Causes
Caries is a multifactorial disease. There are the following reasons that contribute to the development of carious lesions.
- Poor oral care – infrequent, insufficient, improper brushing of teeth.
- The presence of cariogenic bacteria in the mouth (lactobacillus and some types of streptococci), which contribute to tooth infection.
- Accumulation of plaque (soft plaque) and stones on the teeth.
- Frequent consumption of flour and sugar-containing products between meals.
- Rare consumption of raw vegetables and fruits.
- Insufficient intake of vitamins D and B1 and minerals, especially calcium, fluorine and phosphorus.
- Change in the quality or quantity of saliva.
- Internal pathology (diseases of the gastrointestinal tract, endocrine organs, nervous system).
- Transfer of cariogenic infection through saliva and kissing on the lips (relevant, for example, when caring for small children).
If people caring for an infant are sick with caries and at the same time lick the pacifier before giving it to the baby, taste food with the same cutlery that the baby then eats, drink from his cup - all this contributes to the transfer of infection from the adult’s mouth to baby's mouth.
As a result, the baby’s oral cavity, free of pathogens, is populated by cariogenic bacteria, which are the triggering factor for caries disease in particular. This same mechanism also operates in cases where those close to you kiss the child on the lips.
When do molars erupt?
Molars are the last teeth that erupt in the child’s lower and upper dentition. As a rule, the first units appear on the lower jaw at the age of 12-18 months, a month later molars erupt on the upper row. The second molars appear in a child between 24 and 30 months of age.
Replacement of primary molars of the lower jaw occurs at the age of 6-8 years. In place of the upper units, molars grow only by the age of 9-12 years. However, these are average indicators and may vary depending on individual characteristics.
The timing of eruption depends on the following factors :
- hereditary predisposition;
- the general health of the child;
- congenital features;
- climatic living conditions;
- nature of nutrition;
- gender of the child.
Symptoms
Chewing teeth are more susceptible to caries due to the more intense load on them. In the initial stages, as a rule, there are no symptoms, except for a cosmetic defect - a round spot of whitish, cream or brownish color.
Over time, the spot turns black and increases in size. A little later, complaints of pain in the tooth appear from sweet, salty or sour foods, from hot or cold drinks. At the same time, a carious defect is usually discovered in the form of a cavity with uneven edges. Due to the frequent accumulation of food debris in it, an unpleasant odor appears from the tooth.
If hard pieces of food fall to the bottom of the carious cavity, a sharp but short-term pain occurs in the tooth. Without treatment, the cavity gradually deepens and reaches dangerously close to the pulp chamber. If measures are not taken, pulpitis will soon develop.
In addition, the “weak point” of molars and premolars are the natural pits and grooves (i.e., fissures) on the chewing surface, in which food debris and debris often accumulate. The deeper these fissures, the higher the likelihood of caries forming in them. Here it appears in the form of darkened grooves, initially mainly in the central part of the tooth, and then spreads over the entire chewing surface.
The process goes deeper, so gradually the destruction reaches the dentin and then sensitivity to chemical and thermal irritants appears. A signal that caries has reached the pulp chamber is the occurrence of spontaneous, twitching or aching pain at night.
Chewing surface of the tooth
The chewing surface of the tooth is the surface of the tooth facing the teeth of the opposite row (directed upward for the lower teeth, and downward for the lower teeth). The chewing surface is also called occlusal, or closure, since it is it that is involved in the formation of occlusion, or the closure of the upper and lower dentition. Its shape and compliance of the chewing surface of the teeth of the upper row with the chewing surface of the teeth of the lower row is important for complete chewing and grinding of food.
The chewing surface in the proper sense is present in large and small molars ( molars and premolars ), since they perform the main function of chewing and grinding food. In incisors and canines, the cutting edge is directed towards the teeth of the opposite row, which is usually quite narrow. The cutting edge is used to bite off food. In canines, this edge is usually narrowed and pointed to one degree or another, and is partially involved in tearing tough pieces of food (for example, meat fibers). In predators, fangs are the main teeth with which they bite off (tear off) pieces when eating prey. In humans, due to the fact that his ancestors were omnivores, that is, they could eat both animal and plant foods, as well as the transition to a diet consisting of food that was mainly heat-treated, the size of the fangs is smaller than that of predators, and their function is mainly to participate, along with the incisors, in biting off food.
In total, the crown of the tooth has several surfaces:
- Chewing surface
- The vestibular surface is the surface directed towards the vestibule of the mouth. In the front teeth it is also called the labial surface, since it is directed towards the lips, and in the rear teeth it is called the buccal surface, since it is directed towards the mucous membrane of the cheeks.
- The lingual surface is the surface opposite to the vestibular one, and facing the actual oral cavity and tongue. It is also called oral (from oris - Latin mouth).
- The contact surface, or approximal, is the surface directed towards adjacent teeth. The approximal surfaces facing towards the center of the dentition (forward) are called mesial surfaces of the teeth. In the case of the front teeth (incisors), these surfaces are called median. The approximal surfaces directed backwards towards the posterior teeth are called distal.
The shape of the chewing surface of teeth is individual and varies depending on the anatomy of a particular person. Typically, the chewing surface of premolars consists of 3-4 cusps, molars - of 4-5 cusps. In practice, in specific patients, there is often a deviation in the number of teeth in the direction of either increasing or decreasing their number. However, molars with a chewing surface consisting of 7 or more cusps are extremely rare.
Copying the chewing surface of teeth as accurately as possible is one of the most difficult tasks in dental prosthetics facing the dentist and dental technician. It is necessary to take into account all the nuances of the individual characteristics of the chewing surface so that the manufactured prosthesis or crown performs its function as fully as possible, and so that the achieved result meets all the requirements in terms of aesthetics. Even a small error in the restoration of the chewing surface of the lateral teeth can lead to the fact that chewing food will be incomplete or difficult, and the patient will experience unpleasant sensations of incomplete closure of the dental arches and discomfort. A precisely executed and reproduced chewing surface of the teeth makes artificial crowns as aesthetically pleasing and natural as possible, and the process of chewing food is carried out in the most complete and physiological manner.
come back
Tooth anatomy
The structure of all units is the same, but each tooth has a distinctive shape and dimensions, depending on the functions it performs.
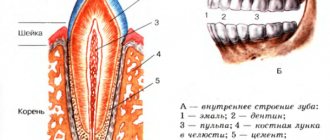
Internal structure of teeth in the photo
What does a tooth consist of? The top layer (enamel) is predominantly composed of minerals. It protects the inner layers of the tooth from mechanical, thermal and chemical damage. The rest of the solid surface of the elements consists of proteins and liquid involved in metabolic processes. This layer tends to wear out and wear off over time. Typically, caries first affects the surface of the tooth. For this reason, you should carefully monitor the condition of the oral cavity and carry out hygiene procedures in a timely manner.
If you examine a tooth in cross-section, you can also see dentin. It also consists of mineral substances and protects the pulp with the nerve fibers located in it. Many small channels are localized in dentin, with the help of which metabolic processes in bone tissue are carried out. Through these structures impulses are transmitted between nerve endings. For 1 sq. mm of dentin there are about 70,000 microscopic tubules.
The internal cavity of the elements is represented by pulp. It consists of nerve endings and lymph nodes.
The structure of the tooth should be considered depending on its location relative to the gum. The visible part of the element is the crown. The area of contact between the tooth and the gum is called the periodontium. The root is located in a special cavity, which dentists call the alveolus. The root of the tooth ends at an apex, which is supplied with blood vessels. Through these structures, the elements are fed.
No Ads
Material and methods
In 2010 - 2011 in the Department of Plastic and Maxillofacial Surgery of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky performed 15 operations on the upper jaw using the iliac crest and 20 operations on the lower jaw with parietal autografts; in all clinical situations, the possibility of placing dental implants was achieved.
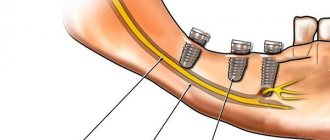
To eliminate the vertical deficiency of bone tissue in the area of implant placement in the projection of the mandibular neurovascular bundle, we used the transplantation of parietal autografts from the lingual and vestibular sides. Bone chips were compacted between the bone blocks (see Fig. 8,9). After 6 months, we removed the skeletal screws and installed dental implants.
To reconstruct the alveolar process in the projection of the maxillary sinus with extended defects and severe atrophy of 0.5 mm, the iliac crest was used with osteotomy of the anterior wall of the maxillary sinus and fixation of the graft to the palatine bone. After 6 months, the implants were installed (see Fig. 14, 15, 16).
Patient A. , 59 years old, came to the clinic for the manufacture of fixed dentures on the lower jaw. The patient had bone tissue atrophy, 2-3 mm down to the mandibular canal.
Orthopantomogram of patient A. before surgery
Treatment choice tactics: three-dimensional reconstruction of the alveolar process in the lateral areas using mandibular cortical autoblocks is impossible due to the insufficient volume of donor bone tissue.
In this case, we chose the parietal bone, since the resorption of bone grafts of intramembranous origin occurs more slowly than that of enchondral ones [5].
For access and collection of parietal autografts, a semi-coronal incision was used. We collected 4 parietal autografts measuring 4*2.5 cm and 3*2 cm in quantities of 3 and 1, respectively.
Access for harvesting and harvested parietal bone autografts
The collected bone blocks were fixed. After fixation of the bone blocks, the space between the autografts (vestibular and lingual) is augmented with autografts mixed with venous blood.
Fixation of autologous bone grafts from the vestibular and lingual sides, augmentation with autoshafts, scheme for fixation of grafts from the vestibular and lingual sidesA similar operation was performed on the left. The wounds are sutured with U-shaped and interrupted sutures, without tension, creating mucoperiosteal “bags”.
Orthopantomogram of patient A. after surgery
After 6 months, dental implantation was performed. During implantation, there was a good blood supply to the bone tissue, which was similar in properties to the mandibular tissue. The negative side of this method is the need to perform vestibuloplasty at the stage of installing gum formers.
Dental implantation patient A. after 6 months
Orthopantomogram of patient A. after dental implantation
Patient B. , 32 years old, came to the clinic to install dental implants in the area of teeth 25,26,27. An orthopantomogram and CT scans showed a height of the maxillary sinus floor of less than 0.5 mm, which is called the “eggshell” symptom.
Orthopontomogram of patient B. patient before surgery
A trapezoidal incision was made from 23 to 27, and the mucoperiosteal flap was detached. A through defect in the anterior wall of the maxillary sinus was noted, which makes successful sinus lift difficult. An osteotomy of the anterior wall and floor of the maxillary sinus was performed. An autograft was collected from the iliac crest according to the defect of the alveolar process of the upper jaw. Modeling was performed and the graft was fixed to the palatal wall of the maxilla with long screws, the anterior wall of the maxillary sinus was returned to its place and fixed. The wounds are sutured with periodontal and interrupted sutures.
Stages: incision and tissue detachment, harvesting, fixation of the iliac crestThus, since the ilium is enchondral, covering the vestibular and palatal sides with cortical plates, we give it the properties of membranous bone.
Postoperative orthopantomogram and fixed bone graft
After 4 months, dental implantation was performed. When forming a bed for implants, good blood supply to the graft and an increase in bone tissue density were noted.
Orthopantomogram of patient B. after surgery
Patient V. , 70 years old, went to a private dental clinic. The patient was noted to have unilateral vertical atrophy of the alveolar process of the mandible. Vertical reconstruction was performed using mandibular blocks under local anesthesia.
Orthopantomogram of patient V. before surgery
Mandibular bone blocks and fixed grafts from the vestibular and lingual sides
Split free bone grafts from the branches of the lower jaw were fixed on the vestibular and lingual sides, the space between the grafts was augmented with xenogeneic material "BiOss". The wounds are sutured with U-shaped and interrupted sutures to form mucous-muscular “bags”.
Orthopantomogram of patient V. after surgery