Acute sialadenitis on ultrasound
Inflammation of the salivary glands is called sialadenitis.
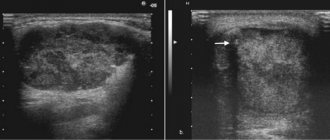
Acute bacterial sialadenitis develops when the infection is introduced hematogenously or through the excretory ducts, as well as from an open injury. Many viruses (for example, mumps virus, influenza, cytomegalovirus) have an affinity for glandular tissue, including the parenchyma of the salivary glands. In acute sialadenitis, a painful swelling appears in the area of the salivary glands, and the amount of saliva secreted decreases. As a rule, during viral infections several salivary glands are affected. In acute sialadenitis, ultrasound shows an increased size of the affected glands; the echogenicity of the parenchyma is reduced, often heterogeneous due to oval hypoechoic areas; the contour of the gland is clear and slightly convex; blood flow is often increased. It is likely to encounter enlarged regional lymph nodes with increased central blood flow. Acute sialadenitis is not characterized by dilated ducts, increased echogenicity of their walls, or hyperechoic inclusions in the parenchyma of the gland.
| Photo. With viral mumps on ultrasound, the parotid gland (A, B) is enlarged, the parenchyma is hypoechoic, heterogeneous due to small anechoic ovals, the color circulation determines dilated vessels; blood flow is noticeably increased (B). Conclusion: Echo signs of acute mumps. | ||
| Photo. A 5-year-old girl with a temperature of 38.6ºC, a wet cough and painful swelling in the parotid region on the right. On ultrasound, the right parotid gland (A, B) is enlarged, the parenchyma is hypoechoic, heterogeneous due to small anechoic ovals, the color circulation determines dilated vessels; blood flow is noticeably increased. The parotid gland on the left (B) is unchanged. In the general blood test, lymphocytosis, the level of IgM antibodies to the mumps virus is increased. Diagnosis: acute mumps. | ||
| Photo. A, B — On ultrasound, the parotid gland is enlarged, the contour is wavy, the parenchyma is hypoechoic, heterogeneous due to small almost anechoic ovals, probably dilated vessels; enlarged lymph nodes are detected. Conclusion: Echo signs of acute mumps, secondary lymphadenitis. B - Echo signs of acute parotitis in the main gland and accessory lobule. | ||
Journal "Child's Health" 5 (32) 2011
Sialadenitis is an inflammation of any salivary gland; mumps - inflammation of the parotid salivary gland. Sialadenitis can be primary (an independent disease) or more often secondary (a complication or manifestation of another disease). The process may involve one gland or two symmetrically located ones at the same time, and sometimes there may be multiple lesions of the glands. Sialadenitis occurs acutely or chronically, often with exacerbations [1, 2, 5–7].
Etiology and pathogenesis
The development of sialadenitis is usually associated with infection. Primary sialadenitis, represented by mumps, is associated with a viral infection. Acute viral sialadenitis can also be caused by influenza viruses, herpes, cytomegalovirus, Coxsackie virus and other viruses. Secondary sialadenitis is caused by a variety of bacteria and fungi. In the ducts of the salivary glands with sialadenitis, a mixed flora is found, consisting of staphylococci, pneumococci and streptococci. The cause of inflammation can also be pathogens of actinomycosis, tuberculosis or syphilis. The routes of infection into the gland are different: dental (infectious agents enter the salivary gland through the mouth of the excretory duct, which is sometimes preceded by the introduction of a foreign body into the duct - villi from a toothbrush, apple peel), hematogenous, lymphogenous, contact. Sialadenitis of a non-infectious nature develops due to poisoning with salts of heavy metals (when they are excreted in saliva). Unfavorable factors in the development of the disease are: gingivitis, stomatitis, dental plaque, complicated caries, poor oral hygiene [1, 2, 5, 6]. In addition, acute sialadenitis includes acute parotitis of the newborn, which occurs most often in premature, weakened children with an unfavorable premorbid background.
Classification of inflammatory diseases of the salivary glands in children. Sialadenitis according to its clinical course is divided into:
1) acute: specific, nonspecific (bacterial);
2) chronic: parenchymal, interstitial, sialodochitis;
3) chronic in the acute stage, in the remission stage;
4) chronic specific: tuberculous, actinomycotic;
5) salivary stone disease in the remission stage, in the acute stage.
Among acute specific sialadenitis in children, acute mumps is the most common. Acute nonspecific sialadenitis in children is much less common. The parotid salivary glands are most often affected.
The clinical picture , characteristic of an infectious-inflammatory disease in a child, is aggravated by concomitant (causal) diseases. Most often, one parotid salivary gland is affected. The disease begins acutely with complaints of pain in the gland area, increased body temperature, weakness, and malaise. Locally the gland is enlarged and painful on palpation. The mouth of the Stenon's duct gapes and is hyperemic. During massage, cloudy, thick, viscous saliva is released from the duct. A characteristic sign is dysfunction of the gland in the form of hypo- or hypersalivation, as well as the appearance in the saliva of flakes of mucus, pus, and a large number of desquamated epithelial cells. A general blood test reflects the nonspecific nature of inflammation (leukocytosis, neutrophilia, increased ESR). With purulent sialadenitis (mumps), in addition, hyperemia of the skin over the gland, discharge of pus from the duct of the salivary gland when massaging it, narrowing of the external auditory canal, etc. are possible. General reactions of the body are also pronounced [1–3, 7].
When treating children with acute sialadenitis, great importance is attached to etiopathogenetic therapy. Treatment is carried out with antibacterial, antifungal, antiviral drugs, depending on the type of pathogen; hyposensitizing agents, as well as drugs that increase the body's resistance. Locally, to normalize salivation, instillation of the excretory ducts of the gland with solutions of antiseptics, antibiotics, light massage of the gland, application of a dimexide solution to the area of the gland, vacuum drainage, bougienage of the mouth of the excretory duct in case of stone formation in the ducts of the salivary glands are used. After normalization of salivation, a salivary diet, massage, and physical therapy (UHF) are indicated. For purulent sialadenitis, antibacterial, detoxification, hyposensitizing, immuno- and restorative therapy are additionally used. The prognosis for timely treatment is favorable [1–3, 7].
Complications and outcomes
Acute sialadenitis ends with recovery or transition to chronic. The outcome of chronic sialadenitis is sclerosis of the gland with atrophy of the acinar sections, stromal lipomatosis, with a decrease or loss of function, which is especially dangerous in case of systemic damage to the glands (Sjogren's syndrome), as this leads to xerostomia. With the progression of acute sialadenitis, the inflammatory process can result in an abscess or purulent-necrotic phlegmon of the parotid area. In these cases, surgical treatment is used - opening the phlegmon. Acute sialadenitis can be complicated by stenosis of the salivary ducts, the formation of salivary fistulas, and a persistent decrease in gland function.
In childhood, chronic parenchymal sialadenitis (mumps) of the parotid salivary gland . The disease develops most often as a type of primary chronic inflammation. It is characterized by a long course with periods of exacerbation, most often in the area of one gland.
The causes of chronic parenchymal mumps (CPM) have not been fully identified. One of the possible factors is a violation of the tone of the excretory ducts, which leads to saliva retention and the development of inflammation in the parenchyma of the gland. Many authors consider the cause of CPP to be a congenital malformation of the salivary gland - the presence of congenital cystic cavities in the area of the acini, which also contributes to the retention of saliva and the occurrence of inflammation. It has also been established that morphological changes in the gland that occur after mumps, contribute to the occurrence of CPP. The disease is possible with diabetes mellitus and other neuroendocrine diseases. Particular importance in the development of exacerbations of CPP is given to a decrease in the body’s resistance and levels of nonspecific defense factors. CPP can be an outcome of the acute form of the disease [1, 2, 4–7]. Chronic mumps may be one of the manifestations of Sjogren's and Mikulicz syndromes.
The clinical picture of the disease is different during the period of remission and during the period of exacerbation of the process. There are three forms of chronic (nonspecific) sialadenitis: parenchymal, interstitial and with damage to the ducts (chronic sialadenitis). The connective tissue growing in the stroma compresses or replaces the parenchyma, and the narrowing of the excretory ducts of the gland leads to sialostasis. With sialodochitis, the gland ducts are unevenly dilated, infiltration and tissue sclerosis are observed around the ducts. When stones form in the ducts of the salivary gland, chronic calculous sialadenitis develops. Exacerbations of CPP are observed more often in the cold season, often after ARVI and other infectious diseases. The patient complains of an enlarged gland and pain in its area. Palpation reveals a dense, lumpy and painful gland. When you massage it, pus or muddy, salty-bitter saliva with lumps of mucus is released from the duct. The general reaction of the body is characteristic - fever, intoxication, leukocytosis, etc. Treatment of children with CPP in the acute stage is almost the same as for acute sialadenitis. But more attention is paid to general strengthening treatment and immunotherapy.
During the period of remission, the disease is clinically mild. Thus, general reactions, as a rule, are absent. Locally, the gland is somewhat “grainy” upon palpation. When massaging the gland in the morning on an empty stomach, cloudy, viscous, bitter-salty saliva may be present. When conducting contrast sialography during this period, characteristic cavities in the form of a “bunch of grapes” are visible; the ducts of the 3rd, 4th, 5th order are unclear and intermittent. In the late stage of the disease, the main excretory duct is dilated and uneven (sialodochitis). Diagnosis of the disease is based on medical history and clinical and radiological picture. CPP should be differentiated primarily from lymphadenitis of the parotid region and mumps, and rarely from tumors [1–4, 7].
The diagnosis of chronic sialadenitis is established on the basis of complaints, objective examination data, data from special research methods - radiography, radionuclide scanning, sialography, ultrasound. These methods make it possible to determine the form and stage of sialadenitis, and also to carry out differential diagnosis with a tumor of the salivary gland. To identify a specific process, purulent discharge is examined and serological studies are performed.
Treatment of patients with chronic parenchymal parotitis is aimed primarily at preventing exacerbations of the inflammatory process. For the purpose of immunization, multivitamins, immunostimulants, etc. are prescribed. The body is hardened. Locally, the greatest importance is attached to the sanitation and hygiene of the oral cavity. In addition, other foci of chronic inflammation are sanitized. In order to prevent exacerbation of the disease, systematic massage of the gland, the use of a salivary diet, and prevention of hypothermia are recommended. Periodically (once every quarter or six months), courses of therapy should be carried out, including UHF therapy, potassium iodide electrophoresis, paraffin therapy, laser therapy and other methods of physiotherapy. All patients with CPP require clinical observation immediately from the moment of diagnosis. The purpose of medical examination is to prevent exacerbations of the disease. Children are removed from dispensary registration in case of persistent (2–3 years) remission of the disease [1–4, 7].
We provide a description of a case of chronic sialadenitis in a preschool child. Child M., born July 21, 2001, was under our supervision from June 2007 for 3.5 years.
From the life history : a child from the third pregnancy, which proceeded with the threat of termination in the first and second half of pregnancy, was born at 35–36 weeks, with a body weight of 1920. He was treated in the neonatal pathology department of the city hospital No. 3 of Mariupol for respiratory syndrome disorders of stage II, multiple atelectasis in the lungs, postelectatic pneumonia, DN II against the background of stage I prematurity, ante- and intrapartum hypoxic damage to the central nervous system, depression syndrome. A child from the ChDB group often suffers from colds and sore throats. In 2009, a bilateral tonsillectomy was performed. At the dispensary with an ophthalmologist regarding convergent strabismus and amblyopia on the right. He was treated for intestinal giardiasis.
History of the disease. From the age of two, frequent (up to 3-4 times a year) relapses of mumps and the phenomenon of bilateral sialadenitis are observed. Relapses of the disease occurred with symptoms of intoxication, an increase in body temperature to high levels (38–39 ° C), a significant increase in the parotid salivary glands, more on the left, their sharp pain, the inability to open the mouth, eat, chew, and enlarged lymph nodes in the cervical group. The child was treated on an outpatient basis and was examined several times by pediatricians, a surgeon, an ENT doctor, and a dentist. A diagnosis of acute lymphadenitis of the parotid region was repeatedly made, and mumps was excluded. In a general blood test during relapses of the disease, leukocytosis was noted from 13.4 to 15.8 G/l, increased ESR from 21 to 32 mm/h, neutrophilia (band 4–5%, segmented 55–57%), the presence of basophils was noted - 1-2%, young - 1%, plasma cells - 1-2%. Antibacterial drugs have always been used in therapy.
An objective examination (June 2007) revealed that the boy was in moderate condition, with a body temperature of 39.5 °C. The skin is pale, there is a blush on the cheeks. There is general weakness, severe pain on both sides in the parotid region, inability to open the mouth, eat, and chew. In the parotid region on both sides, more on the left, there is a significant increase in the parotid salivary glands, the color of the skin over them is not changed, sharp pain on palpation. The neck muscles are tense. Peripheral lymph nodes - submandibular, anterior cervical and posterior cervical - are palpable, 0.5–1 cm in diameter, elastic, painless. The oral mucosa is clean, pink, the palatine tonsils are hypertrophied, grade II–III, the mouths of the ducts of the parotid salivary glands are gaping and hyperemic. Above the lungs there is a percussion pulmonary sound, auscultation vesicular breathing, RR - 24 per minute. The boundaries of the heart are age-related, the sounds are sonorous, rhythmic, heart rate is 108 per minute. The abdomen is soft, painless, the liver is palpable 2.5 cm below the costal margin, the spleen is at the rib. Stool and urination are not impaired.
Examined: 1. Blood tests during relapses of the disease. 10/11/2005 (4 years): erythrocytes - 3.6 H 1012/l, hemoglobin - 109 g/l, leukocytes - 13.2 H 109/l, eosinophils - 3%, young - 1%, band - 4 %, segmented - 55%, lymphocytes - 31%, monocytes - 5%, plasma cells - 1%, ESR - 32 mm/h, platelets - 250 H 109/l.
2. Blood test dated December 24, 2005 (4 years): erythrocytes - 3.6 × 1012/l, hemoglobin - 120 g/l, leukocytes - 15.8 × 109/l, eosinophils - 4%, basophils - 1 %, band - 4%, segmented - 57%, lymphocytes - 29%, monocytes - 5%, ESR - 20 mm/h.
3. Blood test dated June 16, 2006 (5 years): erythrocytes - 3.6 × 1012/l, hemoglobin - 120 g/l, leukocytes - 11.5 × 109/l, eosinophils - 4%, basophils - 2 %, band - 1%, segmented - 63%, lymphocytes - 23%, monocytes - 7%, ESR - 21 mm/h.
4. Blood test dated 07/07/2007 (6 years): erythrocytes - 4.3 × 1012/l, hemoglobin - 130 g/l, leukocytes - 12.9 × 109/l, eosinophils - 4%, band cells - 4 %, segmented - 55%, lymphocytes - 28%, monocytes - 8%, plasma cells - 1%, ESR - 25 mm/h, platelets - 220 H 109/l.
5. Saliva for DNA by PCR: Epstein - Barr virus (EBV) - detected, cytomegalovirus (CMV) - not detected.
6. IgM, IgG to toxoplasma, chlamydia, cytomegalovirus - not detected.
7. Anti-IgG to EA EBV - detected (++) (antibodies are normally absent); anti-IgG to VCA EBV - 90.3 U/ml (normal antibodies < 3 U/ml); anti-IgG to EBNA EBV - 96.1 U/ml (normal antibodies < 3 U/ml).
8. General urine test - no deviations from the norm.
9. Blood test dated August 17, 2007, within normal limits: total bilirubin - 6.3 µmol/l, indirect - 5.2 µmol/l, AST - 28.6 U/l, ALT - 14.2 U/l , LDH - 402.5 U/l, albumin - 46.6 g/l.
10. Ultrasound of the salivary glands dated August 14, 2007. The parotid salivary glands are enlarged, on the left - 36 x 16 mm, on the right - 33 x 16 mm. The echogenicity of both is reduced (the left one to a greater extent), the contours of the left one are blurred and indistinct. In the right, the process of fibrotization is more pronounced, in the left - edema and dilation of the ducts, and isolated small calcifications. Submandibular and sublingual salivary glands of reduced echogenicity, with compacted interlobular spaces. Conclusion: signs of chronic sialadenitis in the acute stage, more on the left, mainly of the parotid glands.
11. Consulted in the maxillofacial department. Diagnosis: chronic bilateral parenchymal parotitis. Bougienage of the excretory ducts of the parotid salivary glands was performed. A swab was taken for bacterial culture.
12. Culture of saliva obtained from the ducts of the parotid salivary glands: isolated St. aureus 108, sensitive to II–III generation cephalosporins.
Treatment provided: antiviral therapy (Proteflazid, Viferon suppositories, Cycloferon, Valtrex), hyposensitizing therapy (Suprastin, Erius), antibacterial therapy (Medocef, Cebanex), probiotics (Linex, Enterozermina), restorative therapy (vitamins, Imudon), applications with Dimexide on the parotid area, rinsing with antiseptic solutions, bougienage of the excretory ducts of the parotid salivary glands. Proteflazide was prescribed in an age-specific dosage for 3 months, 2 times a year, every 6 months, for 3 years. Suppositories Viferon-1, 2 suppositories 2 times a day, daily No. 10, then every other day for 3 months. A course of cycloferon was administered according to the scheme. In just 3 years, I received 2 courses of Valtrex for 10 days at a dose of 1 g/day. After the therapy, significant positive dynamics were noted. Relapse of the disease was observed after therapy once after rubella, in addition, it occurred without significant intoxication, body temperature did not rise above 37.5 ° C; the enlargement and pain of the gland were less pronounced. Over the past 3 years there have been no relapses of the disease.
Thus, one should remember about the possibility of developing such a rare disease in children as chronic parenchymal sialadenitis (mumps). Knowledge of the clinical picture and features of the course of the disease is very important for timely diagnosis of the disease and the prescription of adequate therapy.
Chronic sialadenitis on ultrasound
Congenital disorders of the development of ducts and glandular tissue, salivary gum disease, as well as autoimmune diseases contribute to the development of a chronic inflammatory process in the salivary glands. Regardless of the cause, there are three stages of chronic inflammation: initial, clinically pronounced and late. In each stage there are periods of exacerbation and remission. In chronic sialadenitis on ultrasound, the parenchyma is hypoechoic, heterogeneous due to point and linear hyperechoic inclusions, the contour is uneven. During the period of exacerbation of large iron, its echogenicity is significantly reduced. During the period of remission, the size of the gland decreases and its echogenicity slightly increases. The decrease in the echogenicity of the gland is due to swelling of the parenchyma and hyperplasia of the intraglandular lymphoid tissue. Hyperechoic inclusions appear when parenchyma is replaced by fibrous tissue. Due to severe fibrosis in the later stages, the iron decreases in size.
| Photo. On ultrasound, the parotid gland on the right (A, B) is enlarged, the parenchyma is hypoechoic, heterogeneous due to small anechoic ovals and linear hyperechoic inclusions. The parotid gland on the left is unchanged. Conclusion: Echo signs of chronic mumps. | ||
| Photo. On ultrasound, the parotid gland is enlarged, the parenchyma is hypoechoic, heterogeneous due to small anechoic foci, point and linear hyperechoic inclusions; the vessels are dilated and blood flow is increased. Conclusion: Echo signs of chronic mumps. | ||
Sjögren's syndrome is a chronic autoimmune disease, predominantly affecting women over 40 years of age, in which lymphocytes and plasma cells intensively infiltrate and destroy the salivary and lacrimal glands. The main complaints of Sjögren's syndrome include dry mouth and keratoconjunctivitis, as well as arthritis. The disease often affects all salivary glands. In Sjögren's syndrome, ultrasound shows that the salivary glands are enlarged, the parenchyma is heterogeneous due to diffusely scattered multiple hypo- or anechoic oval foci; blood flow is usually increased. It is believed that hypo- and anechoic foci are lymphocytic infiltrates against a background of unchanged parenchyma. In the presence of lesions larger than 2 cm and rapid growth, a biopsy is recommended.
| Photo. A 50-year-old man complains of dry mouth and keratoconjunctivitis. On ultrasound, all salivary glands are enlarged, the parenchyma is hypoechoic, heterogeneous due to small hypoechoic foci and linear hyperechoic inclusions. Conclusion: Echo signs of chronic sialadenitis. Diagnosis: Sjögren's syndrome. | ||
A special form of chronic sialadenitis is chronic sclerosing sialadenitis or Küttner's tumor, when a persistent painful tumor appears in one of the salivary glands. This disease is rare and most often affects the submandibular gland. Microscopy reveals atrophy of glandular tissue, dense fibrosis, and periductal lymphocytic infiltrates. Sialoliths and mucus plugs are often found in altered ducts. It remains unclear whether they are a cause or a consequence of the inflammatory process. Some authors suggest that thick secretion blocks small ducts, which leads to inflammation, fibrosis, and atrophy of glandular tissue. Other authors point to the autoimmune nature of the pathology. With Küttner's tumor, ultrasound reveals diffuse parenchymal damage in the salivary gland: multiple round hypoechoic foci. Less common is a focal lesion: a hypoechoic heterogeneous focus against the background of unchanged parenchyma, which simulates a malignant process. In all doubtful cases, a biopsy is recommended. Chronic sclerosing sialadenitis is an exclusively benign inflammatory disease. Often the affected gland has to be removed; no additional treatment is required.
Preparation
Typically, an ultrasound of the salivary glands is preceded by a consultation with a general practitioner. At the initial appointment of a patient with pain symptoms in the glandular area, the doctor examines visually, collects a detailed history and diagnoses using palpation. Next, the patient will be asked to undergo laboratory tests or undergo an ultrasound scan. There is no need to specially prepare for an ultrasound of the salivary glands. It is completely painless and does not cause radiation exposure to the patient’s body. Ultrasound diagnostics are easily tolerated by people of any age. There are only a few recommendations for obtaining a more informative ultrasound examination. Before going to see a specialist, it is recommended to stop eating food 3-4 hours in advance, and to thoroughly clean the oral cavity before performing the diagnosis.
Previous NextSialosis (sialoadenosis) of the salivary glands on ultrasound
Sialosis (sialoadenosis) is a non-inflammatory and non-malignant, recurrent, often painless, usually bilateral enlargement of the salivary glands. The causes of sialosis are unclear. Sialosis occurs in patients with endocrine and autoimmune diseases, liver cirrhosis, chronic alcoholism, vitamin deficiencies, etc. With sialosis, ultrasound reveals enlarged hyperechoic salivary glands, but without focal changes and increased blood flow.
| Photo. On ultrasound, the submandibular (A, B) and parotid (C) glands are enlarged, the parenchyma is hyperechoic, poorly transmits ultrasound waves (the posterior contour of the gland is not visible), homogeneous, the blood flow is not changed. Conclusion: Echo signs of sialoadenosis. | ||
Inflammation of the lymph nodes in the salivary glands on ultrasound
The parotid glands contain a large number of lymph nodes that collect lymph from the upper jaw, lips, mouth, cheeks, outer parts of the nose, upper and lower eyelids, temporal and frontal regions, outer ear and tissues of the parotid-masticatory region. Inflammatory disease in these areas causes a reaction in the lymph nodes of the parotid glands. Inflammation of the intraglandular lymph nodes imitates mumps. Misdiagnosis here is unacceptable, since mumps and lymphadenitis have different management tactics and prognosis.
Important!!! With bacterial lymphadenitis, the infection lymphogenously penetrates into the regional lymph nodes through the “entry gate”. Viral infections hematogenously affect the lymph nodes of several anatomical areas.
Ultrasound with acute serous lymphadenitis within the parotid gland reveals an oval-shaped anechoic formation with clear and slightly wavy contours, often with central blood flow - an inflamed lymph node. Inflammatory edema and infiltration of the tissues surrounding the lymph node (periadenitis) lead to the development of lymphogenous sialadenitis (pseudosialoadenitis). A painful, diffuse swelling appears and the amount of saliva decreases. On ultrasound with lymphogenous sialadenitis, the echogenicity of the parenchyma is reduced, an almost anechoic lymph node is determined; the contour of the lymph node is often not clearly visible, which does not always indicate destruction of its capsule. With a positive outcome, the size of the lymph node decreases, its echogenicity increases, and the contour becomes clearer.
| Photo. Ultrasound of the parotid gland: the echogenicity of the parenchyma is not changed, heterogeneous due to oval-shaped hypoechoic foci with a central scar. Conclusion: Echo signs of reactive lymphadenitis. | ||
Purulent lymphadenitis on ultrasound differs little from acute serous lymphadenitis - an oval-shaped anechoic focus, but as the intensity of the reflected signal increases (GAIN regulator) with purulent melting of the lymph node in the peripheral sections (parietal), point inclusions of medium echogenicity appear, while the central sections the lymph node remains without inclusions. The clarity of the contours and the oval shape indicate the preservation of the capsule of the lymph node during its purulent melting - this is a forming abscess in the salivary gland. An anechoic area of uncertain shape with unclear and uneven contours due to purulent melting of the lymph node and its capsule is adenophlegmon of the salivary gland.
| Photo. On ultrasound, both parotid glands are enlarged, hypoechoic, heterogeneous due to hypo- and anechoic foci. Conclusion: Echo signs of multiple microabscesses. | ||
| Photo. A 2-year-old child with swelling in the parotid region on the right. On ultrasound, the right parotid gland is noticeably enlarged, heterogeneous due to many hypo- and anechoic foci with acoustic enhancement behind and increased blood flow along the periphery. Conclusion: Echo signs of a formed abscess in the parotid gland. | ||
Long-term entry of low-virulent flora into the lymph nodes or inadequate treatment of acute serous lymphadenitis can lead to chronicity of the inflammatory process. An enlarged lymph node in chronic lymphadenitis on ultrasound is hypoechoic, oval in shape with clear contours and (necessarily!) inclusions of high echogenicity in the center. It is the presence of echogenic inclusions in the central parts of the lymph node that confirms the existence of a chronic inflammatory process.
Salivary stone disease on ultrasound
Salivary stones are most often located in the submandibular gland (60-90% of cases) and can be multiple. The parotid glands are affected in 10-20% of cases. Stones can form due to metabolic disorders. Therefore, it is often possible to trace the hereditary nature of the disease. A rather characteristic combination of salivary stone disease and a chronic inflammatory process in the gland.
Sialilithiasis causes partial or complete mechanical obstruction of the salivary duct, which leads to recurrent swelling of the salivary gland during meals and may be complicated by bacterial infection. Sialoliths in the distal submandibular duct can be palpated at the base of the mouth.
Important!!! In preschool children, the role of a calculus can be played by foreign bodies of the submandibular ducts, which enter the ducts through gaping orifices. Such foreign bodies are often toothbrush lint, wood chips from pencils, seed husks, blades of grass, etc.
Calcified stones in the duct of the salivary gland are visible on ultrasound in the form of hyperechoic point or linear inclusions with a pronounced distal acoustic shadow. The duct proximal to the stone is usually dilated.
Only 20% of sialoliths are radiopaque. Uncalcified stones in the salivary gland duct are visible on ultrasound as inclusions of medium or high echogenicity without a distal acoustic shadow. Air bubbles mixed with saliva can mimic stones. An enlarged intraglandular duct indicates the location of the hyperechoic inclusion within the duct, and not in the parenchyma of the gland.
| Photo. Cross section of the parotid gland: 1 - parotid gland, 2 - excretory duct, 3 - stone with an acoustic shadow behind in the distal part of the excretory duct, 4 - masticatory muscle (m. masseter), 5 - ascending arch of the mandible, 6 - buccal muscle ( m. buccinator). | ||
| Photo. A, B — Stones in the excretory duct of the submandibular gland. B - Small stones in the excretory duct of the parotid gland. | ||
| Photo. The parotid gland is enlarged, echogenicity is reduced, somewhat heterogeneous due to small hypoechoic foci, blood flow is increased; the excretory duct is greatly expanded, in the distal section a hyperechoic inclusion with an acoustic shadow behind is determined. Conclusion: dilation of the excretory duct of the parotid gland, echo signs of a calculus in the distal part, secondary parotitis. | ||
Traditional medicine in the treatment of sialadenitis
Drugs from this category really help reduce symptoms, but do not stop the progression of the inflammatory process. Therefore, before using decoctions, you should consult a doctor and do not refuse drug treatment. The most effective in the treatment of sialadenitis are decoctions of:
- chamomile flowers and eucalyptus leaves;
- peppermint leaves and elderflower flowers;
- yarrow and viburnum leaves.
In any case, visiting a doctor is inevitable. You can make an appointment with a specialist on our website.
Salivary gland cysts on ultrasound
Simple cysts are uncommon in the salivary glands. They can be congenital or acquired. Some acquired cysts develop due to obstruction of the salivary ducts in the presence of tumor, stones, or inflammation. Clinically they appear as a painless tumor. On ultrasound, simple cysts are defined as avascular anechoic lesions with a clear contour and posterior acoustic enhancement.
Retention cysts of the sublingual glands are located under the tongue on one side of the frenulum of the tongue: sometimes the cyst displaces the frenulum, but never moves to the opposite side. On palpation, a soft, elastic, painless swelling of a round or oval shape with a smooth, slightly wavy surface is determined. Being covered with a thinned mucous membrane, retention cysts have a characteristic cyanotic or bluish tint. On ultrasound, a small retention cyst (up to 2.0 cm in size) is visible as an anechoic formation, on one side of the frenulum and fibrous septum of the tongue; the outer and anterior contour are not clearly defined, since in these places the cysts are adjacent to the lower jaw. Retention cysts grow slowly. Sometimes they penetrate through the mylohyoid muscle into the submandibular region. If the cyst is large, the wall can be damaged when eating solid food (baking bags, crackers, candies, etc.). If the cyst empties completely, it cannot be detected on ultrasound. The cyst begins to grow again as fluid accumulates in it. In long-term large retention cysts there is often a suspension of medium echogenicity.
| Photo. A — Retention cyst of the sublingual gland. B — Ultrasound shows a simple cyst of the parotid gland. B — Ultrasound shows a complex cyst of the parotid gland. Such cysts require additional research. | ||
4.Treatment
With small sizes and significant mobility of stones, it is sometimes possible to induce their spontaneous evacuation (heating and means of stimulating salivation are used). However, the effectiveness of conservative methods is low and unpredictable. More often the question is raised about surgical removal of the stone or the entire gland as a whole. Considering the abundant vasculature and innervation, as well as the development of irreversible histological changes in the most advanced and advanced cases, such an intervention is always very complex and risky in terms of consequences.
Therefore, you should consult a doctor at the first appearance of the discomfort or pain described above.
Recently, the possibilities of clinical application of alternative high-tech methods (for example, extracorporeal lithotripsy) have been studied, but the methodology is still at the stage of clinical development and is not widely used (at least in Russia). Minimally invasive sialoscopy, a method based on the use of ultra-thin endoscopes with built-in operating manipulators, should apparently be considered the most promising.
Benign tumors of the salivary glands on ultrasound
The most common benign neoplasms of the major salivary glands are polymorphic adenomas and Warthin tumors (adenolymphoma, cystadeniolymphoma). They grow slowly and may be asymptomatic. It is not possible to make a final diagnosis based on ultrasound alone.
Polymorphic adenomas are most common in the parotid gland (60%-90%) in people in the fourth and fifth decades of life, but can occur at any age. Polymorphic adenoma (pleomorphic adenoma, mixed tumor) is a benign tumor with a well-defined fibrous capsule, has slow expansive growth, and is not prone to malignancy, metastasis and relapse. One of the previously existing names for this tumor, fibrochondromyxoepithelioma, indicates that this tumor develops from two germ layers (meso- and ectoderm). Polymorphic adenoma is very diverse and can be represented by both homogeneous dense masses of a grayish color, and mushy masses, areas of mucus with a soft gelatinous consistency, cartilaginous tissues with islands of ossification. Polymorphic adenoma of the salivary glands on ultrasound looks like a round or oval formation of reduced or low echogenicity with a clear, even or coarsely wavy contour. The echogenicity of polymorphic adenoma can be from slightly reduced to low and almost anechoic. The echostructure of the tumor can be homogeneous or contain many pinpoint inclusions of high echogenicity, randomly distributed throughout the tumor, or have large zones with inclusions of medium echogenicity. Blood flow in polymorphic adenoma is often poor or absent, but may be abundant.
| Photo. Polymorphic adenomas of the parotid gland on ultrasound: A - Hypoechoic focus with a wavy contour, almost homogeneous echostructure, blood flow in the center and along the periphery of the focus is increased. B — Hypoechoic focus with a wavy contour, heterogeneous due to hyperechoic foci. B — Hypoechoic focus of lobular structure, heterogeneous due to hyperechoic inclusions. | ||
Important!!! After unsuccessful surgery, polymorphic adenomas can recur multifocally. Untreated pleomorphic adenomas can undergo malignant changes after decades.
Infantile hemangiomas are the most common parotid tumor in infants. Like infantile hemangiomas of other areas, it is benign, appears soon after birth, grows quickly, and spontaneously regresses after 18 months. Surgery is usually not required. On ultrasound, in the projection of the parotid gland, a lobulated hypoechoic formation with a clear contour and extreme vascularization is found.
Warthin's tumor (adenolymphoma, cystadeniolymphoma) accounts for 5-10% of all benign neoplasms of the salivary glands and occurs more often in men in the fifth and sixth decades of life. In 10-60% of cases, Warthin tumors can occur at two or more points, grow and appear at different times. Warthin's tumors are benign; extremely rarely, the epithelial component can undergo malignant transformation. Adenolymphomas consist of a bilayered eosinophilic epithelium and lymphoid stroma. The epithelium forms various glandular and papillary structures: solid, cystic, lobular, papillary. Warthin's tumors on ultrasound are oval, hypoechoic lesions with a clear contour, often containing multiple anechoic areas. Warthin tumors are often hypervascularized but may also contain only short segments of vessels.
| Photo. Warthin tumors on ultrasound. | ||
Cystic lymphangioma occurs from dilated lymphatic vessels when drainage is impaired. Lymphangiomas are not true tumors, but malformations of the lymphatic system. Lymphangioma of the parotid gland is manifested by the presence of an extensive painless formation of soft elastic consistency without clear contours. The color of the skin over the lymphangioma remains normal. Lymphangioma of the parotid gland can extend to adjacent areas (temporal, buccal and submandibular), as well as to the superolateral parts of the neck. Lymphangiomas increase with colds. In this case, the lymphangioma becomes denser and even painful. Inflammation and even suppuration of lymphangioma is often observed, which is accompanied by an increase in volume, thickening, pain that sharply increases with palpation, a change in the color of the skin over the lymphangioma, a local and general increase in temperature. Cystic lymphangioma on ultrasound is visible as an anechoic cavity formation of irregular shape with clear contours, easily changing with pressure. In the lymphangioma cavity, septa are usually visible. The walls of the cysts are relatively thick, up to 1-3 mm, and may contain blood vessels, nerves, and adipose tissue. An inflamed lymphangioma on ultrasound is characterized by greater resistance of the cavity to compression and a convexity of the outer contour, the septa become thicker and more noticeable, and multiple point inclusions appear in the cystic fluid. With hemorrhage, the lymphangioma changes from anechoic to hypoechoic.
| Photo. Cystic lymphangioma. | ||
The parotid gland contains its own veins and transit venous lines - the superficial temporal vein, the mandibular vein, the maxillary vein, therefore, of the hemangiodysplasias in the parotid glands, venous dysplasia or isolated phleboectasis are most common. Venous dysplasia can spread beyond its borders. Large venous nodes located in the subcutaneous tissue and skin create a characteristic clinical picture. Deep venous dysplasia manifests itself as a painless swelling of soft elastic consistency with unclear contours. A characteristic clinical sign of venous dysplasia is an increase in the size of this formation when the child strains or cries, as well as when the head is tilted or in a horizontal position. In a calm state, venous dysplasia on ultrasound is represented by an area of reduced echogenicity of an indeterminate shape with uneven and unclear contours. When performing the Valsalva maneuver, the characteristics of the zone of change change dramatically: its echogenicity decreases, its contours become clearer, and its shape becomes more rounded. This technique allows you to confidently differentiate venous dysplasia from all other diseases of the parotid gland.