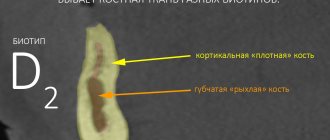
The quality of dental implantation and subsequent prosthetics depends on various factors. Before choosing implants, the doctor conducts an examination. Its obligatory stage is the determination of bone density. Depending on this parameter, the implantologist determines the possibility of installing an artificial root, its length, puncture method, etc.
Bone characteristics also influence the initial stabilization of the implant, the period required for complete healing. For successful implantation, the quantity, quality, biotype of bone tissue, its structure, and the structure of the jaws are important. The doctor studies all these parameters during the preliminary examination.
Bone Density Measurement
Bone density is determined by different methods:
- Echoosteometry. Diagnostics is based on the characteristics of the passage of ultrasound through bone tissue. The doctor evaluates the speed of passage and calculates the density. The peculiarity of this method is that to evaluate the characteristics, a straight section of at least 4 cm is needed, so it is used only on the lower jaw.
- Radiography. Used on the upper jaw, where it is impossible to use more precise ultrasound methods. The disadvantage of its use is inaccurate results.
There are situations where it is impossible to accurately determine bone density. The doctor is guided by low-reliability data, and only during bone preparation does he realize that its density is not enough. An experienced doctor can successfully place an implant in loose bone. To do this, you can make a bed of smaller diameter and condense the bone. This helps ensure primary stability, and taking calcium supplements during the rehabilitation period helps ensure good survival.
Cone beam diagnostics: anatomical landmarks in dental implantation
Cone beam computed tomography (CBCT), also known as a method of computer visualization of volumetric images, is a valuable diagnostic tool for verifying the structural features of anatomical objects, diagnosing pathologies of the oral cavity, assessing the height and width of the alveolar process, as well as treatment planning in cases of dental implantation .
Many authors have drawn attention to the fact that the informed agreement alone, which the patient signs when familiarizing himself with the potential risks of the dental implantation procedure, often cannot provide adequate legal protection for either the doctor or the patient in cases of lawsuits. For example, Curley and Hatcher, considering an example of iatrogenic penetration into the area of the mandibular canal during implantation (and the resulting occurrence of parasthesia), warn that if the patient did not undergo a preoperative tomographic examination, which could help avoid such consequences, then legal problems associated with the insufficiency of a written agreement as a legal document become more acute, gaining a conflict nature. On the other hand, the need for CBCT is determined by the decision of the attending physician, which depends on many factors. One of these factors is the need to obtain additional objective information to assess the parameters of intraoral and facial structures. Thus, it is logical that the very understanding of the capabilities of CBCT scanning is one of the key factors in effective treatment, because this type of diagnosis ensures the simultaneous receipt of various projections of the anatomical area of interest (from panoramic to cross-sectional and axial), and the ability to manipulate the resulting graphic reconstruction further expands the horizons of adequate preoperative planning for future intervention.
The American Academy of Oral and Maxillofacial Radiology has developed a series of recommendations regarding which tomographic image slice shapes are most appropriate for analysis during the planning phase of a dental implant procedure. The recommended sectional reformats greatly facilitate the process of verifying the parameters of the bucco-lingual width and height of the alveolar ridge of the upper and lower jaws, and also help determine the areas of bone undercuts and the position of individual structures (for example, the lower alveolar nerve), which determine the fundamental possibility of installing a dental implant.
This article is a kind of foundation for a detailed study and interpretation of CBCT images. The reader will also be able to familiarize themselves with the advantages of some panoramic images, which provide a fairly large amount of information about a particular anatomical segment, and how this type of planimetric images can be effectively combined with volumetric reconstructions at the planning stages of iatrogenic intervention. A description of some structural elements of the upper and lower jaws is carried out taking into account their clinical significance and the possibility of implementing the acquired knowledge in the practice of a dentist.
Clinical and radiographic studies
When studying CBCT scans, the doctor must analyze each tomographic section in detail for the presence of hidden pathological changes. It is recommended, although not required, to begin analyzing the 3D reconstruction on the left side of the image (which corresponds to the patient's right side) and work forward by examining slice by slice (also called layers or cross-sections). Slice thickness is typically 1 mm, but may vary depending on the software used. On the periphery of each section there are horizontal and vertical millimeter markings that help to measure parameters of different anatomical structures. In addition, other graphical software tools can be used to carry out similar measurements. The use of radiopaque markers (for example, barium sulfate) at the time of scanning greatly facilitates taking measurements in certain areas of the jaws. But we should not forget about the need for a thorough clinical examination, complementing X-ray diagnostics: palpating the intervention area and manual assessment of the ridge parameters in edentulous areas.
Structures of the mandible: foramen and lingula
One of the first anatomical structures visible on CT images of the mandible is the mandibular foramen (mandibular foramen), the area where the trunk of the inferior alveolar nerve enters the ramus structure of the mandible (Figure 1). When performing mandibular anesthesia, it is recommended to insert the injection needle 6-10 mm above the occlusal plane, since the entrance to the mandibular canal is located more coronally in 2-25% of cases. Therefore, when anesthesia is performed at the level of the occlusal plane, its result may not always be quite effective. Above the mandibular foramen there is a bony tongue, and adjacent to this area the sphenomandibular ligaments are attached (Figure 1).
Photo 1. Mandibular foramen and lingula of the lower jaw: A) the nerve trunk enters the body of the jaw through the mandibular foramen; B) the tongue is part of the bone crest, overlapping the mandibular foramen, to which the sphenomandibular ligament is attached.
Inferior alveolar canal
Moving forward from the ramus of the jaw on the CT image, you can notice that the inferior alveolar nerve (IAN) (photo 2) can occupy a variable position relative to the body of the mandible. On average, the width of the canal is 3.2 mm, and its space is surrounded by cortical bone, which, however, does not provide reliable safety for the nervous structure when preparing the bone bed. In order to determine the optimal implant length in a particular area of the mandible, it is advisable to measure the length from the top of the alveolar ridge to the most coronal part of the canal, and then subtract another 2 mm from the result obtained to ensure the safety of a future implantation procedure.
Photo 2. Panoramic reformat: the course of the inferior alveolar nerve. As a rule, the third branch of the trigeminal nerve (mandibular nerve) gradually descends along the body of the mandible, but sometimes it can change the level of its position quite abruptly.
Submandibular fossa and mylohyoid ridge
The submandibular fossa is an undercut at the back of the mandible and contains the submandibular salivary gland (Figure 3). The latter is topographically located under the mylohyoid muscle. This area of the jaw must be palpated before implantological manipulation in order to determine possible bone undercuts in the molar area. Parnia et al reported that 52% of patients had submandibular fossa depressions 2–3 mm in depth, and 28% were found to have a submandibular fossa depth greater than 3 mm. Thus, in cases of extensive bony undercuts, the preparation of the bone bed should be carried out with greater care to avoid iatrogenic trauma to the tissues of the floor of the mouth, damage to blood vessels and the occurrence of bleeding. The ridge on the lingual side of the mandible, shown in photo 3, is nothing more than the mylohyoid ridge, to which the mylohyoid muscle of the floor of the mouth is attached.
Photo 3. Submandibular fossa and mylohyoid ridge: A) in the area of the submandibular fossa there is a submandibular salivary gland; B) the mylohyoid ridge is the site of attachment of the mylohyoid muscle.
mental hole
In the area of the first molar or second premolar, the NAS usually divides into two branches: the mental and incisive nerves. The mental foramen is an anatomical formation through which the mental nerve exits its canal. When analyzing CT slices, the mental nerve canal is visualized as a separate, well-contoured area of lucency that passes through the buccal cortex of the mandible (Figure 4). An important aspect is to understand the fact of the branch of the incisive nerve: unintentional iatrogenic injury to the latter cannot provoke parasthesia, but, at the same time, damage to the NAS or mental nerve often results in a violation of nerve sensitivity. It is extremely important to analyze the CT slices anterior to the mental foramen in detail, since the nerve fiber branch may form an anatomical loop that extends slightly anterior to the usual exit of the mental nerve. Often, such a loop is formed when the NAS goes down and anteriorly to the mental foramen, and after exiting it returns back into the lumen of the canal. This may appear on the image as two separate canals, or as a “C” shape of the anatomical structure (Figure 5). In the absence of the anterior loop of the mental nerve, located mesial to the mental foramen, traces of secondary X-ray clearings are usually not observed in the bone structure (photo 6). At the same time, in the absence of a mental nerve loop, favorable conditions are formed for installing a longer implant, since signs of paresthesia are usually not observed when the incisive nerve is damaged.
Photo 4. Chin hole. Three branches of nerve fibers emerge from the foramen area at once, but the radiolucent area of the mental foramen is the main landmark when analyzing CBCT images.
Photo 5. Frontal loop of the inferior alveolar nerve in the area of the mental foramen in the shape of the letter “C”. There should be at least a 2 mm safe zone above the loop area during implantation.
Figure 6. CBCT images of the normal area of the mental foramen without signs of a nerve trunk loop in the frontal region.
Marrow space
The medullary space (Figure 7) can be found within the cancellous bone structure in the form of an anatomical region ranging from 200 to 2000 µm in width. Radiologically, the space is represented by a hollow formation, which cannot provide any resistance to the instrument during the preparation of the bone bed. When performing an osteotomy on the lower jaw over the area of the nerve trunk, it is necessary to use preparation stoppers, which will help avoid unplanned penetration into the medullary space.
Photo 7. Marrow space in the structure of cancellous bone.
Alveolar ridge outline
The contour of the alveolar ridge is a critical parameter when choosing the width of the implant for installation in this area of the jaw. For the residual ridge shown in photo 8, several treatment options can be used at once. For example, when forming bone dislocations on the buccal or lingual sides of the alveolar ridge during preparation of the bone bed, special membranes filled with bone substitute can be used. In cases where the height of the ridge is sufficient, its vertical parameter can be reduced to achieve a level of suitable width. The principles of guided bone regeneration and mandibular clefting can also be used to create an adequate bone contour. It should be noted that in some cases, the alveolar ridge may clinically appear thinner than it actually is, which is subsequently confirmed by the results of a CT scan, which objectifies the true parameters of the bony structures of the oral cavity (photo 8).
Photo 8. The narrow contour of the ridge does not limit the possibility of implantation without additional augmentation of the residual ridge to achieve the required bone width parameters.
Hourglass shaped mandible configuration
The hourglass shape of the alveolar ridge is an unusual variation in mandibular architecture that results from bony narrowing at the alveolar-basal junction. The prevalence of this jaw type can be found in approximately 3.9% of cases (Figure 9). Despite the reason for this anatomical configuration (a genetically determined shape or a structure formed as a result of age-related development), it significantly complicates the dental implantation procedure. In such cases, it is possible to perform bone grafting to restore the shape of the alveolar ridge before installing an implant, or to reduce the residual bone structure to achieve the necessary parameters under appropriate concomitant treatment conditions. It is easier, of course, to select other adjacent areas for implantation, bypassing the problem area.
Photo 9. Hourglass shape of the lower jaw: the problem area needs either reconstruction, or a different topographic area must be selected for implantation.
Lingual opening
In the area of the lingual foramen, the hypoglossal artery of the floor of the mouth anastomoses with the buccal blood trunk (photo 10). If the integrity of these structures is damaged during osteotomy, the amount of bleeding will be significantly greater than usual, but the use of guide pins helps to avoid such complications.
Photo 10. The lingual foramen is the area where blood vessels penetrate from the floor of the mouth into the structure of the lower jaw.
Cortical and cancellous bone types
It is important to ensure that there is sufficient volume of cancellous bone between the buccal and lingual cortices, since when the ridge is split, the volume deficit is replaced by cancellous bone tissue, while the cortical part has much less regenerative potential (photo 11).
Photo 11. Cortical and cancellous bone: Before performing a jaw splitting procedure, it is necessary to ensure that there is sufficient presence of cancellous bone, which plays an important role in the regeneration process.
Upper and lower mental tuberosities
The mental tuberosities are small bony prominences located on the lingual side of the lower jaw (photo 12). They are located on either side of the midline and are the area of attachment for the genioglossus (attached to the superior tuberosity) and geniohyoid muscles (attached to the inferior tuberosity). When separating flaps in case of providing surgical access, the genioglossus muscles should not be completely retracted from the area of the mental tuberosities, since in this case the tongue will retract in the posterior direction, which provokes blockage of the upper respiratory tract. In cases of mass resorption of the mandible, the mental tubercle can be found near the apex of the alveolar ridge, thus representing the so-called lingual eminence.
Photo 12. Upper and lower mental tuberosities: the genioglossus muscles are attached to the upper ones, and the geniohyoid muscles are attached to the lower ones.
Maxillary structures
Maxillary tubercle
The maxillary cusp (Figure 13) is a rounded structure on the distal surface of the bone body located behind the root region of the third molar. This area of bone tissue can be used as a site for bone graft harvesting for further use in bone crest reconstruction.
Photo 13. Maxillary tubercle: sometimes used for autograft harvesting.
Maxillary sinuses
The maxillary sinuses are the largest paranasal sinuses (photo 14). The maxillary sinus has the shape of a pyramid with a height of 36 mm to 45 mm and is lined with Schneiderian membrane. The thickness of the mucous membrane of the sinuses may increase in cases of smoking and other pathological conditions (photo 15). A lateral sinus lift is performed by creating a bone window on the buccal side of the jaw, then lifting the Schneiderian membrane and installing a bone graft in the lower third of the sinus.
Photo 14. Maxillary sinus: A) buccal wall; B) medial wall; B) zygomatic arch.
Photo 15. Maxillary sinus: thickening of the Schneiderian membrane.
The space of the maxillary sinus is limited by six walls:
- anterior (photo 16), containing the infraorbital nerve and blood vessels of the anterior teeth;
- the top (photo 16), which simultaneously represents the bottom of the orbit;
- posterior (photo 16), located in the pterygomaxillary region and separating the sinus cavity from the pterygopalatine fossa.
- medial, separating the sinus from the nasal fossa.
- lower (photo 16), passing along the area of the roots of the upper molars. If CT images reveal fenestration of the maxillary sinus floor (Figure 17), the flap is carefully removed to the ridge area, and the tissue protruding into the fenestration area is positioned back into the sinus. Otherwise, when Schneider's mucosa is lifted inward, the risk of its rupture in this area increases. Also, pseudocysts can often be found in the area of the sinus floor (Figure 18);
- lateral, providing access to the sinus during sinus lifting. The presence of a small area of radiolucency in the area of the buccal wall indicates the presence of a blood vessel (photo 19), and in case of an unsuccessful sinus lift procedure, CBCT may reveal fenestration of bone tissue in this anatomical area (photo 20). To achieve an effective result of sinus lifting, during the manipulation it is necessary to form a split flap, the connective tissue part of which must be positioned inside the sinus, thus ensuring its attachment to the newly formed Schneiderian membrane. Figure 21 shows the result of a completed sinus lift where the bone graft material did not reach the level of the medial sinus wall.
Photo 16. Maxillary sinus (panoramic reformat): four of the six walls are visualized in the image - A - the upper wall; P – posterior wall; SF – sinus floor; S – top wall.
Photo 17. Maxillary sinus: A) fenestration of the sinus bottom; B) thickening of Schneiderian membrane.
Photo 18. Maxillary sinus: pseudocyst in the area of the sinus.
Photo 19. Maxillary sinus: A) vessels in the structure of the buccal wall (radiopaque line); B) septum (septum) on the wall of the sinus. The septum can be verified on any wall of the sinus; as a rule, it divides the sinus into several sections. In this case, the septum is directed from the area of the medial wall to the buccal wall of the sinus. To fully diagnose the septum, it is imperative to analyze additional axial and panoramic reformats.
Photo 20. Maxillary sinus: fenestration in the area of the buccal wall.
Photo 21. Maxillary sinus: sinus elevator in the area of the lateral wall.
Anastomosis
The anastomosis is the anatomical junction of the maxillary sinus and the middle meatus (Figure 22), which is located in the upper part of the medial wall of the maxillary sinus above the first molar. The distance from the bottom of the sinus to the anastomosis is on average 28.5 mm, while the size of the latter is from 2 mm to 3 mm. Therefore, in cases where bone graft particles enter the sinus space after sinus lifting, they are removed from the sinus cavity through the anastomosis into the nasal space by the movement of the ciliated epithelium.
Photo 22. Anastomosis between the maxillary sinus and the middle meatus.
Partitions
The septa are bony structures in the sinus space that divide it into several segments (Figure 19). In 31% of cases, the septa are located in the premolar area, and, as a rule, do not completely divide the sinus space into independent single compartments. Most often they are found near the medial wall of the sinus, but when they are found in the area of the surgical field (the formed bony window of the lateral wall), the potential risk of rupture of the Schneiderian membrane during sinus lift increases.
Zygomatic arch
The zygomatic arch, or simply the cheekbone, consists of the zygomatic process of the temporal bone and the temporal process of the zygomatic bone (photo 14). In some cases, when performing planimetric radiography, the zygomatic arch is superimposed on the area of the maxillary sinus, and, thus, complicates the process of adequate diagnosis.
Nasopalatine canal
The nasopalatine canal is located more lingually between the central upper incisors (if they are present, of course), and the nasopalatine foramen in some sources is also called the incisive (cutting) (photo 23). When separating the flap in the area of the nasopalatine foramen, you can notice two separate lateral canals, which are called cutting canals. The anterior branches of the descending palatine vessels and individual branches of the nasopalatine nerve pass through them. Sometimes a dilemma arises about the possibility of installing an implant precisely in the area of these canals, especially in cases with acute resorption of the incisive premaxillary bone. The width of the nasopalatine foramen is approximately 4.6 mm and the length ranges from 8 mm to 12 mm, with the distance from the labial surface of the unresorbed ridge to the nasopalatine foramen averaging about 7.4 mm.
Photo 23. The nasopalatine canal is located lingual to the upper central incisors and contains the nasopalatine nerve and corresponding vessels.
Turbinate
The nasal cavity contains the inferior, middle, and superior turbinates (photo 24). The inferior turbinate is an independent, separate facial bone, while the middle and superior turbinates are parts of the ethmoid bone. In cases of inflammation, the mucous membrane of the shells swells and loosens, increasing in volume.
Photo 24. Nasal turbinates: A) inferior; B) average; B) top.
conclusions
CBCT scanning is a valuable diagnostic tool during dental implant procedure planning, providing much greater accuracy than panoramic or periapical x-rays. Sonick and colleagues, having analyzed the average radiographic linear distortions of each of the above diagnostic methods, found that with periapical radiographs the image deformation is about 14%, with panoramic images - 23%, and in cases of CT slices - no more than 1.8%. CBCT examination provides a valuable amount of diagnostic information with minimal radiation exposure, and the ability to obtain sections in different planes objectifies the parameters of the bone structures of the studied areas. This article demonstrated the main relationship between the diagnostic value of CT slices and the importance of identifying and verifying individual anatomical landmarks, knowledge of which greatly simplifies the process of planning future treatment. Correct interpretation and analysis of CBCT reformats allows not only to achieve the most predictable and effective results of dental implantation, but also to avoid a number of possible consequences and complications both at the time of manipulation and in the postoperative period.
Authors: Gary Greenstein, DDS, MS; Joseph R. Carpentieri, DDS; John Cavallaro, D.D.S.
How to determine bone thickness
When the bone is not thick enough, an implant cannot be installed. In this case, the implantologist may recommend undergoing an osteoplasty procedure first. The parameter is determined using computed tomography. This method allows you to accurately determine the thickness of even thin bones. This avoids the risk of installing an implant into bone tissue that is not able to cope with the load.
What is maxilla?
The maxilla is the name given to the upper jaw, the largest bone of the skull, which is paired: the right and left maxilla, respectively. The position of the entire upper jaw depends on them. The main function of the maxillae is to protect the contents of the skull from external influences. They can be compared to the front part of a motorcycle helmet, the purpose of which is to protect the head from injury. The maxillae prevent damage to the skull as a result of impacts from the front or side.
The influence of the structure of the maxillae on facial aesthetics
The attractiveness of the face largely depends on the shape of the upper jaw. One part of it is connected to the eye sockets, and the second is deeply “recessed” into the skull. The location of such important elements as the eyes, nose, upper teeth, palate and even the lower jaw directly depends on the location of the maxillae, their size and shape.
Many people make attempts to improve the aesthetics of their faces by choosing a teeth straightening method. If a person clearly understands the importance of maxillae, he will understand that wearing braces to correct the bite is a bad idea. The reason for the curvature of the nasal septum, differences in eye size, and incorrect position of the teeth relative to each other when the jaws are closed (bite) is the displacement of the maxillae. The presented photographs clearly demonstrate how much the maxillae influence the position of the nose, eyes and cheekbones.
Since the maxillae touch the lower border of the orbits, they support the eyeball, provided that they are extended in a horizontal position and at the same time raised. For the reason stated above, the eyes look more attractive and seem more alive. At the same time, folds and wrinkles do not appear on the skin under the eyes. If the maxillae are extended downward and flat, then the appearance of the eyes changes for the worse: they look tired, set deep in the skull. The horizontally retracted maxilla prevents the protrusion of the lower jaw. For this reason, the problem of crowding of teeth arises, and the chin begins to sag, looking extremely unattractive, as can be seen in the presented photos.
People's faces look beautiful if the maxillae are pushed up and forward. The last feature determines the aesthetics of a smile. Many people believe that a wide smile is an attractive feature. Look at the faces of famous actors in the picture. They have very charming smiles! All these movie stars have raised maxillae, which reduces the distance between the nose and upper lip and increases the height of the cheekbones. Faces developed forward look voluminous.
The faces of some people who decide to undergo plastic surgery do not look the way they expected: their lips are overstretched. The skin, as well as the muscles of the face, cover the bones of the skull like a canvas frame. If such a “frame” is flat, that is, the maxillae are extended downward, no actions of the plastic surgeon will lead to the desired result. Faces look really beautiful if the maxillae are three-dimensional.
In the profiles of girls on most social networks you can find selfie photos in which they pose with duck lips. Often such pictures look ridiculous, but the only reason for choosing such a facial expression is an attempt to imitate beautiful models whose maxillae are developed horizontally and pushed forward.
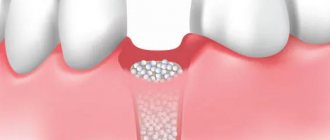
How to determine bone width
Using computed tomography, another important parameter for implantation is studied - bone width. For normal implant survival, it is necessary that the width of the surrounding bone tissue be 6-7 mm. If the width is insufficient, implantation is impossible. In this case, the doctor will recommend osteoplasty or another type of prosthetics.
The influence of soft tissues, in particular the tongue, on the development of maxillae
To demonstrate the influence of soft tissue on facial attractiveness, Dr. Mike Mew uses photographs of his beautiful wife. In the photo, important elements are indicated in different colors, while the part of the maxilla that determines external beauty to the greatest extent is painted in blue. Blue and red colors are used to represent the inner and lateral parts of the cheekbones, respectively. The maxilla is under the influence of several muscles at once. For example, the masticatory muscle is affected from the side. But what determines the position of the inner part of the maxilla? Oddly enough, but language influences this! More precisely, his position.
The tongue is one of the main muscles, the strength of which determines the development of the upper jaw. The position of the tongue also matters. If it is located on the upper palate, and its tip rests on the palatine tubercle (the area immediately in front of the front teeth), then under its influence the maxillae develop upward and forward. The opposite situation is observed if the muscles of the tongue are weak and the tongue itself is poorly developed. The tongue, which constantly puts pressure on the palate, contributes to the development of an attractive face, which is characterized by a large width of the upper jaw, regular placement of teeth, height of the cheekbones and attractive shape of the eyes. The force with which a properly positioned tongue constantly presses on the palate prevents the development of a downward-looking face.
Causes and features of the development of facial dystrophy
This is a common problem that occurs due to various reasons: cesarean section, birth trauma, malposition of the fetus. But most often, facial dystrophy begins to develop in childhood and adolescence. Above are photographs of the boy taken at different ages. In the first picture (ten years of age), the face has horizontally developed wide maxillae. The remaining two photographs, taken at the age of 17, show compacted and elongated maxillae, and a retracted lower jaw. What caused these changes?
The peculiarities of the position of the tongue and the swallowing process, which are laid down in infancy, have a significant influence on the development of the maxillae. Breastfeeding plays a key role. The first unconditioned reflex developed at the beginning of life is sucking. The process of sucking milk from the breast requires quite complex manipulations of the elements of the oral apparatus. The further position of the tongue, the development of the correct type of swallowing, in which the tip of the tongue rests on the area behind the front teeth of the upper jaw, depends on it. This process involves the deep muscles of the tongue, as well as the entire front of the neck. This type of swallowing can only develop as a result of breastfeeding.
Another important feature of the process of sucking milk from the breast is its influence on the development of the correct functioning of the sphincters of the human body. When performing sucking movements, you can notice how the perineal sphincter begins to function. From this we can conclude that breastfeeding affects not only the correct development of the oral apparatus, but also is the basis for the future physical and psychosexual characteristics of a person. This is why many doctors recommend breastfeeding unless there are any contraindications for the baby. Bottle feeding, thumb sucking or pacifier sucking are the main causes of tongue misalignment.
If an older child prefers soft foods, the development of incorrect tongue position continues. According to the founder of orthotropics, John Mew, and who continued the work of his father, Mike Mew, facial dystrophy is caused by environmental influences and does not have a genetic predisposition. Photographs of our ancestors can serve as evidence of these judgments. The shape and structure of the faces depicted on them confirm the influence of breastfeeding and nutritional habits on the condition of soft tissues and the development of maxillae. In the past, people ate solid foods more often, and the mothers of our ancestors always breastfed their babies.
When viewing photographs from a hundred years ago, which depict Cossacks, Permians, Siberian hunters and representatives of other subethnic groups, one can easily notice that the faces of almost all of them are horizontally developed. With a few exceptions, they have high cheekbones and a protruding upper jaw.
Modern man lives in different conditions than 100 or more years ago. We are used to eating mostly soft foods, which has a bad effect on the development of the muscles and bones of the skull. Researchers, including the founders and followers of orthotropics, have noticed a trend in the lengthening of the skull. The found remains can only suggest (simulate on a computer) what the faces of distant ancestors were like. But even photographs taken a hundred years ago make it possible to notice significant differences between the faces of people who lived in the 19th and 20th centuries and the faces of modern people. The latter are increasingly experiencing a deviation called facial dystrophy, since our living environment has undergone serious changes associated with the rapid development of science. This has a bad effect on natural bodily beauty, including facial attractiveness.