- Causes of salivary gland cancer and risk groups
- Symptoms of the disease
- Diagnostic methods
- Classification: types of salivary gland cancer
- Stages of the disease
- Treatment
- Complications and relapses
- Life prognosis at different stages of cancer and prevention
The salivary glands produce saliva, a liquid found in the oral cavity that performs some important functions: wetting the mucous membrane, food, facilitating articulation, swallowing, protecting against pathogenic bacteria, etc. There are two groups of salivary glands:
- Large: sublingual, parotid, submandibular.
- Small ones have a microscopic structure, scattered throughout the oral cavity - there are several hundred of them in total.
Cancer can develop in all of these glands. Most often (in 7 out of 10 cases), benign and malignant tumors arise in the parotid salivary glands. Approximately 1–2 tumors out of ten occur in the submandibular salivary glands; in 50% of cases they are malignant. In rare cases, cancer develops in the sublingual or minor salivary glands.
Causes of salivary gland cancer and risk groups
A normal salivary gland cell becomes cancerous when a certain set of mutations occurs in it. The development of malignant tumors is caused by mutations in oncogenes (genes that activate cell reproduction) or tumor suppressor genes (suppress cell reproduction, “repair” damaged DNA, trigger programmed cell death - apoptosis). In each specific case, it is very difficult to judge the reasons for the mutations that occurred in cells. It is impossible to say why exactly they happened.
There are some risk factors that increase the likelihood of developing a malignant tumor:
- The older a person is, the more changes in his genes accumulate, the higher the likelihood of developing various types of cancer.
- Salivary gland cancer is more common in men than in women.
- Irradiation of the head. For example, this may be a previous course of radiation therapy, exposure to ionizing radiation in the workplace.
- There is evidence that the risk of salivary gland cancer is increased in people who have certain occupational hazards: contact with asbestos, nickel alloy dust, work in enterprises that produce rubber and woodworking.
The role of heredity is currently considered insignificant. Most patients do not have a family history (close relatives who have been diagnosed with the same type of cancer). The role of alcohol and tobacco has not been proven. These unhealthy habits are known to increase the risk of head and neck cancer in general, but no association has been found with salivary gland cancers.
Is a mobile phone dangerous? In one study, researchers found that heavy cell phone users were more likely to have parotid tumors (usually benign). But other studies have not found such a relationship.
Performing surgery to remove the salivary gland
With the traditional method of surgery, the patient assumes a lying position with his head thrown back and to the side. The operation involves local infiltration anesthesia. Several parallel incisions are made in the submandibular area, the tissue is lifted, and the capsule of the salivary gland is discovered, which is opened, and the gland tissue is extremely carefully removed and removed. When a malignant tumor grows together with nearby tissues, the latter are also removed. After this, stitches are applied.
During endoscopic surgery, both local and general anesthesia can be used. Through small punctures in the tissue, manipulators and a video probe are inserted, which projects all the actions performed on the screen. When the manipulators reach the gland, small incisions are made with their help, through which pathological tissue is removed. The endoscopes are then removed and sutures are placed at the puncture sites.
Postoperative care of the surgical site includes:
- hygiene - no water or dirt should get into the wounds;
- special diet - the diet will consist of semi-liquid warm food, no hot or cold drinks, no alcohol;
- smoking ban;
- special treatment - it is recommended to regularly treat the seams with antiseptics, and the oral cavity after each meal should be rinsed with a mixture of antiseptic and water.
If all the recommendations of the attending physician are followed, complete wound healing occurs within a few months.
Symptoms of the disease
Benign and malignant tumors of the salivary glands present with similar symptoms. One of the main differences is that cancer grows much faster and more often leads to a number of symptoms associated with growth into surrounding tissues and compression of nerves.
You need to visit a doctor if you are bothered by the following symptoms:
- A lump or swelling has appeared in the mouth, cheek, jaw, or neck.
- You have noticed that your face has become asymmetrical.
- I am worried about pain in the mouth, neck, ear, cheek, jaw. It doesn't last long.
- Numbness of part of the face.
- Weakness in the facial muscles, because of this, half of the face may be “lowered,” which becomes especially noticeable when baring teeth or frowning.
- I can't open my mouth wide.
- Difficulty swallowing.
Symptoms
A stone located in the duct of the salivary gland clogs the duct and prevents the flow of saliva into the mouth. In this case, saliva collects in the salivary gland, which becomes swollen and often painful. Depending on the location of the stone, pain and swelling occurs either under the jaw (submandibular gland) or in front of the auricle and in the area of the angle of the jaw bone (parotid gland). Some stones can be removed endoscopically through the mouth under local anesthesia as an outpatient procedure, but sometimes the entire salivary gland must be removed. Most often, stones are found in the submandibular gland.
The tumor is usually palpable as a nodule in the salivary gland and can cause swelling, pain, and facial nerve dysfunction. Even a benign tumor usually must be removed.
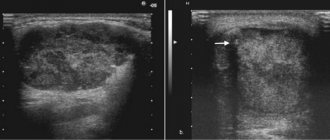
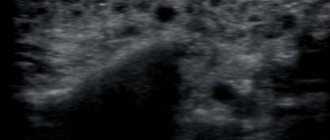
Diagnostic methods
During the initial appointment, the oncologist talks with the patient, questions him, trying to find out risk factors, and conducts an examination. The doctor feels the tumor on the face and cervical lymph nodes, evaluates the sensitivity of the face and the work of facial muscles. After this, the patient can be referred for additional consultation to an ENT doctor.
Computed tomography and magnetic resonance imaging help assess the size, shape and location of the tumor, and detect lesions in the lymph nodes and other organs. The current gold standard for searching for distant metastases is PET scanning. If the tumor is located near the jaw, an x-ray is taken. A chest x-ray helps detect metastases in the lungs and evaluate the condition of the lungs and heart before surgical treatment.
The most accurate method for diagnosing salivary gland cancer is a biopsy. During this procedure, the doctor receives a fragment of pathologically altered tissue and sends it to the laboratory for cytological and histological examination.
The most common procedure is fine-needle aspiration biopsy. Tumor tissue is obtained using a hollow needle similar to the one used for injections. If the required amount of tissue cannot be obtained, the doctor performs an incisional biopsy: makes an incision and removes part of the tumor.
If tumor cells are found in the sample, the diagnosis of cancer is virtually certain.
Prevention
To prevent any pathological processes in the OSJ, it is recommended:
- visit the dentist regularly;
- follow all the rules of daily oral care;
- strengthen immunity;
- promptly treat all viral and infectious diseases;
- eat sour vegetables and fruits (to stimulate saliva production).
So, the salivary glands are the largest salivary glands in the human body, producing about a third of the total secretion volume. These formations are susceptible to inflammatory processes of infectious and autoimmune origin, they can become foci of the formation of benign and malignant tumors, and salivary stones also develop in the OSJ. Careful care of the oral cavity, balanced nutrition and timely medical assistance at the first symptoms of “local” problems will help to avoid complications of the most common diseases of the salivary glands (from dysfunction of the salivary glands to sepsis).
Classification: types of salivary gland cancer
The salivary glands are made up of different types of cells, any of which can give rise to a malignant tumor. Therefore, there are different types of cancer:
- Mucoepidermoid carcinoma of the salivary gland is the most common type. Most often it is found in the parotid salivary glands, less often in the submandibular and small ones. These tumors are rarely aggressive.
- Adenoid cystic carcinoma is characterized by very slow growth and rare metastasis. However, this malignant tumor can be very difficult to get rid of: it can recur a long time after treatment.
- Adenocarcinoma is a malignant tumor that develops from glandular cells. Different types of adenocarcinomas can occur in the salivary glands: acinic cell carcinoma, low-grade polymorphic adenocarcinoma, basal cell adenocarcinoma, clear cell carcinoma, cystadenocarcinoma, etc.
- Rare types of malignant cancers of the salivary glands include: squamous cell carcinoma, epithelial-myoepithelial carcinoma, anaplastic small cell carcinoma, undifferentiated carcinomas.
Removal of the parotid, submandibular gland, removal of cervical lymph nodes
The salivary glands are divided into minor and major salivary glands. There are 3 pairs of large salivary glands: the parotid salivary glands, located below and in front of the auricle directly under the skin, the submandibular salivary glands and the sublingual glands, located under the mucous membrane of the floor of the mouth. The minor salivary glands are located in the mucous membrane of the mouth, palate, cheeks and lips. Various tumors, stones, and recurrent infections are the most common reasons for operations on the salivary glands.
Stages of the disease
Salivary gland cancer, like other malignant tumors, is classified into stages according to the generally accepted TNM system. The letter T in the abbreviation denotes the characteristics of the primary tumor: the size and degree of its growth into surrounding tissues, N - spread to the lymph nodes, M - the presence of distant metastases. Depending on these indicators, the following stages are distinguished during salivary gland cancer:
- Stage 0 is “cancer in situ” (carcinoma in situ). The tumor is located within the layer of cells that form the salivary gland and does not grow into neighboring tissues.
- Stage I is a tumor that is located within the salivary gland and measures no more than 2 cm.
- Stage II - the tumor reaches a size of more than 2 cm, but not more than 4 cm.
- Stage III - a tumor that reaches a size of more than 4 cm and/or spreads into surrounding tissues, or a tumor of any size that has grown into surrounding tissues, has spread to one cervical lymph node on the same side, and the focus in the lymph node is no more than 3 cm and does not extend beyond its borders.
- Stage IV includes substages IVA, IVB or IVC. The first two are characterized by varying degrees of spread of the malignant tumor to the anatomical structures of the head, neck, and lymph nodes. If stage IVC is diagnosed, it means that there are distant metastases.
In addition to stages, there are three degrees of malignancy of salivary gland cancer:
- Grade I - low degree of malignancy. Such tumors are called highly differentiated. Tumor tissue is as similar as possible to normal salivary gland tissue. It grows slowly, and the prognosis for such patients is most favorable.
- Grade II are moderately differentiated tumors. Tumor tissue differs more significantly from normal tissue. This cancer is more aggressive and has a poorer prognosis.
- III degree - poorly differentiated tumors. Cancer cells almost completely lose the features of normal ones. Such tumors behave the most aggressively.
Determining the degree of malignancy helps the doctor predict how the cancer will behave and plan treatment correctly.
Acute non-epidemic parotitis
Acute non-epidemic parotitis is inflammation of the parotid gland as a result of impaired salivation due to general and local factors.
Causes of non-epidemic mumps
The causes of non-epidemic mumps, as mentioned earlier, are general and local factors.
Common factors include infectious diseases, exhaustion of the body, and surgical interventions. Local factors: inflammation of the mucous membrane, foreign body in the excretory duct of the gland, lymphadenitis, otitis media, sinusitis.
Non-mumps clinic
The non-mumps clinic is quite vibrant. The patient complains of pain and swelling, most often in the area of one gland. Body temperature is above 39 C. Then the entire parotid area swells, the earlobe protrudes, difficulty swallowing and breathing appears, and after this xerostomia appears. Due to swelling, the skin in the outer ear area is smoothed, the ear canal is compressed, and hearing is reduced. When massaging the gland, a cloudy or purulent exudate appears. Inflammation increases for 3-4 days, then acute inflammatory reactions subside, and compaction remains in the area of the gland for a long time.
There are 3 forms of acute non-epidemic parotitis: catarrhal, purulent, gangrenous.
The purulent form is characterized by intense tearing pain. This occurs due to the accumulation of pus, formed from the breakdown of glandular tissue, under the capsule of the gland. Over time, a fistula may form in the external auditory canal, then spread into the peripharyngeal space with the formation of peripharyngeal phlegmon, up to mediastinitis.
The gangrenous form is characterized by extensive tissue necrosis and the development of mediastinitis, thrombosis, phlebitis, and sepsis.
Treatment of non-mumps
Treatment of non-epidemic mumps at the initial stage is conservative. A gentle diet, UHF, dry heat and compresses based on dimexide, anti-inflammatory drugs, and antibiotics are prescribed. Sulfonamide drugs intramuscularly and antibiotic-novocaine blockades subcutaneously and from the oral cavity along the excretory duct are indicated.
In severe cases, antibiotics are prescribed every 3 hours. Also, washing the excretory ducts with chymotrypsin has a good effect. For purulent forms, treatment is surgical. One incision is made along the angle of the jaw, the pancreas and parotid-masticatory fascia are dissected, and a second incision is made along the edge of the zygomatic arch and drainage is placed.
Prevention of non-epidemic mumps
Prevention of non-epidemic mumps includes good oral hygiene, administration of salivary agents in case of xerostomia and disinfectants that are secreted through the salivary glands (phenyl salicylate, hexamethylenetetramine).
Treatment
The patient is treated by a team of doctors, which may include: a clinical oncologist, an ENT doctor, an oncologist-surgeon, an oral and maxillofacial surgeon, a chemotherapist, a radiotherapist, etc. The treatment program is determined by the stage of cancer, the histological type of the tumor, its location (which gland is affected) , age, general condition and concomitant diseases of the patient.
Surgery
If the tumor has not grown much into the surrounding tissue, then it is resectable, that is, it can be removed surgically. The surgeon’s task is to excise the tumor while capturing the surrounding tissue so that there are no cancer cells left on the cut line, that is, to ensure a negative resection margin. If tumor cells have spread to the lymph nodes, or a biopsy reveals aggressive cancer, the lymph nodes are also removed.
For parotid salivary gland cancer, surgery presents certain difficulties, because the facial nerve passes through the gland, which controls the work of facial muscles. If the tumor affects only the superficial lobe of the gland, you can remove it separately - perform a superficial parotidectomy. There is no risk of damaging the facial nerve. In some cases, it is necessary to remove the entire gland, and if the tumor has grown into the facial nerve, then it too.
For cancer of the sublingual and submandibular gland, the surgeon removes the gland itself and some of the tissue located around it, including, possibly, bone tissue. In some cases, it is necessary to excise the nerves that control sensitivity, movements in the lower part of the face, in the tongue, and the sense of taste.
For cancer of small glands, the affected gland and part of the surrounding tissue are removed. The extent of the operation depends on the size and location of the tumor.
Radiation therapy
Indications for the use of radiation therapy for malignant tumors of the salivary glands:
- To combat malignant tumors that cannot be removed surgically due to their location or size. Sometimes radiation is supplemented with courses of chemotherapy.
- After surgical treatment. This type of radiation therapy is called adjuvant and is sometimes combined with chemotherapy. Radiation after surgery helps destroy remaining cancer cells and prevent recurrence.
- For advanced cancer. In this case, radiation therapy is aimed at combating pain, difficulty swallowing, bleeding and other symptoms.
Radiation is typically given five days a week for 6–7 weeks. If radiation therapy is used for palliative purposes, the course will be shorter.
Chemotherapy
Chemotherapy is used quite rarely for malignant neoplasms of the salivary glands. Anticancer drugs can reduce the size of the tumor, but are not able to completely destroy it. They are most often prescribed for advanced cancer as palliative treatment or in addition to radiation therapy.
Depending on the type and other characteristics of the cancer, the doctor may prescribe combinations of different chemotherapy drugs: carboplatin, cisplatin, 4-fluorouracil, doxorubicin, paclitaxel, cyclophosphamide, vinorelbine, docetaxel, methotrexate. Chemotherapy for cancer is always given in cycles. The patient is administered the drug, then takes a “break” for several days. The course of treatment may consist of several cycles.
Rehabilitation
After treatment, some problems associated with nerve damage may persist: dysfunction of the facial muscles, speech disorders, swallowing, and cosmetic defects. Some side effects of chemotherapy and radiation therapy go away after treatment is completed, while others persist for a long time. In such cases, rehabilitation courses are indicated. The doctor draws up a rehabilitation treatment program individually, depending on the severity and nature of the disorders.
Complications after surgery
During surgery to remove the parotid gland, the facial nerve can be impacted, sometimes causing facial nerve palsy, usually the inferior branch, which can cause the corner of the mouth to droop. Typically, facial nerve paresis recovers within a few weeks with facial exercises, and only in rare cases does the facial nerve fail to recover.
Sometimes the cancer affects the facial nerve and then the facial nerve is completely removed, in which case the paralysis is permanent. However, the condition can usually be improved through various surgical interventions.
After removal of the parotid salivary gland, the pinna of the ear is usually partially numb, but over time some sensitivity returns. Due to the risk of frostbite, the auricle must be properly protected from the cold.
During surgery to remove the submandibular gland, the facial nerve may be injured (stretched), causing temporary dysfunction of the corner of the mouth, but permanent damage caused by this branch of the facial nerve is very rare. Damage to the sensory and motor nerves passing under this gland is extremely rare.
After parotid surgery, saliva may leak from the wound, especially when eating. Salivary secretion is harmless and usually ends spontaneously. Surgery to remove one salivary gland does not cause noticeable dry mouth.
Complications and relapses
Even if the treatment is successful and the examination results show no signs of the presence of cancer cells in the patient’s body, a relapse may occur in the future. Therefore, you need to regularly see an oncologist, come for examinations, undergo various studies and take tests.
Typically, the doctor prescribes examinations once every few months for several years, then less frequently.
- If cancer recurs, treatment options may vary:
- If the tumor can be removed, surgery is performed followed by a course of radiation therapy.
- If the tumor cannot be removed surgically, the doctor prescribes radiation therapy in combination with chemotherapy.
- If there are distant metastases, chemotherapy becomes the main treatment method. Radiation therapy and surgery can be used to control some symptoms.
With advanced cancer with metastases, achieving remission becomes extremely unlikely. In this case, treatment will be aimed at slowing the progression of cancer, combating symptoms, and prolonging the patient’s life.
Euroonco doctors undertake cancer treatment at any stage. For us there are no hopeless patients. You can always help, and we know how to do it correctly, we have all the necessary technologies, the latest generation drugs.