A lactating woman should limit herself in many ways. This applies to nutrition, lifestyle, and physical activity. Medications are especially prohibited for nursing mothers due to possible negative effects on the newborn. But sometimes when headache, dental, muscle or joint pain occurs, it is impossible to do without an analgesic.
Ketonal is a non-steroidal anti-inflammatory drug that relieves pain in musculoskeletal diseases and other types of pain syndrome. An effective drug eliminates the inflammatory process and reduces fever.
Basic information
Dosage forms and composition of Ketonal:
1.Injection liquid:
- ketoprofen;
- propylene glycol;
- ethyl and benzyl alcohol;
- sterile liquid.
2.Cream:
- ketoprofen;
- propylhydroxybenzoate;
- preservative E218;
- myristanoic acid isopropyl ester;
- petrolatum;
- propylene glycol;
- glyceryl oleate;
- elfakos;
- magnesium sulfate;
- distilled water.
3.Gel:
- ketoprofen;
- triethanolamine;
- carbomer;
- water;
- ethanol;
- lavender oil.
4. Rectal suppositories:
- ketoprofen;
- solid fat;
- miglyol 812n.
5. Enteric-coated tablets:
- ketoprofen;
- magnesium sterol;
- pyrogenic silicon dioxide;
- crospovidone;
- starch;
- talc;
- lactose.
6.Extended release tablets:
- ketoprofen;
- magnesium stearate;
- pyrogenic silicon dioxide;
- crospovidone;
- MCC;
- hypromellose.
Thanks to the action of its components, Ketonal eliminates the inflammatory process, relieves pain, and reduces fever. Ketoprofen inhibits the synthesis of bradykinin (polypeptide), stabilizes lysosome membranes, and inhibits the release of enzymes that destroy tissue during the inflammatory process. As a result, the patient's pain threshold increases.
Ketonal is used to eliminate symptoms of inflammatory diseases of the musculoskeletal system and relieve pain of various origins.
Indications for the use of liquid for injections, tablets and rectal suppositories:
- Rheumatoid arthritis;
- Ankylosing spondylitis;
- Inflammatory joint damage in psoriasis;
- Arthropathy;
- Deposition of urates (uric acid salts) in the joints;
- Pyrophosphate gout;
- Degenerative-dystrophic changes in joints and bone formations;
- Inflammation of the mucous bursae of the shoulder, knee, elbow joints;
- Tendon inflammation;
- Damage to the peripheral nerve, which is accompanied by severe pain;
- Muscle pain;
- Radiculitis;
- Headache;
- Inflammation of the nerve roots in the spinal cord;
- Pain after injury or surgery;
- Pain syndrome in oncology;
- Painful menstruation;
- Inflammation of organs in the pelvis.
Indications for use of gel and cream:
- Injuries of the musculoskeletal system (bruises, sprains, ruptures);
- Autoimmune inflammation of connective tissues with predominant damage to joints;
- Inflammation of periarticular tissues;
- Ankylosing spondylitis;
- Psoriatic arthritis;
- Arthropathy;
- Tendon inflammation;
- Muscle pain;
- Radiculitis;
- Osteoarthritis.
Before using Ketonal, consult your doctor.
Dosage
The drug in the form of a cream is used to treat the skin on the affected area. A thin layer is applied twice or three times a day. The gel is used in the same way as the cream, but not more than 2 times a day. Therapy lasts about 14 days; if necessary, the doctor will increase the duration of the course.
Liquid for injection is injected into a muscle or vein - 1 ampoule 1 or 2 times in 24 hours.
Infusion administration (intravenous infusion) is carried out only in a hospital. The maximum daily dose of the drug is 200 mg.
The daily dosage of rectal suppositories is 1 or 2 pieces.
The drug in tablet form is taken orally before or after meals with filtered water (100 ml).
Daily dose of tablets:
- Enteric-coated tablets - 1 piece twice.
- Extended-release tablets – 1 piece once.
The final dosage and frequency of administration will be determined by the attending physician.
Precautionary measures
Ketonal, like any medicine, has a number of contraindications:
- Hypersensitivity to main or excipients;
- Aspirin asthma;
- Ulcer;
- Ulcerative colitis;
- Diverticulosis;
- Chronic inflammation of all parts of the gastrointestinal tract;
- Impaired hemostasis;
- Chronic kidney diseases.
As stated in the instructions, Ketonal is prohibited for children under 14 years of age, pregnant and nursing mothers.
Under the supervision of a doctor, people suffering from bronchial asthma, anemia, alcoholism, and cirrhosis take the drug. This limitation applies to patients with functional insufficiency of the liver, kidneys, diabetes mellitus, and hypertension. Use the drug with caution for edema, stomatitis, and blood diseases.
Sometimes side effects occur after taking the medication:
- epigastric pain, nausea, vomiting, stomatitis, etc.;
- headache, irritability, sleep and speech disorders;
- hypertension, increased heart rate;
- disturbances of vision, hearing or taste;
- rash, shortness of breath, runny nose, Quincke's edema.
If the above or other symptoms appear, stop taking the drug and consult a doctor.
ketonal during breastfeeding
Compatibility can be viewed here:
1.https://www.e-lactancia.org/ingles/inicio. On the website, drugs are divided into four categories (they assess the risk for lactation and for the child together): 0 - safe 1 - relatively safe: side effects in the child are possible, but they are rare and not very strong. 2 – quite dangerous: there is a possibility of moderate consequences for the child. 3 – very dangerous, do not use during feeding. how to use this guide is here
2. WHO/UNICEF “Breastfeeding and maternal drug treatment” (WHO/CDR 95.11)
3. Use of anti-infective chemotherapy drugs during pregnancy and breastfeeding –
4. a table that brings together the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale: The table is not too large, but the most common things are there. Feeding categories: L1 – safest. The drug has been taken by large numbers of nursing mothers with no observed harm to infants. There is extensive research available. L2 – safe. There are limited studies showing no negative effects on infants AND/OR negative effects are possible but very unlikely. L3 – relatively safe. Studies have shown the possibility of mild side effects for the child. L4 – possibly dangerous Studies in breastfeeding women have shown an increased risk to the baby, but use may be justified by a threat to the life of the mother. L5 – contraindicated when breastfeeding Studies have shown a serious, confirmed risk to the child.
5.
6.https://www.gvinfo.ru/?q=node/112 compatibility of herbs for breastfeeding (in English)
If your drug is not here, then call us and we will look it up in the reference books.
“Often a situation arises when the official instructions for a drug prohibit its use during lactation, but in fact it is safe for both mother and child. Why is this happening? The fact is that the procedure for registering a drug and allowing it to enter the market does not include mandatory clinical trials of its safety for nursing mothers and breastfed infants. Simply put, such tests are carried out only voluntarily by the manufacturer, which happens extremely rarely, due to the high cost of these procedures. Only separate studies are carried out for adults, separately for children, but breast milk, penetration of the drug and its effect on the child are not tested. Sometimes the instructions describe a situation where a medicine is allowed for infants in the first months of life in its pure form, but is prohibited during lactation, because tests have simply not been carried out. And in the absence of research results, the manufacturer has the right to write only one wording - “prohibited during lactation.” However, there are well-funded third-party independent organizations, such as WHO, AARP and others, that conduct full trials of the use of drugs during lactation, and provide their opinions on their safety and compatibility with breastfeeding. According to these results, there are much more commonly used drugs compatible with breastfeeding than prohibited ones (including antibiotics). Specialized reference books are being compiled, which can be used to check the compatibility of the drug and breastfeeding.”(https://www.detskydoctor.ru/news/2010-04-13-57)
1. Gels for stretch marks on the chest are possible, but not all. Only those that position themselves as gels for stretch marks for nursing and pregnant women. For example, Mustela.
2. Rifampicin According to the Russian manual, it is not compatible. Hale Software (international reference) - L2 (safe. There are limited studies that show no adverse effects in infants AND/OR adverse effects are possible but very unlikely.)
3. According to the Russian reference book, Rovamycin is not compatible with hepatitis B. During e-lactation, it is released into milk in extremely low concentrations, risk level 1
4.Spazmolgon is compatible with guards.
5. Nurofen is compatible with gw
6. finalgon - I do not have data on this drug. so I can’t say how compatible it is with Guards. finalgon does not pass into breast milk, but there is not enough experience with its use in nursing mothers, so the manufacturer advises using this drug with caution during breastfeeding.
7. pimafucort cream and contractubex - compatible with gw
8. Scandanest - There is no such thing in the drug compatibility guides. But in its annotation it is written - With caution during breastfeeding (there is no data on penetration into breast milk). Dentists have a large number of drugs that are not in reference books. They themselves usually look at the compatibility according to the annotation.
9.nimesil - Nimesil, Nise - active ingredient - Nimesulide (Nimesulide) On e-lactancia: risk 1 - moderately safe. to replace: Ibuprofen, Diclofenac maximum concentration - after 2.8 hours half-life - after 4.7 hours Note: Drug control authorities in Spain have withdrawn all non-mesulide-containing drugs due to high toxicity and a large number of complications on the liver. Period of complete elimination Instructions: excreted from the body mainly in the urine, about 98% of the dose is eliminated within 24 hours. With prolonged therapy, accumulation of nimesulide is not observed. Other sources: complete elimination period – 12 hours. (The effectiveness of nimesulide in the treatment of dorsopathies M.N. Sharov, O.N. Fishchenko)
10. Monural – according to Hale L3 – i.e. relatively safe. Studies have shown the possibility of mild side effects for the child. According to the annotation, its half-life is 4 hours. So in half a day it will no longer be in the milk..
11. Citramon - Currently, the name Citramon does not correspond to any specific composition of the drug, but rather is a reminder to patients of the nature of the action of the drug, which has long become a familiar “brand” in the countries of the former USSR.
Traditional Citramon (Tabulettae "Citramonum") had the following composition: acetylsalicylic acid 0.24 g, phenacetin 0.18 g, caffeine 0.03 g, cocoa 0.015 g, citric acid 0.02 g. A drug with this composition is no longer available released.
New forms of these drugs with the word “Citramon” in the name are produced by a very large number of pharmaceutical companies. Most often they have the composition “acetylsalicylic acid (aspirin) + caffeine + paracetamol” (the drugs “Citramon P”, “Aquacitramon”, “Citramon-Acri”, “Citramon-Borimed”, “Citramon-MFF”, etc.) are registered with this composition .d.).
If the composition contains aspirin, it can be used only once... Aspirin is not compatible with hepatitis B.
12.Ketarol - according to Hale L2
13. Magne B6 = magnesium lactate (not found on e-lactancia, there are other magnesium compounds, all with risk 0) + pyridoxine (Pyridoxine) Pyridoxine is a vitamin risk level 1 Avoid daily doses above 25 mg. Higher doses may reduce lactation by blocking the release of prolactin. With a balanced, comprehensive diet, there is no need to take vitamins.
13. trichopolum (metronidazole) According to Hale, the risk is L2, that is, you can feed, it is quite safe. half-life time – 8.5 hours, full withdrawal time – 25-75 hours. On e-lactancia - RISK 0 here Since a large amount of this medicine passes into the child’s blood, its use is theoretically contraindicated. As an alternative to weaning the baby, it is recommended to give the mother one dose (2 g) and interrupt breastfeeding for only 24 hours. In “Breastfeeding and Maternal Drug Treatment” (WHO): “if possible, do not prescribe. If a single dose of 2 grams is prescribed, it is advisable to interrupt feeding for 12 hours.” here it’s worth it, yes, to feed. According to Hale, the risk is L2, that is, you can feed, it is quite safe. half-life time – 8.5 hours, full withdrawal time – 25-75 hours.
14. Ultracaine (articaine) it says that it is possible - the risk is 0... And in the WHO reference book it is compatible with breastfeeding
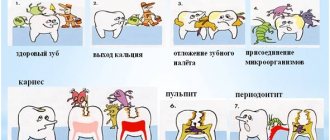
Dental treatment is compatible with breastfeeding; most local anesthetics used in dental treatment are allowed during breastfeeding.
15. List of common drugs for anesthesia: articaine group (astracaine, ultracaine, septocaine) - benzocaine is allowed - bupivacaine is allowed (Marcaine, Macaine) - cincocaine (dibucaine, nupercaine) is allowed - the first degree of risk out of four, do not apply to the chest mepivacaine - the first degree of risk, do not smear pramocaine on the chest - allowed, do not smear procaine on the chest - first degree of risk, do not smear tetracaine on the chest - allowed, do not smear it on the chest
15.detralex and chimes - compatible with gw
16. Suprastin - Chloropyramine - not found in international databases, according to domestic data it is prohibited during lactation.
17. Preparations with the active ingredient cetirizine (trade names Reactin, Allertek, Zyrtec, Zodak, Cetrin) - for E-lactation the risk is zero, according to Hale it is quite safe (L2), the pediatric note states that no cases of complications in children have been reported , but sedation is possible. But according to domestic data, the medicine has contraindications for lactation.
18. Preparations with the active ingredient loratadine (trade names Vero-Loratadine, Claritin, Clarfast, Loradin, Lorid, Erolin) - E-lactation risk 0, according to Hale is completely safe (risk L1), the pediatric note indicates that cases of complications with Children have not been reported, but dry mouth and rapid heartbeat are possible. But according to domestic data, the medicine has contraindications for lactation.
19.Erius, active substance desloratadine, risk 0, according to Hale, not transmitted with milk. But according to domestic data, the medicine has contraindications for lactation.
20.sulfacyl-sodium (eye drops) compatible with hepatitis B
21. Diazolin – I couldn’t find it in the reference books, but the manufacturer lists GV as a contraindication.
22. potassium iodide - “do not prescribe during breastfeeding” from the WHO manual “Breastfeeding and maternal drug treatment: recommendations for the use of drugs included in the pharmacopoeia” iodine - “compatible with breastfeeding in doses of nutritional supplements and standard treatment for mothers with deficiency Yoda. If possible, do not prescribe topical and general medications containing iodine for other purposes.”
23.cefotaxime is classified as safe in pregnancy by the AAP (American Academy of Pediatrics) and while breastfeeding by Dr. Hale (safe. There are limited studies that have not shown a negative effect on infants AND/OR a negative effect is possible, but very unlikely. ) - according to the Russian reference book (authors Karpov, Zaitsev) - compatible with Guards. - according to the reference book of the Spanish hospital Marina Alta - https://www.e-lactancia.org/ingles/inicio.asp - risk 0 (safe)
24. Acyclovir and Valtrex - according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale - L2 ( safe. There are limited studies that have not shown a negative effect on infants AND / OR a negative effect is possible, but very unlikely.)
25. Aloe extract liquid for injection is compatible with gv.
26.ruzam - This drug is not in international reference books, because This is a Russian drug. But in its annotation there are no contraindications for GV. This means that the manufacturer allows it.
27.Suprax (cefixime) – compatible with guards, according to Hale L2
28. Amoxiclav (augmentin) – compatible with guards, Hale software L1
29. Azithromycin (sumamed) is classified in pregnancy by the AAP (American Academy of Pediatrics) and in breastfeeding by Dr. Hale - L2 (safe. There are limited studies that have not shown a negative effect on infants AND/OR a negative effect is possible, but very unlikely.) According to the reference book of the Spanish hospital Marina Alta https://www.e-lactancia.org it has a risk of 0 (Safe for lactation and for the child. Compatible with breastfeeding, based on information published in the scientific literature. Can be taken.)
30. terzhinan – It’s not in my reference books, but I read in the instructions “It is possible to use Terzhinan during pregnancy and lactation (breastfeeding) according to indications.”... In Vidal’s reference book it’s the same…. Here is more information on it: Terzhinan is a complex antibacterial and antifungal drug for the treatment of gynecological diseases. Ternidazole is active against anaerobic flora, including gardnerella, and also has a trichomonacid effect. Neomycin sulfate is an aminoglycoside antibiotic that acts on pyogenic bacteria of the vagina. Nystatin is a polyene antifungal agent that is active against fungi of the genus Candida. Prednisolone sodium metasulfobenzoate is a corticosteroid with a local anti-inflammatory effect. The most incompatible with breastfeeding are tinidazole and ternidazole. On the Hale forum about them: Tinidazole tinidazole and Metronidazole metrodinazole He writes that his book describes in detail the use of metrodinazole for treatment, that it is quite safe and the mother can continue breastfeeding, refers to the AAP. Quote: “she does not need to stop breastfeeding. While Flagyl(metronidazole) does enter milk in moderately low amounts, it is very non toxic and is often given to children for similar infections. „ (mother is prescribed 3 doses every other day of 500 mg, baby is 30 days old) Translation: “She should not stop breastfeeding. Flagyl(metronidazole) appears in milk in fairly low concentrations, is very non-toxic, and is often used to treat children with similar infections.” Hence: The only thing that can change the taste of milk (Hale writes) is that a metallic taste may appear, which the child may not like. Regarding tinidazole, he writes that the concentration and effect are comparable to metrodinazole and can be used by nursing mothers.
31. Cycloferon - not compatible with hepatitis B, but can be replaced with Viferon, which is possible with hepatitis B.
32. Hexoral (hexetidine) – compatible with guards.
33. cromoglin according to Karpov’s reference book - cromoglin is compatible.
34. Flexonase - According to the Russian reference book, it is compatible, as well as according to the instructions. But according to Hale it is L3 (see above), according to the reference book of the Spanish hospital Marina Alta https://www.e-lactancia.org - risk 1 (relatively safe: side effects are possible in the child, but they are rare and not very strong)
35. Finistil - compatible with guards
36.rapidol (paracetamol) - compatible with guards.
37. Magnesia - compatible with guards.
38. Ospamox (Amoxicillin) - compatible with guards.
39. Chondroxide according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale L3 is relatively safe. Studies have shown the possibility of not very strong side effects for the child. According to the reference book of the Spanish hospital Marina Alta https://www. e-lactancia.org it has a risk of 0 (Safe for lactation and for the baby. Compatible with breastfeeding, based on information published in the scientific literature. Can be taken.)
40.Milgamma - With a daily dose of vitamins B6 up to 25 mg, there are no contraindications for use during pregnancy and breastfeeding. Dragees and solution contain 100 mg of the drug, and therefore are not recommended for use in these cases.
41. Tafen nasal according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale L3 is relatively safe. Studies have shown the possibility of not very strong side effects for the child. although according to the reference book of the Spanish hospital Marina Alta https://www.e-lactancia.org it has a risk of 0 (Safe for lactation and for the child. Compatible with breastfeeding, based on information published in the scientific literature. Can be taken.) But here is the Russian reference book (author Zaitsev) - does not allow it under Guards.
42. Lecrolin - not in my reference books, but in the annotation it is allowed, albeit with caution. 43.voltaren - L2 - according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale - L2 ( safe. There are limited studies that have not shown a negative effect on infants AND / OR a negative effect is possible, but very unlikely.)
44. but spa - L2 - according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale - L2 ( safe. There are limited studies that have not shown a negative effect on infants AND / OR a negative effect is possible, but very unlikely.) 45. combilipen - not in the reference books, but in its instructions gv is contraindicated.
46. Flemoxin soblutab - compatible with giv
47. “Cough tablets” (with thermopsis) - not compatible with guards. There is a risk of developing respiratory depression in a child due to the fact that it contains codeine.
48.mucoltin – compatible with gv
49.Polydex with phenylephydrine – In its instructions – “Contraindicated during pregnancy and breastfeeding” I tried to disassemble it into components and check each of them and this is what I found - phenylephidrine according to classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale L3 (relatively safe. Studies have shown the possibility of not very strong side effects for the child.) So. its use is not advisable. And according to Risk Level 1 (relatively safe: side effects in a child are possible, but they are rare and not very strong.) Neomycin- www.e-lactancia.org- Risk 0 Dexamethasone - according to Hale L3, according to www.e-lactancia.org - Risk 1 The compatibility of another component, polymyxin, was not found anywhere.
50.valerian, motherwort, phenibut, Novo-passit, neurohel – compatible with gv
51. Enterofuril – Active ingredient Nifuroxazide. in the instructions: Special instructions: Before prescribing the suspension to infants, it is necessary to exclude congenital deficiency of enzymes that break down sucrose. Can be prescribed to pregnant and lactating women. Ethanol intake may cause hypersensitivity symptoms. It is not absorbed in the gastrointestinal tract, so it can be used during feeding (
52.chophytol On e-lactancia risk 1 - relatively safe: side effects are possible in a child, but they are rare and not very strong. According to the Russian reference book - compatible
53. NEUROMIDIN and NEUROMULTIVIT In the reference books on the compatibility of drugs (Karpov, Heile, and there is no data on these drugs. And in their instructions it is written: NEUROMIDIN - Contraindicated during breastfeeding. - Due to limited experience with the use of NEUROMULTIVIT, it is not recommended to prescribe it during pregnancy and breastfeeding But on the Hale forum this is what is written (https://neonatal.ttuhsc.edu/discus/messages/60/4487.html?1233929012): pyridoxine is dangerous from the group of B vitamins in a dosage greater than 300 mg/day. In neuromultivitis - 200 in one tablet, if the mother drinks no more than 1 tablet per day, then it’s compatible, it turns out.
44. Pentalgin – not compatible with Guards.
45. neo penotran = Metronidazole + Miconazole both drugs - according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale - L2 (safe. There are limited studies that have not shown a negative effect on infants AND/OR negative exposure is possible, but very unlikely.) On e-lactancia-0 - it’s safe so you can feed with it.
46. According to the instructions, the composition of fastum gel is Ketoprofen. According to the classification during pregnancy from the AAP (American Academy of Pediatrics) and when breastfeeding from Dr. Hale, it belongs to group L3 (relatively safe. Studies have shown the possibility of not very strong side effects for the child.) Thus. its use is not advisable. And Voltaren according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale is L2 (safe. There are limited studies that have not shown a negative effect on infants AND/OR a negative effect is possible, but very unlikely.)
47. Baralgin - according to Karpov's reference book, it is compatible, but its composition - Metamizole sodium + Pitophenone + Fenpiverinium bromide could not be verified using other reference books (they are not there, apparently, this drug is used only here).
48.menovazine – I found several different menovazines in composition. 1. Benzocaine* + Procaine + Racementhol. 2. racemic menthol + novocaine + anesthesin for the first - I found no contraindications, but procaine according to Hale L3 for the second - the only contraindications are hypersensitivity to novocaine.
49. sodium thiosulfate - the only contraindication to it is hypersensitivity to sodium thiosulfate. 50.sedalgin - use is not advisable for hepatitis B due to the combination of phenobarbital, codeine and caffeine. In addition, analgin is banned in many countries due to its toxicity. Ingredients: Paracetamol - compatible with HB Metamizole sodium (analgin) - according to e-lactancia - risk 1 Caffeine - Phenobarbital - causes sedation in a child Codeine phosphate - Caffeine can cause a reflux effect in a newborn. 51. caffetine = Codeine + Propyphenazone + Paracetamol + Caffeine Not compatible with giv, because Propyphenazone for e-lactation – risk 3 Alternative compatible with giv-ibuprofen
52. no-spa (drotaverine) - according to Karpov, compatible with lactation.
53. amegrinine according to Hale - according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale - L3
54. papazole = Papaverine + Bendazol (Papaverine + Bendazol) according to Karpov - papaverine and bendazole are compatible. but there are other drugs that WHO recommends for breastfeeding women with hypertension: Captopril, Methyldopa, Hydrochlorothiazide, Hydralazine, Nifedipine (the last two are best not used for a long time). 55. Capoten is compatible with E-lactation, risk 0, minimally excreted in milk. 56. enap(enalapril) for e-lactation - risk 0 according to Hale - L2, in the neonatal period - L4 according to Karpov - not compatible due to lack of data
57. analgin (metamizole sodium) - according to e-lactation - risk 1, it is advisable to replace it with paracetamol or ibuprofen 58. ketonal (Ketoprofen) - According to classification during pregnancy from the AAP (American Academy of Pediatrics) and during feeding from Dr. Hale it belongs to group L3 (relatively safe. Studies have shown the possibility of not very strong side effects for the child.) Thus. its use is not advisable. according to e-lactation - risk 0 59. corvalol - according to Karpov - compatible, but contains phenobarbital, which can cause sedation in the child.
Diclofenac is classified as L2 during pregnancy by the AAP (American Academy of Pediatrics) and while breastfeeding by Dr. Hale (safe. There are limited studies that have not shown a negative effect on infants AND/OR a negative effect is possible, but very unlikely.). For e-lactation - risk 0
Urolesan is a herbal preparation. the instructions say “Data on the use of the drug during pregnancy and breastfeeding are not provided.” But the hops and mint included in the composition reduce lactation. More information about peppermint - relaxes esophagogastric reflux - can aggravate reflux.
phytolysin is compatible with breastfeeding according to the instructions, but be careful with it: it contains sage and mint, which can negatively affect lactation.
Relief is compatible with Guards.
Levomycetin (Chloramphenicol*) - is not compatible with breastfeeding according to Russian reference books, and according to the classification during pregnancy from the AAP (American Academy of Pediatrics) and when breastfeeding from Dr. Hale L4 - possibly dangerous. Studies in breastfeeding women have shown an increased risk to the baby, but use may be justified by a threat to the mother's life.
Nalpaza-Pantoprazole* (Pantoprazole*) with risk 1 - relatively safe: side effects are possible in a child, but they are rare and not very strong. According to the Russian reference book, there are none.
Ketonal during lactation
According to the instructions, Ketonal should not be used during breastfeeding. This is explained by the fact that the components of the medication are absorbed into the mother’s bloodstream and, together with breast milk, enter the newborn’s body. These substances accumulate in the baby’s organs and disrupt their functioning.
Ketonal can be used once if absolutely necessary. It is strongly recommended to skip 1 feeding to avoid dangerous phenomena.
Thus, Ketonal is prohibited during lactation, since the drug negatively affects the newborn.
For a single use, put the baby to the breast 3 hours after using the analgesic. Subscribe to our VKontakte group
Antipyretics during breastfeeding
09.09.2021
Women, when they learn about their “interesting” situation, and after the birth of a child, begin to be much more anxious
treat your health. In essence, there is nothing surprising in this - now they are responsible for small
a defenseless creature that is affected by any changes in the mother’s health. Therefore, as soon as they appear
Some signs of illness in the mother, this immediately causes panic.
The most common phenomenon during lactation is fever in a nursing mother. Previously, in such cases, the baby
She was immediately weaned off the breast and isolated from her mother until her complete recovery. In fact, this tactic is not correct,
especially in the first months of a child’s life. The later you switch your baby to artificial complementary feeding, the better, because
Mother's milk contains everything a baby needs.
If you have a fever, do not panic. First of all, it is worth understanding what caused its increase.
Most often they are seasonal viral infections, milk stagnation (lactostasis), poisoning, mastitis (inflammation of the mammary gland ),
as well as various possible other infections and inflammations. Each of these ailments has its own symptoms and signs, and in order to
In order not to confuse one with the other, understand this thoroughly. For example, ARVI is characterized mainly by a runny nose , sore throat and
/or dry cough, general weakness of the body, possible enlargement of lymph nodes. Lactostasis is characterized by the appearance of compactions
in the chest , which can be felt, and pain in these places, redness of the skin of the chest , low blood pressure and general weakness.
Mastitis is accompanied by the same symptoms as lactostasis, but other symptoms of mastitis will help to distinguish one from the other: very high
temperature (above 39 degrees), the formation of soft areas the chest the chest , indentations may remain in it.
We believe you are already familiar with the signs of poisoning. Here, in addition to the elevated temperature, nausea and vomiting, abdominal , diarrhea ,
headache, pale skin, drowsiness, fainting, etc.
The above symptoms will help you narrow down your suspicions, but in order to accurately determine the disease, you need to consult a specialist.
Only he has the right to prescribe treatment methods for you. Be sure to tell your doctor that you are breastfeeding : then he will be guided by what
to prescribe you the most harmless drugs possible.
However, if the temperature is already quite high, and there is no time to wait for the doctor , you need to know what medications can be taken during the period
lactation, and which ones are best to abstain from. We strongly do not recommend taking acetylsalicylic acid or aspirin - in children, and especially
in such small children, it can cause a very dangerous reaction, sometimes even fatal. Worthy substitutes for this antipyretic
are ibuprofen and paracetamol. Both of these medicinal substances are not only sold under their own name, but are also included in many
other antipyretics. Based on paracetamol, for example, you can buy Panadol and Tylenol at the pharmacy, and based on ibuprofen -
Advil, Brufen and Nurofen. Both paracetamol and ibuprofen also have analgesic and anti-inflammatory properties.
During breastfeeding you need to be especially vigilant with the dosage. Any antipyretic should be taken no more than 4 times a day, 1 tablet.
The course of such treatment should be minimal - no more than 3 days. If during this period the temperature has not completely subsided, it is necessary to undergo a second
examination: perhaps the cause of the elevated temperature is different than what the doctor , and the treatment is also necessary differently. Not worth it for a long time
time to “sit” on the above-mentioned paracetamol and ibuprofen: in large quantities they negatively affect liver .
If the temperature does not rise much - up to 38-38. 5 degrees - then you can try to “bring it down” with folk remedies. The simplest and most accessible means
lowering the temperature is honey - dilute 1 tbsp in a glass of warm water. l. honey Infusions of cranberries, lingonberries, and raspberries help well. Also reduces well
temperature and nettle: pour a tablespoon of dried nettle leaves with a glass of boiling water, and leave (preferably in a thermos so that the water does not cool) for an hour.
Take this medicinal drink 4 times a day – you will definitely feel better.
Published in Pregnancy and pregnancy management Premium Clinic