Kinds
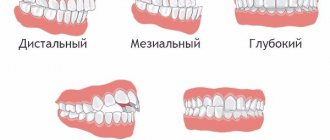
The concept of incisal disocclusion includes several causes of bite defects:
– lack of contact between the incisors due to abrasion of the enamel, changes in the angle of the tooth (sagittal disocclusion);
– contact of the incisal antagonists of both jaws with cutting edges (direct occlusion);
– advancement of the lower incisors forward while maintaining frontal contact of the lower and upper dentition (reverse occlusion);
– forward displacement of the mandibular incisors does not allow close contact with antagonists (reverse disocclusion);
– displacement of the upper incisors forward, lack of contact with the incisors of the lower jaw (vertical disocclusion);
– more than a third, overlap of incisors with antagonists (deep occlusion);
– the above defect, but with an open gap (deep disocclusion).
Edentia of the incisors due to trauma is called false incisor disocclusion.
Correction of distal occlusion using microimplants
M. M. Solomonyuk
Ph.D., orthodontist, Exline clinic (Kyiv, Ukraine)
Historically, views on orthodontic treatment with or without extraction of individual teeth have changed many times [1]. During Edward Engle's time, orthodontic treatment was primarily non-extraction. However, the lack of stable support during orthodontic treatment often had a negative impact on the facial profile [2].
Charles Tweed proposed a new treatment technique based on the principles of anchorage due to the distal inclination of the lateral teeth. Using cephalometric analysis, he justified the need for premolar removal based on the diagnostic triangle [3].
Currently, the need to preserve teeth, especially first premolars, during orthodontic treatment is being actively discussed. A number of researchers have introduced the concept of functional occlusion, based on the principles of gnathology. They consider the removal of premolars during orthodontic treatment unacceptable, since this leads to an imbalance in the functioning of the masticatory apparatus and can be a trigger for the development of TMJ dysfunction [4].
Among the non-extraction methods of treating orthodontic anomalies, the most common is distalization [5].
One of the very first devices for distalization was Headgear. However, wearing the latter as a method of treatment is rejected by many patients due to aesthetic and social considerations and requires full responsibility in wearing the device for at least 18 hours a day [6]. Of the majority of intraoral distalization devices, the Pendulum and its modifications are the most common. However, the need for laboratory stages for the manufacture of the device and the duration of the treatment stages served as prerequisites for the creation of other systems [7].
We propose a method of moving the upper dentition using microimplants and sliding mechanics.
A 21-year-old patient came to the clinic with complaints of an unattractive smile and crowded teeth (Fig. 1). On external examination: the face is symmetrical, proportional, mesiocephalic type. The profile is convex, lips are not closed at rest, breathing is mixed. Moderate chin and nasolabial folds.
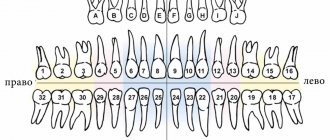
Intraoral examination revealed a molar relationship in Angle class II, complicated by deep incisal occlusion. When analyzing the models, crowding was observed in the upper dentition - 7 mm, in the lower - 5 mm.
The orthopantomogram did not reveal any resorption or inflammatory phenomena. Endodontic treatment of tooth 46 and retention of third molars 18, 28, 48 are required.
Interpretation of the lateral teleroentgenogram (TRG) before treatment revealed skeletal class I, angle ANB - 4º, angles SNA - 79º, SNB - 75º, mandibular angle FMA (angle between the Frankfurt and mandibular planes 27º; Table No. 1). The position of the upper incisors U1 to FH (the angle formed by the axis of the upper central incisors U1 to the Frankfort horizontal FH) is 109°. The ratio of the lower central incisors - IMPA (the angle between the axis of the lower central incisors and the mandibular plane) - corresponds to 105°. The angle of inclination of the occlusal plane to the Frankfurt horizontal is below average values (FH to Occ P 18°). The symmetrical position of the anterior facial height in relation to the posterior one—index PFH/AFH—0.7 (Fig. 2).
Based on the data of clinical examinations, anthropometric examination of jaw models, the use of additional special research methods - TRG in the lateral projection and orthopantomogram - a diagnosis was made: permanent dentition, Engle class II, complicated by deep incisal occlusion, crowding of teeth in the frontal region on the upper and lower teeth arch II degree, skeletal class I.
The treatment steps necessary to correct the identified pathology were as follows:
- Sanitation of the oral cavity.
- Elimination of crowding in the upper and lower dental arches.
- Normalization of the sagittal and vertical relationship of the upper and lower central incisors.
- Correction of deep incisal occlusion.
- Improvement of the facial profile.
- Establishing the relationship on the canines and molars according to Angle’s class I when achieving functional occlusion.
To solve the problems, the patient was offered several treatment options. The first option involved the extraction of premolars on the upper and lower jaws. The patient categorically refused to remove the premolars.
The second alternative treatment plan is to move the upper teeth supported by microimplants and extract impacted lower wisdom teeth. The patient agreed to this treatment plan.
A non-removable "Roth script" hardware with a 0.22-inch groove was installed and fixed with a primary nickel-titanium (Ni-Ti) archwire measuring 0.14 inches, then 0.16 and 0.16-0.25 inches. After aligning the dentition, a 0.19-0.25 inch steel archwire was installed on the upper and lower dentition brackets. To create absolute support, 2 microimplants (1.3 mm thick and 8 mm long, Dentos AbsoAnchor (Korea)) were installed in the interroot space between the second premolars and first molars on the upper jaw in a diagonal direction at an angle of 60° to the bone surface. Hooks are soldered onto the upper steel arch between the lateral and central incisors. To move the upper teeth, closing nitinol springs are installed from the head of the microimplant to the soldered hooks on the arch with a force of 250 mg each (Fig. 3).
(Fig. 1a) (Fig. 1b) (Fig. 1c)
(Fig. 1d) (Fig. 1e) (Fig. 1f)
(Fig. 1g) (Fig. 1h)
Rice. 1. Photos of the patient before treatment.
The closure springs were removed once the Angle class I molar relationship was achieved.
To prevent the effect of wedging of teeth due to distal movement of the molars, increasing the intermaxillary angle FMA, rotation of the occlusal plane and opening of the bite, the posterior teeth were intruded using an elastic chain with a force of 150 g, fixing it from the heads of microscrews around the arch in the area of the second premolars and first molars.
Treatment results
Fixed equipment was removed 15 months after the start of treatment. Analysis of facial photographs revealed a noticeable improvement in the facial profile. On intraoral photographs, the dental arches are aligned (Fig. 4). Analysis of the models showed average values of the sagittal and vertical ratios of the incisors. The relationship of the dentition was according to Engle's class I, the midline on the upper and lower dentition coincided. When diagnosing the articulator at rest, tight intertubercular contact between the dentition, the absence of premature contacts during lateral movements of the lower jaw, frontal guidance and canine guidance on both sides were revealed.
Cephalometric analysis showed a decrease in the angle FMA, FH to Occ P. An increase in SNB, Z-angle. The PFH/AFH index was 0.8.
On the orthopantomogram, the roots of the teeth are parallel, there is no resorption (Fig. 5). Microimplants provided complete anchorage during distal movement of teeth; no symptoms of mobility or loss were observed during treatment.
After 1 year of retention, there was no relapse during clinical examination, and stability of the previously obtained results was observed. The relationship between the canines and molars was according to Angle's class I. There was no crowding of teeth in the frontal area on the upper and lower dentition, and no symptoms from the temporomandibular joint (Fig. 6).
(Fig. 2a) (Fig. 2b)
Rice. 2. Teleradiography before and after treatment.
Analysis and discussion
Moving the upper posterior teeth using microimplants using sliding mechanics provides maximum mechanical advantages compared to traditional methods. There is no need for preliminary use of a distalizing device: treatment begins directly with the installation of a fixed system.
The main successful factor for orthodontic treatment is the choice of support, or anchorage. In this clinical case, microimplants were used for stable support. Their use is most preferable due to the ease of installation, minimal anatomical restrictions when screwing in, there is no wait for the period of osseointegration, and there is the possibility of direct loading after installation. For stable support in the bone tissue throughout the entire treatment period, it is very important to choose the correct length, diameter and installation location. The choice of microimplant diameter will depend on the width of the interroot space, determined on a periapical contact x-ray or computed tomography fragment. If there is sufficient space, it is recommended to install a microimplant of at least 1.5 mm in the upper and lower jaws. If the space is limited by the proximity of the roots, screw in a minimum diameter of 1.2-1.3 mm.
(Fig. 3a) (Fig. 3b) (Fig. 3c)
(Fig. 3d) (Fig. 3e)
Rice. 3. Two microimplants were installed on the upper jaw.
The length will not be critical since the main fixation occurs between the microimplant and the cortical bone. However, on the upper jaw it is set at least 6 mm, on the lower jaw - 5 mm.
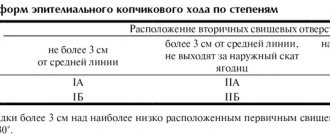
Table 1. Cephalometric indicators
| Cephalometric angles (°) | Average values | Before treatment | After treatment |
| SNA | 82 | 79 | 79 |
| SNB | 80 | 75 | 77 |
| ANB | 2 | 4 | 2 |
| F.M.A. | 25 | 27 | 23 |
| PFH/AFH | 0,8 | 0,7 | 0,8 |
| FH to Occ P | 10 | 18 | 12 |
| Ui to FH | 114 | 109 | 118 |
| I.M.P.A. | 90 | 105 | 105 |
| Z-angle | 75 | 75 | 80 |
The microimplant is best inserted in an oblique direction at an angle of 30-60º to the bone surface. This direction reduces the risk of root damage during installation. It is covered by a larger volume of cortical bone, which increases the adhesion force to the bone. It is better to install microimplants in the area of the attached gum from the edge at 6-8 mm. This allows good access to the microscrew head for various thrust options.
(Fig. 4a) (Fig. 4b) (Fig. 4c)
(Fig. 4d) (Fig. 4e) (Fig. 4f)
(Fig. 4g) (Fig. 4h)
Rice. 4. Photo of the patient after treatment.
(Fig. 5a) (Fig. 5b)
Rice. 5. Orthopantomogram before and after treatment.
(Fig. 6a) (Fig. 6b) (Fig. 6c)
(Fig. 6d) (Fig. 6e) (Fig. 6f)
(Fig. 6g) (Fig. 6h)
Rice. 6. Photo of the patient after treatment.
conclusions
- The use of support on microimplants allows the movement of molars without loss of anchorage in the sagittal, horizontal and vertical planes.
- The most stable effect is observed in patients with low FMA.
- Crowding of the dental arch greater than 7 mm, high IMPA and FMA can serve as indications for the removal of individual teeth.
- For stable support on the upper jaw, it is necessary to install a microimplant with a length of at least 8 mm.
- The success of microimplantation depends on the patient’s bone tissue density, the clinical skills of the orthodontist, the differential diagnostic stages performed, the choice of location and direction of microimplant placement, and oral hygiene.
Causes
The root causes of incisor malocclusion are the following factors:
- heredity, including chromosomal mutations;
- increase in size of the tongue (macroglossia);
- short frenulum of the tongue, lips;
- habits that prevent the correct formation of occlusion (thumb sucking, lip biting, etc.);
- breathing through the mouth due to rhinitis, adenoids and other ENT diseases;
- incorrect position of the tongue in the oral cavity;
- advanced caries of incisors;
- hypovitaminosis, metabolic disorders (including mineral), osteomyelitis, rickets, etc.;
- weakened immunity.
Causes of open bite
One of the most common reasons is the presence of bad habits in children. For example, such as: using a pacifier for a long time, placing the tongue between the teeth, sucking a finger or pencil.
A bad habit is putting your tongue between your teeth.
A bad habit is thumb sucking.
And it seems difficult to argue with this. Because mechanical impact on the dentition, of course, can lead to vertical disocclusion. But! This is a very superficial look at the cause of open bite. After all, thumb sucking and tongue thrusting are more likely a consequence than a cause.
And the cause of vertical disocclusion is always cranial problems (see “Cranial distortions”), that is, problems with the position of the cranial bones. And the resulting cranial dysfunctions are always reflected in the jaws (from which the teeth “grow,” as is known).
Treatment in installments
The Orto-Artel clinic offers installments for the entire process of treating any disease. Personal conditions are considered on an individual basis.
Find out more
or call 8 (495) 128-11-74
This is confirmed by thumb sucking in the womb. What bad habit are we talking about here? A bad habit is something acquired, something that appears throughout life. And thumb sucking while still in the mother’s womb is a subconscious act by which the child unconsciously tries to ensure the stability of the cranial bones. Thus ensuring the functionality of the cranio-sacral mechanism (for those who don’t know what it is, look at Wikipedia). After all, this mechanism is the most important factor ensuring the normal functioning of the central nervous system (CNS). That is, the main “computer” of the entire organism, regulating every single process taking place in it. And that is why every effort is being made to ensure the stability of this “computer”. Even in such a simple way as thumb sucking.
- Thumb sucking in utero during an ultrasound examination.
- Thumb sucking in early childhood, as a continuation of point 1.
- The figure clearly shows how the child unconsciously stabilizes the entire maxillary complex and adjacent cranial bones.
- As a consequence of cranial problems and “bad habits”.
As we see, tongue protrusion simply cannot but occur with such a vertical “gap” between the upper and lower teeth.
The tongue is too “curious” an organ to ignore such a tempting “hole”. And accordingly, tongue insertion, as well as insertion of other objects (including fingers and pencils), only aggravates the problem. That is, it is a “related product”.
Diagnostics
The dentist diagnoses incisal disocclusion visually and prescribes detailed diagnostics to understand the causes of the pathology:
– radiography of the frontal zone, revealing impacted units and other abnormalities of the mucous or bone tissue;
– orthopantomogram demonstrating the condition of the dentition;
– photographs of the patient’s frontal view and profile for anthropometric measurements;
– casts of the dentofacial apparatus for making a model.
The size and extent of the gap space between the dentition, which demonstrate the severity of disocclusion, are also important.
Crossbite
Characterized by atypical (reverse) closure of the anterior or lateral or both the first and second teeth together with simultaneous deviation of closure in the left or right area of the bite. A double form of this bite is possible.
If professional treatment and care are not provided, patients with transverse bite experience facial distortions and serious changes in appearance, as the jaw bones develop asymmetrically. Characterized by chewing dysfunction and difficulties with pronunciation. Often patients with this bite suffer from biting the mucous membranes of the cheeks, tongue, and lips.