensive examination of the patient using radiological, clinical and other methods. To make a diagnosis, dentists today use different systems for diagnosing trauma to children’s teeth.
Standard ELLIS classification
This system of dividing acute injuries into separate types, developed by Ellis, is the very first and most used in practice. It includes 9 categories of dental damage:
- I – slight fracture of the crown within the tooth enamel;
- II – moderate crown fracture extending into enamel and dentin;
- III – severe fracture of the crown with exposure of the pulp;
- IV – loss of pulp viability in the presence/absence of a crown fracture;
- V – complete dislocation of the injured tooth;
- VI – damage with root fracture;
- VII – slight subluxation of an injured tooth;
- VIII – fracture of the crown in the cervical area;
- IX – trauma to baby teeth.
Types of Traumatic Injuries WHO
Actively used in modern dentistry along with ELLIS. This classification was developed based on the Andresen system and includes, in addition to dental injuries, damage to other tissues (oral mucosa, gums, periodontal tissue, bones).
I. Damage to pulp and hard tissue:
- cracks in tooth enamel (A);
- fracture of the crown without opening the pulp (enamel affected - B, enamel and dentin affected - C);
- fracture of the dental crown exposing the pulp (D);
- combined root and crown fracture with pulp exposure (E);
- trauma with root fracture (F).
II. Periodontal damage:
- shock of the tooth with a weak response of periodontal tissue to percussion without increasing its mobility and displacement (A);
- subluxation with change in mobility without displacement (B);
- penetration of the injured tooth deep into the tissues (C);
- exit of the tooth from the anatomical socket (D);
- displacement in a direction other than axial (E);
- complete dislocation of the injured tooth (F).
III. Bone injury:
- tight connection of the tooth with the socket with penetration deep into the tissue (A);
- fracture of the wall of the anatomical recess (B);
- fracture of the alveolar bone tissue (C, D);
- fracture of the jaw bone (upper – E, lower – F).
IV. Injury to the gums and oral mucosa:
- acute soft tissue injury (A);
- bruise of the mucous membrane or gums (B);
- soft tissue detachment (C).
Classification of injuries to children's teeth according to ICD-C
This is an international system for defining acute injuries, based on ICD-10 (1997). Used in pediatric dentistry to classify various injuries, including fractures of primary and permanent teeth (S02.5):
- fracture (chip) within the thickness of the enamel (S02.50);
- fracture of the dental crown without injury to the pulp (S02.51);
- crown fracture with injury extending to the pulp (S02.52);
- fracture of the root part of a permanent tooth (S02.53);
- double fracture in the area of the dental crown and root (S02.54);
- multiple fractures of different locations (S02.57);
- unspecified fracture of primary or permanent tooth (S02.59).
Types of tooth dislocations
| Variety | Description |
| Incomplete | Incomplete tooth dislocation is characterized by partial displacement of the root in the socket, rupture or stretching of part of the fibers of the periodontal ligament. The position of the tooth is disturbed: it deviates to the vestibular, oral or lateral side. Rotation around an axis is possible. The injury may be of a combined nature (with a fracture of the supra-, subgingival part of the unit, the bone of the alveolar process). |
| Full | Complete damage (traumatic extraction, avulsion) is characterized by loss of a segment from the alveolus, rupture of the fibers of the circular dental ligament, nerves, and blood vessels. The most common condition is complete dislocation of the front tooth (central incisors) of the upper jaw. |
| Hammered | Intrusion is the depression of an injured unit under the influence of a blow into the depths of the alveoli. Immersion can be complete or partial. With such an injury, the root enters the spongy jawbone. The periodontal ligament is usually completely torn. Some fibers are sometimes preserved, but they undergo stretching. Capillaries and nerve bundles also break. The bottom and walls of the cortical plate break down. At the same time, the segment can deviate to the side and rotate around its axis. If the injury is localized in the upper jaw, there is a risk of damage to the maxillary sinus. Impacted tooth dislocation has a poor prognosis. Almost all cases of injury (especially with a late start of endodontic treatment) end in resorption. |
Procedure for providing assistance to children with dental damage
Immediately after receiving an injury, the patient is provided with primary medical care, which includes a general assessment of the child’s condition, pain relief, prescription of antibiotics, anesthetics and other medications, as well as a preliminary diagnosis. After this, the patient’s parents are given a recommendation to make an appointment with a pediatric dentist (therapist), who will carry out full dental treatment. The doctor providing specialized care carries out:
- registration of a medical history (including legal and social aspects of the case);
- collecting anamnesis (origin of injury, presence of concussion, local symptoms);
- clinical examination of the injury (visual examination, percussion, palpation, temperature tests of the pulp, instrumental methods);
- additional diagnostics (electroodontodiagnostics (EDD), transillumination, targeted radiography, occlusal radiography, computed tomography);
- making a diagnosis based on examination, clinical and other studies;
- choice of treatment tactics taking into account the nature of the damage, possible risks, benefits and costs.
The period of rehabilitation of a child after an injury, starting from the moment of emergency assistance, can take 1-3 or more days. Given the complexity of treatment, the period of complete restoration of the integrity and functions of damaged teeth often takes a longer period - several months or even years.
Symptoms of tooth dislocation
The clinical picture depends on the type of dislocation:
- If the periodontal ligament is incompletely damaged, the patient complains of pain (especially when chewing), loosening of the causative unit, and a change in its position in the row. The displacement can occur in different directions. The gums in the pathological area are swollen and hyperemic. Bleeding from the periodontal pocket is possible.
- Symptoms of avulsion: absence of a segment in a row; in place of the lost tooth there is a fresh hole filled with a clot (or bleeding). Associated signs: pain, bruises, wounds on the gums and lips.
- Signs of intrusion: the segment has become shorter compared to neighboring units (or has completely disappeared into the alveolar bed), and reacts with increased sensitivity to percussion. The pathology is often accompanied by alveolar bleeding and soft tissue injuries of varying severity.
Tooth fracture without pulp exposure
In dentistry, a fracture is understood as an injury in which the enamel prisms diverge from each other, and part of the dental tissue is lost. In the event of a fracture, the prisms are not only separated, but also parts of them are lost. The fracture can also pass through dentin, but in this case the dental pulp remains intact.
X-ray
When conducting radiographic studies, if a child’s tooth has chipped, it is not difficult to determine serious damage, while it is almost impossible to recognize a crack in the picture.
Treatment and postoperative monitoring
For small chips, grinding down the enamel is possible, but for more extensive damage, a composite tooth restoration may be required.
In cases where the patient was able to save the chipped tooth fragment, it is possible to fix it in place using adhesive bonding techniques. The technology for performing the work is fully consistent with the methods used by dentists when providing services for complete dental restoration with composite materials.
Recent laboratory studies have proven that with the use of modern adhesive materials, it is possible to restore the reliability of the connection of the broken area of the tooth, corresponding to the intact tooth.
To increase the aesthetic appeal of the tooth being restored, it is recommended to first create a bevel of small width from composites around the entire perimeter of the broken area, reaching 1-2 mm depending on the specific situation.
Forecasting
After recovery, the patient is required to visit the dentist 2 and 12 months after the procedure. In cases where tooth sensitivity remains within normal limits, there is no need for further observations. The risks of complications due to the pulp are minimal.
Crown fractures, methods of their treatment
Incomplete crown fracture
An incomplete crown fracture (fracture) is a tooth crack that appears as a result of acute (dislocation, bruise) and chronic (abnormal bite, bad habits) traumatic injuries, while the integrity of the tooth is not compromised. The cracks look like lines that run randomly across the enamel; they can appear on teeth located next to a tooth that has undergone more severe traumatic effects.
During a normal inspection, cracks may not be visible; they are detected using transillumination. Transillumination is an examination method that involves shining a cold light beam through the injured tooth. Transillumination lighting is used not only to detect cracks, but also to identify contact caries, subgingival dental plaque, and pulpitis.
When a patient with an incomplete crown fracture seeks help, an electroodontodiagnosis (EDD) is performed to monitor the condition of the pulp after injury.
Typically, cracks do not penetrate deeper than the enamel-dentin border of the tooth, and therefore do not cause complaints in patients, except for minor sensitivity to temperature and chemical stimuli, which sometimes occurs when eating. Over time, the enamel at the site of damage darkens, caries develops, and the tooth may split along the crack.
Causes of fractures
Tooth fractures occur when:
- a strong blow to the tooth during a game, a fall, an accident, or doing any work;
- contact of solid food with a tooth with a carious cavity or with a previously treated tooth with large fillings;
- presence of bad habits (crunching nuts in shells, opening beer bottles with teeth);
- abnormal bite;
- hitting the antagonist tooth with dental forceps when removing a tooth on the opposite jaw.
A tooth fracture can occur in any part of the tooth; In direction, fractures are longitudinal, oblique and transverse.
Enamel fracture (chip)
When the enamel is fractured, its surface layer usually breaks off. Patients do not complain of pain, they are concerned about cosmetic defects. Chipping most often occurs at the corner of the tooth; the sharp edges of the chip injure the mucous membranes of the oral cavity.
X-ray examination does not reveal any changes in the dental tissue; transillumination examination can reveal enamel cracks at the edges of the chip. When a chip is combined with a tooth bruise, pulp death is possible.
Treatment for an enamel fracture involves grinding off the sharp edges and applying fluoride varnish to the fracture plane to protect the tooth from caries. Chips are restored using artistic restoration - extension is carried out with composite materials. If the pulp dies, it must be removed followed by filling the root canals.
Possible complications
A fracture of a baby tooth in a child usually does not lead to complications, as it is accompanied by the removal of a temporary tooth and subsequent observation.
In adults, trauma to a permanent tooth can lead to its loss and a long recovery process. Delayed contact with the dentist leads to:
- To an abscess of the maxillofacial area.
- The formation of phlegmon is a purulent-necrotic inflammation that can lead to sepsis or meningitis.
- Tooth loosening and loss.
- Acute pulpitis.
- Pulp atrophy, that is, its replacement with connective tissue.
- Inflammation of the periosteum (periostitis).
Long-term consequences of injury include root resorption, that is, resorption of the bone tissue surrounding the tooth. This phenomenon is normally observed in children when changing baby teeth.
If, after a minor injury, a person does not go to the dentist, then it should be taken into account that the integrity of the tooth may be compromised. A crack or break is not always noticeable outwardly, and the painful syndrome is mild. In this case, the tooth may not withstand normal chewing load. This can lead to a complete fracture.
Diagnostics
Examination of the patient first reveals a tooth dislocation, a root fracture is confirmed later by X-ray examination; It is recommended to perform a 3D computed tomography, since a regular x-ray may not detect a fracture. In addition to determining the area and direction of the fracture, the study makes it possible to determine the condition of the walls of the alveoli, periodontium, and the position of displaced fragments.
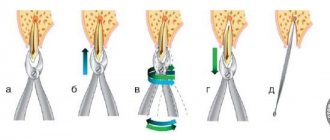
The dentist is also able to determine a root fracture using the following technique: with his right hand he slightly moves the crown of the tooth back and forth, while the finger of his left hand located on the vestibular surface (oriented towards the vestibule of the mouth) of the alveolar part of the jaw will feel the movement of part of the broken root associated with crown This method is not suitable if the fracture occurred in the apical part of the root, so an x-ray examination is required.
What to do if a tooth is dislocated
If an injury occurs, it is necessary to provide assistance to the victim and take him to a doctor for dental diagnosis and treatment.
First aid scheme:
- Examine the oral cavity. If a segment falls out, wrap it in a damp, clean cloth and put it in a bag. If there is a bleeding hole: apply a clean gauze pad to it. The victim's mouth must be closed for 30 minutes. After half an hour, the gauze can be removed. In case of a depressed injury, tamponade cannot be performed.
- Apply ice to the sore area of the cheek.
- Take the person to the dentist.
After clarifying the circumstances of the incident, the doctor will examine the oral cavity and determine the nature and type of injury. To study the details and assess the general condition of the jaw, X-ray diagnostics (orthopantomography) is prescribed. Sometimes a CT scan and EDI may be required (to monitor the pulp).