{jcomments on}Treatment of victims with jaw fractures consists of repositioning and immobilization of jaw fragments, as well as drug treatment and physical therapy. Reposition involves aligning or moving facial bone fragments into the correct position. If it is not possible to compare the displaced fragments at once, they are reduced gradually, over several days, using elastic traction. Immobilization means securing the fragments in the correct position for the period necessary for their fusion (consolidation), i.e. until callus formation. On average, this period is 4-5 weeks for uncomplicated healing of a fracture of the upper jaw and a unilateral fracture of the lower jaw. With a bilateral fracture of the lower jaw, the immobilization period can increase to 5-6 weeks. Drug and physical treatment are necessary to prevent the development of complications during the period of consolidation of fragments (antibacterial, anti-inflammatory, antihistamines; medications that improve the rheological properties of blood and tissue microcirculation, immunostimulants, drugs that optimize osteogenesis). In addition, the question of the advisability of preserving teeth in the fracture gap and the need for therapeutic measures in relation to these teeth must be resolved.
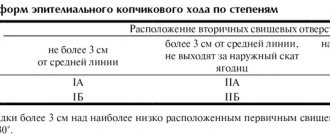
Types of conservative methods of immobilization of jaw fragments
There are temporary methods of immobilization (including transport) and permanent (therapeutic). Temporary methods for securing jaw fragments are divided into: - extraoral (bandage, chin sling, improvised bandages using improvised means); — intraoral (methods of intermaxillary ligature fastening, splints-spoons with “mustaches” of different designs). Permanent (therapeutic) methods of immobilization are divided into : - non-laboratory splints (individual dental splints made of metal or other material, standard dental splints); — laboratory-made splints (Weber’s supragingival splint, simple or with an inclined plane, Vankevich and Vankevich-Stepanova splints, various dental aligners, Port’s supragingival splint).
Temporary (transport) immobilization
Indications for imposing temporary (transport) immobilization: - lack of conditions for permanent (therapeutic) immobilization and the need to transport the victim to a specialized medical institution; — lack of specialized personnel who can carry out permanent immobilization; - lack of time required for permanent (therapeutic) immobilization. This usually happens during combat operations or other emergency situations (earthquake, accidents with a large number of casualties, etc.), when a large flow of victims and wounded with trauma is simultaneously observed; - severe general somatic condition (traumatic shock, coma, intracranial hematoma, etc.), which is a temporary relative contraindication for therapeutic immobilization. Temporary immobilization is imposed for a period of no more than 3-4 days (the maximum time required to transport victims to a specialized institution or call a specialist to the patient), since with its help it is impossible to achieve the required long-term immobility of fragments. In exceptional cases, this period is extended due to the severe general condition of the patient, in which therapeutic immobilization is temporarily contraindicated. Temporary immobilization can be performed both outside a medical institution and in a specialized clinic. If it is imposed while the victim is being transported to a medical facility, it is called “transport”. Typically, temporary immobilization is applied by junior or nursing staff, as well as in the form of self- or mutual assistance. Some methods are performed only by specialists (intermaxillary ligature fastening).
Extraoral methods of temporary (transport) immobilization.
— A simple bandage parietal-chin bandage . It is applied for fractures of the upper and lower jaw. A wide gauze bandage is used, circular tours of which are carried out through the chin and parietal bones. You can use improvised material: a headscarf, scarf, etc., which is less convenient. A simple bandage does not stay firmly on the head and must be adjusted frequently. — The parietal-chin bandage according to Hippocrates is securely fixed on the head and does not require correction. Used for fractures of the upper and lower jaw.
Parietomental bandage according to Hippocrates
— Standard soft chin sling by Pomerantseva-Urbanskaya. Used for fractures of the upper jaw and lower jaw. It consists of a chin sling, to which wide elastic bands are sewn on both sides, turning into fabric ribbons with holes for a lace. The sling is convenient and versatile, but is not used for fractures of toothless jaws and the absence of dentures.
Standard soft chin sling Pomerantseva-Urbanskaya
— Standard bandage for transport immobilization (rigid chin sling) for fractures of the lower and upper jaw. This bandage consists of a standard dimensionless cap and a rigid chin sling with slots and protrusions used to fix rubber rings and the victim’s tongue, as well as to drain wound contents. Intraoral methods of temporary (transport) immobilization.
Standard bandage for transport immobilization
— Standard transport splint for immobilization of the upper jaw . Consists of a standard cap and a standard metal spoon splint with extraoral rods (“whiskers”) firmly fixed to the spoon splint. — Intermaxillary ligature fastening . It is used most often in clinical practice. For immobilization, wire ligatures are used, which should be easy to bend, not oxidize and be inexpensive. Bronze-aluminum wire with a diameter of 0.5-0.6 mm meets this requirement. To apply an intermaxillary ligature fastening, take pieces of bronze-aluminum wire 7-10 cm long and tools (crampon forceps, Billroth-type hemostatic clamps, scissors for cutting metal wire, anatomical tweezers). Indications for the application of intermaxillary ligature fastening are to prevent displacement of fragments and eliminate intra-wound trauma during the transportation of the victim and during his examination, until the moment of therapeutic immobilization. General rules observed when applying intermaxillary ligature fastening: immobilization is carried out under local anesthesia, tartar is first removed, mobile teeth and teeth located in the fracture gap are not used for intermaxillary ligature fastening, stable antagonist teeth are used, wire ligatures are twisted clockwise. There are a large number of different methods of intermaxillary ligature fastening of jaw fragments.
Methods of intermaxillary ligature fastening.
— Silverman . A bronze-aluminum ligature is drawn around each of the two adjacent teeth and twisted, then the ends of these two ligatures are also twisted. The same is done in the area of antagonist teeth. The upper wire flagellum is twisted with the lower one, and the end is cut off. Advantages: ease of manufacture. Disadvantages: after twisting the ligatures, thick wire flagella are formed in the vestibule of the mouth, injuring the mucous membrane; if necessary, open the patient’s mouth and cut the thick wire flagella, which is quite difficult. After examining the oral cavity, the structure has to be redone.
— Intermaxillary ligature fastening using the Ivey method.
Intermaxillary ligature fastening using the Ivey method
It is most often used in clinical practice, usually in all cases of jaw fractures. In case of a fracture of the upper jaw, the intermaxillary ligature fastening is supplemented with the application of a chin sling to prevent its displacement downward when the lower jaw involuntarily drops. Advantages: simplicity and efficiency, the ability to quickly open the mouth if necessary, without compromising the integrity of the structure. Intermaxillary ligature fastening according to Kazanyan is less convenient compared to the Ivey method. The technique differs in that a figure-of-eight ligature is placed around the adjacent teeth of one fragment and its two ends are twisted in the vestibule of the mouth. The same manipulation is carried out on the antagonist teeth and on the teeth of the other fragment. The free ends are twisted and trimmed. Thus, the common end of the wire (flagellum) consists of four ends. The disadvantages of the method are the presence of a thick wire harness in the vestibule of the mouth, which can injure the mucous membrane, as well as the need to re-apply ligatures if they break or after emergency cutting of the ligatures.
— Intermaxillary ligature fastening according to Gotsko.
A polyamide thread is used as a ligature. It is passed around the neck of the tooth and tied with a knot on its vestibular surface. Next, both ends of the thread are passed through the interdental space of the antagonist teeth from the vestibule - into the oral cavity, then each end is taken out of the cavity into the vestibule of the mouth (distal and medial), pulled up and tied together with a knot, immobilizing. Advantage : low trauma, high efficiency.
Intermaxillary ligature fastening using the Gotsko method
Therapeutic (permanent) immobilization using non-laboratory dental splints
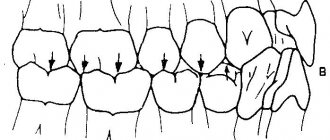
Individual dental wire splints by Tigerstedt. Types of Tigerstedt dental splints: - smooth splint-bracket; — bus-bracket with a spacer bend; - tire with hook loops.
The splints are made of aluminum wire d=1.8-2.0 mm and 12-15 cm long. They are tied to the teeth using bronze-aluminum wire d=0.5-0.6 mm. The splint is bent individually for each patient using crampon forceps. General rules for applying dental splints . 0.5 ml of a 0.1% atropine solution is injected subcutaneously to reduce salivation, splinting is carried out under local anesthesia, it is necessary to remove tartar to freely pass the ligature into the interdental space, bend the splint from the side of the fracture, try it on the teeth in the mouth, and bend it outside the oral cavity, the splint should be adjacent to the neck of each tooth at least at one point, the splint is tied to each tooth with a ligature wire, which is twisted clockwise. The production of the splint begins with bending a large hook that clasps the first tooth, or a hook spike inserted into the interdental space. To try on a splint, it is applied to the teeth in the mouth.
Smooth splint.
It is used to treat fractures of the lower jaw, provided that the larger fragment contains at least four, and the smaller fragment contains at least two stable teeth.
Smooth splint
Indications for use : linear fractures of the lower jaw, located within the dentition, without displacement or with easily reducible fragments, fractures of the alveolar process, fractures and dislocations of teeth, tooth mobility in acute odontogenic osteomyelitis and periodontitis, fractures of the upper jaw (Adams and Dingman methods), to prevent pathological fracture of the lower jaw. After treatment, before removing the splint, loosen the ligatures and check the lack of mobility of the fragments by rocking them. The splint is removed after 4-5 weeks. The patient needs to take liquid food. The doctor should regularly examine the patient 2-3 times a week. In this case, it is necessary to monitor the state of the bite, the strength of fixation of the fragments, the condition of the tissues and teeth in the fracture gap. When the fixation of the splint on the teeth becomes loose, it is necessary to tighten the ligatures by twisting them. If the ligature bursts, it is replaced with a new one. The patient is taught hygienic measures to prevent the development of gingivitis. For this purpose, the patient should brush his teeth and splint with toothpaste and a brush 2 times a day, after each meal, remove food debris with a toothpick, and rinse his mouth with antiseptic solutions 3-5 times a day.
Busbar with spacer bend.
The spacer bend prevents lateral displacement of fragments.
Busbar with spacer bend
Indications for use : fracture of the lower jaw within the dentition and the presence of a bone tissue defect of no more than 2-4 cm, fracture of the lower jaw without displacement or with easily reducible fragments, if the fracture gap passes through the alveolar part, devoid of teeth.
Tire with hook loops.
The splint is most often used to treat jaw fractures. Two splints with hooking loops are made for the teeth of the upper and lower jaw.
Tire with hook loops
Indications for use : fractures of the lower jaw outside the dentition, within the dentition - in the absence of four stable teeth on the larger fragment and two stable teeth on the smaller one, fractures of the lower jaw with difficult-to-reduce fragments requiring traction, bilateral, double and multiple fractures of the lower jaw, fracture of the upper jaw (with the obligatory use of a chin sling), simultaneous fractures of the upper and lower jaw. When making a splint, its hook loop should be at an angle of 45° relative to the gum. The towing loops are bent on the tire so that they are located in the area of the 6th, 4th and 2nd teeth. If the patient does not have these teeth, then hooking loops are made in the area of other teeth that have antagonists. Usually, 3-4 hook loops are bent on the splint adjacent to the teeth of the larger fragment, and 2-3 hook loops on the smaller one. The base of the loop must be within the crown of the tooth. If the displacement of the fragments is large and it is difficult to bend one splint onto both fragments, splints can be made and secured to each of the fragments. After their reposition, rubber rings are put on the hook loops at an angle so that they create compression of the fragments, which significantly prevents their movement. Periodically (2-3 times a week) the patient is examined, ligatures are tightened, rubber rings are changed, the vestibule of the mouth is treated with antiseptic solutions, and the condition of the bite is monitored. 10-25 days after applying the splint, an X-ray examination is performed to monitor the position of the fragments. After fusion of the fragments, before removing the splints, it is necessary to remove the rubber rings and allow the patient to walk for 1-2 days without fixation, eating soft food. If the fragments do not move, the splints are removed. If there is a slight change in the bite, the rubber traction is retained for another 10-15 days.
Splinting using the A.P. method Vikhrov and M.A. Slepchenko.
The authors proposed using a polyamide thread to strengthen the attachment of the splint to the teeth. To do this, take a bronze-aluminum wire ligature, fold it in the form of a hairpin and insert both of its ends into one interdental space from the mouth towards the vestibule of the mouth. The ligature is tightened so that a small loop is formed on the lingual surface of the interdental spaces. A similar procedure is performed in the area of all interdental spaces. Take a polyamide thread with a diameter of 1 mm and pass it through all the loops on the lingual side, the ends of the thread are brought out into the vestibule of the mouth behind the last teeth on both sides. Next, a previously made splint is placed on the teeth so that it is located between the two ends of the same previously made bronze-aluminum ligatures, which are then twisted. According to the authors, the advantages of their method are the following: stronger fastening of fragments, reduction of splint fastening time, and absence of trauma to the gum mucosa.
Splinting using the Vikhrov-Slepchenko method
Tooth standard splints.
Good manual skills are required to make custom wire splints. Their production requires a lot of time and frequent fitting to the dental arch. It is especially difficult to bend them in case of malocclusion, dental dystopia, etc. Taking into account the above, standard splints were proposed, which are manufactured in the factory, do not require bending of the hook loops and simplify splinting. In Russia, standard belt tires were proposed by V.S. Vasilyev. The tire is made of a thin flat metal strip 2.3 mm wide and 134 mm long, which has 14 hooking loops. The tire bends easily in the horizontal plane, but does not bend in the vertical plane. The Vasiliev splint is cut to the required size, bent along the dental arch so that it touches each tooth at least at one point, and tied to the teeth with ligature wire. The advantage of the splint is the speed of its application . The disadvantage is the impossibility of bending it in a vertical plane, which does not allow to avoid injury to the mucous membrane in the lateral parts of the jaws due to the discrepancy between the splint and the curve of Spee. This splint is not suitable for single-jaw splinting due to its low strength. Abroad, there are various designs of standard tires made of steel wire (Winter tires) and polyamide materials that can be bent in any plane. Tires are manufactured with pre-made hooks.
Comparative assessment of the effectiveness of three methods of gentle immobilization of the lower jaw for fractures
G. A. Khatskevich Doctor of Medical Sciences, Professor, Head of the Department of Pediatric Dentistry with a course of Maxillofacial Surgery at St. Petersburg State Medical University named after. acad. I. P. Pavlova (St. Petersburg)
V. G. Avetikyan Candidate of Medical Sciences, Associate Professor of the Department of Pediatric Dentistry with a course of Maxillofacial Surgery at St. Petersburg State Medical University named after. acad. I. P. Pavlova (St. Petersburg)
I. G. Trofimov Candidate of Medical Sciences, Associate Professor of the Department of Pediatric Dentistry with a course of Maxillofacial Surgery at St. Petersburg State Medical University named after. acad. I. P. Pavlova (St. Petersburg)
Zhang Fan , doctor, postgraduate student at the Department of Pediatric Dentistry with a course in Maxillofacial Surgery at St. Petersburg State Medical University named after. acad. I. P. Pavlova (St. Petersburg)
I. Yuan Ph.D., Lecturer at Shanghai University (Shanghai, China)
V. B. Nekrasova Doctor of Medical Sciences, Professor of St. Petersburg MAPO (St. Petersburg)
Patients with injuries of the maxillofacial area make up about 30% of all patients treated in hospitals for maxillofacial surgery, while fractures of the lower jaw make up about 70-85% of all fractures of the facial bones (Ivasenko P.I., Zhurko E. P., Chekin A.V., Konvay V.D. et al., 2007; Inkarbekov Zh.B., 2009; Bakardjiev A., Pechalova P., 2007).
An analysis of data published in the scientific literature showed that the frequency of complications of mandibular fractures reaches from 10 to 41% (Mubarkova L.N., 2008; Mirsaeva F.Z., Izosimov A.A., 2009), which does not allow us to talk about effectiveness existing treatment methods.
An important pathogenetic link in the development of inflammatory complications in fractures of the lower jaw is a violation of local immune defense, regional blood circulation and innervation in the fracture zone, deterioration of oral hygiene and impaired chewing function (Timofeev A. A., 2004; Berkhman M. V., Borisova I. V., 2007; Magomedgazhiev B. G., 2008; Inkarbekov Zh. B., 2009). Moreover, these changes can be provoked not only by the injury itself, but also by inadequate fixation methods. This especially applies to round aluminum or tape dental splints. Their application is extremely traumatic for the patient and dangerous for the surgeon due to the possibility of hand injury and infection.
In addition, dental splints, used for an average of 30 days, complicate oral hygiene and injure the periodontal border. This leads to the development of pronounced inflammatory changes in the periodontium. Fractures of the lower jaw occur quite often, in which there is no displacement of the fragments and mobility is low. In this case, the immobilization provided by dental splints turns out to be redundant. In this regard, the development of gentle immobilization methods is of particular relevance.
Material and research methods
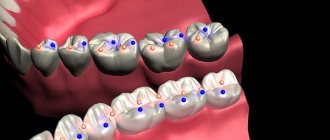
The work is based on the experience of treating 90 patients with fractures of the lower jaw. Of these, in 48 patients, the method of gentle immobilization—intermaxillary fixation using fixed orthodontic equipment—was used as the main and auxiliary (during osteosynthesis surgery) method of fixation (Fig. 1).
Rice. 1a. The stage of gluing Protekt dental buttons-braces. Immobilization of the lower jaw using elastic rings (the least traumatic method).
Rice. 1b. The stage of gluing Protekt dental buttons-braces. Immobilization of the lower jaw using elastic rings (the least traumatic method).
The comparison methods used were: immobilization of fragments with wrapping transmaxillary sutures - 18 patients (Fig. 2).
Rice. 2a. Immobilization of the lower jaw using two wire wrapped sutures.
Rice. 2b. Immobilization of the lower jaw using two wire wrapped sutures.
Intermaxillary suspension using orthodontic mini-implants - 24 patients (Fig. 3).
Rice. 3. Immobilization of the lower jaw using intraosseous implants of fixators and elastic rings.
The control group included 16 males (22.9 ± 1.2 years), practically healthy.
In the main group of patients, where Protekt braces and lingual buttons were used, biologically active additives (dietary supplements) "Lesmin" for oral administration and individual oral hygiene using dental Fitolon pastes.
For diagnosis and evaluation of results, clinical and radiological immunological, index-hygienic methods, electromyography and Doppler flowmetry were used to assess vascular microcirculation.
Indications for choosing the immobilization method using fixed orthodontic equipment (Protect) are as follows. The independent method of immobilization of the lower jaw, as an alternative to splinting, was used in the following cases: unilateral fractures without displacement or with slight displacement; bilateral fractures without displacement or with slight displacement; fracture of the condylar process without clinically detectable and functionally significant displacement (slight limitation of movements in the temporomandibular joint due to pain, the bite is not disturbed). In case of bilateral fractures of the lower jaw, in a number of cases where osteosynthesis was performed with titanium plates, bracket fixation was used as an additional method (Fig. 4).
Rice. 4. Bilateral fracture of the lower jaw. Immobilization was carried out using osteosynthesis and braces.
The analysis included only those cases where the method of gentle immobilization was used as the main method of fixation of fragments and the patients fully followed the recommendations for oral hygiene proposed by the authors. A total of 66 clinical cases were analyzed. Variants of fractures in percentage and their ratio are presented in Figure 5.
Rice. 5. Variants of mandibular fractures with gentle immobilization methods.
Research results
Patients of all 3 groups were observed from the start of treatment and for 3 months. The final assessment of treatment results was carried out 3 months after injury. Inflammatory complications were taken into account throughout the treatment. Consolidation of fragments occurred in all patients, regardless of the method of gentle immobilization. Malocclusion was detected in only one patient, whose jaw was immobilized using orthodontic mini-implants. In this case, it was possible to restore the bite by selective grinding of the teeth. The effectiveness of treatment with the methods under consideration was the same.
Inflammatory complications were observed with all methods of gentle immobilization, while in the case of using fixed orthodontic equipment (group 1), only one patient (4.2%) had a limited osteomyelitic process due to a tooth fracture left in the gap with pulp necrosis versus 12. 6% when fixed with mini-implants and 16.6% when fixed with wrapping transmaxillary sutures (Fig. 6).
Rice. 6. Frequency (%) of inflammatory complications with different methods of gentle immobilization.
In the second group (using mini-implants), 1 patient had a hematoma suppuration, and 2 patients had a limited osteomyelitic process. In the third group (wrapping transmaxillary sutures), 2 patients had suppuration of postoperative hematomas in the tissues of the floor of the mouth and one patient had chronic traumatic osteomyelitis. Thus, in the group of patients in whom gentle immobilization was performed using fixed orthodontic equipment, the number of inflammatory complications is minimal, which is due not only to less additional trauma during the procedure for immobilizing fragments, but also to the systemic use of dietary supplements.
Questionnaires to study self-assessment of quality of life were filled out by patients 1 month after the injury when the fixation structures were removed. A comparative analysis of the study results was carried out in samples of 12 patients from each group. A study of the “quality of life” profiles in patients using different methods of gentle immobilization showed that the quality of life decreases to a lesser extent in patients with fractures of the lower jaw when fixed using fixed orthodontic equipment and mini-implants (Fig. 7).
Rice. 7a. Comparative assessment of relatively healthy respondents’ QoL profiles with different methods of gentle immobilization. OTMS - wrapping transmaxillary sutures.
Rice. 7b. Comparative assessment of relatively healthy respondents’ QoL profiles with different methods of gentle immobilization. OMI - orthodontic mini-implants.
Rice. 7th century Comparative assessment of relatively healthy respondents’ QoL profiles with different methods of gentle immobilization. NOT - fixed orthodontic technique.
One month after the injury, self-assessment of the quality of life in patients with fractures of the lower jaw with a gentle method of immobilization using fixed orthodontic equipment on all scales of the physical component of health and one scale of the mental component (vitality) was higher than in patients with fixation using wrapping transmaxillary sutures.
When determining the level of oral hygiene, the Fedorov-Volodkina Hygiene Index (FHI) and the severity of periodontal inflammation according to the papillary-marginal-alveolar index (PMA) were recorded; at the initial examination, no statistically significant differences were found in patients of the three groups.
The highest RMA values were found in the group of patients where fixation of fragments was carried out using wrapping transmaxillary sutures - 43.3 ± 2.4%
Subsequently, when examined after 7 days, the level of oral hygiene worsened regardless of the method of gentle immobilization and was assessed in all groups as unsatisfactory. When examined a month later, a further increase in IGPV was observed in all groups, however, in the group using fixed orthodontic technology, the increase in IGPV was found to a lesser extent - 2.4 ± 0.03 versus 2.64 ± 0.07 points (p < 0.01) in the group where fixation was carried out using orthodontic mini-implants.
Compared to the initial values, an increase in inflammation during treatment was observed in all groups of patients. At the same time, the highest RMA values were established in the final study in the group of patients where the fixation of fragments was carried out using wrapping transmaxillary sutures - 43.3 ± 2.4%, and the lowest with the gentle method of immobilization we proposed using fixed orthodontic equipment - 26.4 ± 0.8% (Table No. 1).
Table No. 1. Comparative analysis of the dynamics of dental indices with gentle methods of immobilization of the lower jaw, used as the main ones.
| № | groups | n | IGFV (points) | RMA (%) | ||||
| 1 time | 2 times | 3 times | 1 time | 2 times | 3 times | |||
| 1 | NOT | 24 | 2,08±0,04 | 2,3 ±0,06 ** | 2,4±0,03 *** | 22,0±0,8 | 27,5 ±1,0 *** | 26,4±0,8 ** |
| 2 | OMI | 24 | 1,98±0,07 | 2,32±0,07 ** | 2,64±0,07 *** | 22,2±1,0 | 26,9±1,36 ** | 34,9±1,3 *** |
| 3 | OTMS | 18 | 2,17±0,04 | 2,35 ± 0,09 | 2,5±0,09 ** | 25,1±2,1 | 32,2±1,75 * | 43,3 ±2,4 *** |
| P1-2 | >0,05 | >0,05 | <0,01 | >0,05 | ||||
| P1-3 | >0,05 | >0,05 | >0,05 | >0,05 | ||||
Note: the differences relative to the initial examination are statistically significant: * - p<0.05; ** — p<0.01; *** — p<0.001; 1st time during the initial examination; 2nd time after 7 days (at discharge); 3rd time after 1 month. (when removing structures).
This result is associated with the use of surgical intervention in the comparison groups that stimulates the inflammatory response. Less severe inflammation in the final study could have been influenced by the use of the Lesmin dietary supplement by patients in the experimental group and the use of Fitolon toothpaste.
The study of factors of nonspecific protection and local immunity in the oral fluid of victims with fractures of the lower jaw during the initial examination revealed that in all groups there was a significant decrease in lysozyme activity compared to healthy individuals against the background of activation of mucosal immunity (increased levels of immunoglobulins) with a pronounced imbalance of pro- and anti-inflammatory cytokines (increased IL-8 and decreased IL-4). When examined a week later, a decrease in lysozyme activity relative to the initial data was found only in patients with entwined transmaxillary sutures (65.5 ± 2.1 versus 73.1 ± 2.3% at p < 0.01). In the same group, the lowest levels of lysozyme activity were found after a month (63.6 ± 2.2%), although upon admission in this group the activity of lysozyme was the highest (Fig. 8).
Rice. 8a. Dynamics of lysozyme and sIgA activity in patient groups. Note: NOT - 1st group, OMI - 2nd group, OTMS - 3rd group.
Rice. 8b. Dynamics of lysozyme and sIgA activity in patient groups. Note: NOT - 1st group, OMI - 2nd group, OTMS - 3rd group.
When examined after 7 days, in groups 1 and 2 the level of sIgA decreased slightly, and in group 3 it increased just as slightly. The final examination a month later showed a slight decrease (normalization) of sIgA in group 1, where we used the gentle immobilization method we proposed using fixed orthodontic equipment - 56.1 ± 3.8 versus 72.5 ± 5.78 μg/mg of protein ( p < 0.01) and 77.7 ± 11.4 μg/mg protein.
Studies have shown that when using fixed orthodontic equipment as the main method of fixation, inflammatory complications in the fracture zone are detected in 4.2% of cases
When examined after 7 days, IgG was still at high levels in all groups. Against this background, only in the experimental group of patients was there a decrease in IgM to the control level (from 2.3 ± 0.2 to 1.37 ± 0.1 μg/mg protein, with p < 0.001). A month later, a study confirmed the normalization of IgM levels only in the experimental group, where we used the gentle immobilization method we proposed using fixed orthodontic equipment (1.38 ± 0.1 versus 1.9 ± 0.13 and 2.49 ± 0.26 μg/ mg protein in comparison groups). Moreover, after a month in the experimental group, IgG decreased most significantly (3.77 ± 0.3 versus 4.6 ± 0.45 and 5.0 ± 0.4 μg/mg of protein in the comparison groups).
During the initial examination, the level of IL-8 was 9 times higher than that of the control group; in some patients it was more than 5000 pg/ml, and in some cases IL-4 was not detected at all. Against the background of such large-scale changes in the regulators of the immune response, the smallest were found in patients in the experimental group. Thus, after 7 days they showed a decrease in IL-8 (from 2707.9 ± 198.7 to 1916.3 ± 199.0 pg/ml, with p < 0.01), and when examined a month later, it was in this group has the lowest level of IL-8 (1488.2 ± 183.3 versus 1953.3 ± 202.1 and 2247.1 ± 304 pg/ml in the comparison groups) (Fig. 9).
Rice. 9. Dynamics of IL-8. Note: NOT - 1st group, OMI - 2nd group, OTMS - 3rd group.
The dynamics of IL-4 are less pronounced. In the experimental group, its amount practically does not change during treatment, remaining 2 times lower than in the control group, and in the comparison groups it further decreases. After a month, in patients of group 1, the level of IL-4 was 2.7 ± 0.2 versus 1.12 ± 0.4 and 1.0 ± 0.5 pg/ml in the comparison groups.
Thus, the study of the activity of lysozyme, mucosal immunity and the level of cytokines in the oral fluid showed that in response to a fracture of the lower jaw, the body responds with an acute-phase inflammation reaction, accompanied by a decrease in lysozyme activity against the background of activation of mucosal immunity and a pronounced imbalance of pro- and anti-inflammatory cytokines. When using the method of gentle immobilization developed by us against the background of systemic administration of the Lesmin dietary supplement, the normalization of disorders proceeds faster (in some cases, improvement occurs after 7 days), and when examined a month later, it is more pronounced, which is due to the less traumatic method of fixation and systemic administration of the biomodulator Dietary supplement "Lesmin"
conclusions
- As a support for mandibulo-maxillary fixation, it is proposed to use non-removable orthodontic equipment: dental braces and lingual buttons, which will eliminate surgical intervention, which complicates the course of the restoration process in periodontal tissues, and will simplify and increase the effectiveness of treatment for patients with mandibular fractures.
- When using fixed orthodontic equipment as the main method of fixation, inflammatory complications in the fracture zone were detected in 4.2% of cases. When using Fitolon toothpaste and Lesmin dietary supplement, better results were registered in comparison with the control. IGFV 2.4 + 0.03 versus 2.65 + 0.1 points at P < 0.05, and a decrease in the intensity of periodontal inflammation RMA 26.4 + 0.1 versus 36.8 + 2.0% at P < 0.001 .
- Our data confirm the regulatory effect of cytokines in the development of inflammation. The initial increase in IL-8, as a consequence of injury, is physiologically determined and stimulates the mucosal immune system, without having a negative effect on such a factor of nonspecific defense of the oral cavity as lysozyme. However, high values of IL-8 after a month negatively affect the restoration of lysozyme activity. At the same time, a decrease in the level of the anti-inflammatory cytokine IL-4, established at all stages of the study, is accompanied by an increase in lysozyme activity.
- Restoration of lysozyme activity against the background of a decrease in elevated immunoglobulins in the oral fluid and a decrease in the degree of imbalance between pro- and anti-inflammatory cytokines leads to a decrease in the inflammatory reaction in the periodontium and an improvement in the hygienic state of the oral cavity, which confirms the effectiveness of the use of Fitolon toothpaste and the systemic use of the Lesmin dietary supplement. in patients with fractures of the lower jaw against the background of a gentle immobilization method using fixed orthodontic equipment.
- A comparative analysis in three groups of patients with gentle immobilization showed that in the case of using fixed orthodontic equipment, the number of inflammatory complications is minimal, which is apparently due not only to less additional trauma during the procedure for immobilizing fragments, but also to the systemic use of dietary supplements. Moreover, a month after the start of treatment, these patients’ self-assessment of quality of life is higher than with other methods of gentle immobilization.
- With the gentle immobilization method we developed, the normalization of identified violations of local nonspecific and immune defense proceeds faster - in some cases, improvement in indicators occurs within 7 days (decrease in sIgA, IgM and IL-8), and when examined a month later, the normalization is more pronounced (decrease in sIgA, IgM and IL-8 with an increase in lysozyme activity), which is due to both a less traumatic fixation technique and systemic administration of the biomodulator dietary supplement "Lesmin", which increases nonspecific resistance of the oral cavity and has an antioxidant effect.
Therapeutic immobilization of jaw fragments using laboratory-made splints
Laboratory-made splints are classified as orthopedic immobilization methods. They perform both an independent immobilization function and can be an additional device for various surgical methods of fastening fragments. Removable orthopedic structures include supragingival splints (simple or inclined plane Weber supragingival splint, Vankevich splint, Vankevich-Stepanov splint) and Porta supragingival splint. Non-removable orthopedic structures include dental splints with fixing elements of various modifications. Indications for the use of laboratory-made splints : - severe injuries of the jaws with significant defects of bone tissue, in which bone grafting of the jaw is not performed; — the presence of concomitant diseases in the victim (diabetes mellitus, stroke, etc.), in which the use of surgical immobilization methods is contraindicated; — the patient’s refusal to surgically fix the fragments; — the need for additional fixation of fragments simultaneously with the use of wire splints. To produce laboratory splints, the following conditions are required: a dental laboratory, special materials. Dental work is carried out by dental technicians.
Simple Weber dentogingival splint.
Can be used independently or as one of the main elements when using the surrounding suture method for fractures of the lower jaw. The Weber splint is used for significant defects of the lower jaw as a result of traumatic osteomyelitis or after resection of the lower jaw for a tumor. In these cases, long-term wearing of the splint (for 2-3 months) can lead to the elimination of pronounced lateral displacement of the lower jaw after removal of the splint. The Weber splint is prepared in the laboratory, after taking impressions of jaw fragments. To prevent lateral displacement of fragments, an inclined plane is made on it in the area of the molars. You can make a splint directly in the patient’s mouth from quick-hardening plastic.
Bus Vankevich and bus Vankevich-Stepanova.
They are dental splints supported on the alveolar process of the upper jaw and the hard palate. In the lateral sections it has two inclined planes facing downwards, which abut against the anterior edges of the branches or the alveolar part of the lateral sections of the body of the lower jaw, mainly from the lingual side and do not allow fragments of the lower jaw to move forward, upward and inward. The Vankevich splint is used to fix and prevent lateral and rotational displacement of fragments of the lower jaw, especially with significant defects, due to the emphasis of the inclined planes on the anterior edges of the branches of the jaw. The Vankevich splint as modified by Stepanov differs in that instead of a maxillary base there is a metal arch, like a clasp prosthesis. The Port splint is used in case of a fracture of the edentulous lower jaw without displacement of the fragments and the patient does not have removable dentures and teeth in the upper jaw. The splint consists of two base plates for each jaw, similar to complete removable dentures, rigidly connected to each other in the position of central occlusion. There is a hole in the front section of the tire for food intake. The Porta splint is used in combination with wearing a chin sling bandage.
Dental splints with fixing elements.
Used for immobilization of fragments of the lower jaw in the presence of a bone tissue defect within the dentition, when the fragments have a sufficient number of stable supporting teeth. These splints consist of metal caps fitted to the teeth of the lower jaw. The caps are soldered together and fixed on the teeth of each fragment. With the help of various locks (pins, levers, etc.), after their reposition, the fragments are secured for the period necessary for consolidation. The teeth used for splinting are not prepared.
Fracture of the lower jaw - symptoms and treatment
Diagnosis of patients with fractures of the lower jaw is carried out in order to establish the location, number of fractures, as well as to determine injuries to nearby tissues, vessels and nerves.
Diagnostic methods are basic and additional (instrumental).
Basic diagnostic methods are carried out with a standard set of instruments in the emergency room, dental office or dressing room. The doctor finds out the patient’s complaints, learns about previous diseases and previous operations. At this stage, it is very important to establish the time of injury, since the duration of the injury plays a big role in further treatment tactics.
During the investigation, the doctor will find out whether the injury was sustained at home, at work, or during a fight, and whether it is of a criminal nature. In case of injury during violent acts, the doctor is obliged to report the incident to the police. After that, an internal affairs officer talks with the victim, finding out the details of what happened. In this regard, there is often a concealment of the real reasons for the injury, and the patient sometimes invents very ridiculous and implausible stories.
Sometimes collecting complaints and medical history is difficult or impossible due to the patient’s serious condition or alcohol/drug intoxication.
A clinical study begins with an external examination; post-traumatic swelling, changes in skin color, the presence of abrasions, hematomas, and bleeding are detected. Next, palpation is carried out, during which the nature of the swelling is revealed, inflammatory infiltrate, hematoma, and subcutaneous emphysema are excluded. Palpation of the lower jaw is carried out symmetrically, starting from the branch of the lower jaw and ending in the chin. The presence of a bony step indicates a fracture of the mandible. The degree of mobility of the fragments and the direction of their displacement are also determined.
When examining the oral cavity, special attention is paid to the mucous membrane of the alveolar part of the lower jaw, identifying violations of integrity and bleeding. The relationship of the dentition and the displacement of the central line of the lower jaw when opening and closing the mouth are determined. The landmarks are the labial frenulum, the line between the central incisors of the upper and lower jaw.
Often, the opening of the mouth with jaw fractures is limited. When rocking the lower jaw, relying on the chewing teeth and the basal edge, you can determine the degree of pathological mobility of the lower jaw and the location of the fracture.
Additional diagnostic methods:
- X-ray : an X-ray of the skull is taken in a direct projection in order to exclude fractures of other parts of the face and an X-ray of the lower jaw in lateral projections, the number of fractures, the presence or absence of displacement, diastasis (gap) and the presence of teeth in the fracture line are analyzed.
- An orthopantomogram is a more modern method, with functionality similar to an x-ray. One detailed image is taken, and it is possible to view it on the monitor screen using various programs.
- Computed tomography allows you to most accurately identify fractures of the lower jaw, measure the distance of displacement of fragments, diastasis, determine the size and number of fragments, and the presence of foreign bodies. Using certain setting modes, you can determine the violation of soft tissues (muscles, blood vessels, nerves) and the presence of hematomas.
- Assessment of the general condition of the body - examination of organs and systems of the body, identification of viral and chronic diseases. For this purpose, a physical examination, digital chest x-ray, ultrasound examination, and laboratory diagnostic methods are used. If necessary, consultations with related specialists are carried out. All this helps to select the most effective therapy for the patient, taking into account the characteristics of a particular clinical case.